1. Introduction
Blood clots, while essential to healing wounds, can also pose a severe threat to health when they form inappropriately. In the context of health, blood clots can become a silent killer, leading to life-threatening conditions such as strokes, heart attacks, and pulmonary embolisms. Given their potential to cause sudden and severe complications, it's critical to recognize the signs, understand the causes, and be aware of the associated risks.
A blood clot forms when blood turns from a liquid to a gel-like state, a natural response to injury to prevent excessive bleeding. However, when clots form within the bloodstream without a necessary trigger, they can block blood flow to vital organs, leading to critical health issues. This underscores the importance of being vigilant about symptoms, knowing the causes, and understanding the risk factors, so that individuals can take charge of their health and seek timely medical intervention.
Awareness can be a lifesaver when it comes to blood clots. Whether you’re at risk due to lifestyle factors, genetic predispositions, or medical conditions, understanding this health issue is key. Educating yourself on how blood clots form, the warning signs to watch for, and the treatment options available can help you stay informed and prepared. By doing so, you can play an active role in protecting yourself from potentially life-threatening complications. This article will explore everything you need to know about blood clots, from their formation to how they can be treated or prevented.
2. Understanding Blood Clots
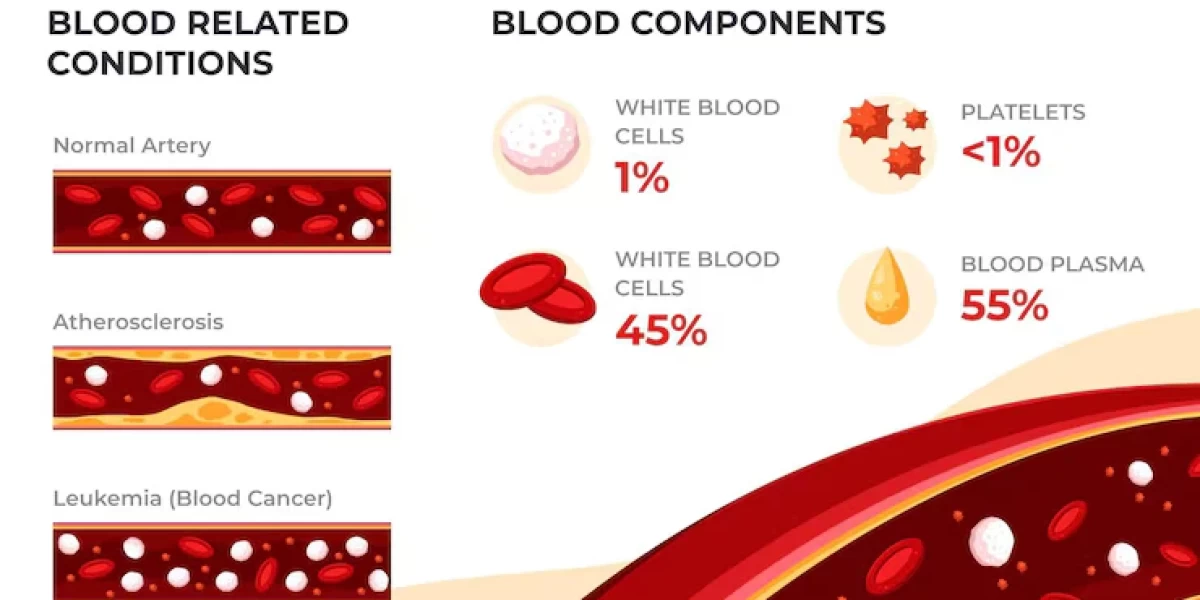
Blood clots are natural formations that occur when blood thickens and forms a semi-solid mass. This is part of the body’s defense mechanism, especially in cases of injury. When you get a cut or a bruise, blood clots work to stop the bleeding by sealing the wound and allowing tissue repair to begin. In this sense, blood clotting is a vital process for healing and recovery.
However, not all blood clots are beneficial. Clotting becomes dangerous when it happens in the wrong place or at the wrong time, such as in an artery or vein where blood flow is meant to remain fluid. Harmful blood clots can lead to blockages in blood vessels, preventing oxygen-rich blood from reaching organs and tissues. This can result in conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), or even a stroke.
The body’s clotting system is designed to balance between clot formation and breakdown. Under normal circumstances, the body knows when to form a clot and when to dissolve it. But when this process is disrupted, clots can form unnecessarily and fail to dissolve, leading to dangerous outcomes. This is where awareness becomes crucial, as understanding when a clot is beneficial versus when it is harmful could potentially save lives.
There are two main types of harmful clots: arterial clots and venous clots. Arterial clots form in the arteries, which carry blood away from the heart to the rest of the body. These clots can lead to strokes or heart attacks by cutting off the blood supply to the brain or heart. On the other hand, venous clots form in the veins, which carry blood back to the heart. One of the most common and dangerous types of venous clots is deep vein thrombosis (DVT), often occurring in the legs. If a portion of this clot breaks off and travels to the lungs, it can cause a pulmonary embolism, a life-threatening condition.
Thus, while blood clots are essential to healing, they become harmful when they occur without injury or fail to break down as intended. Knowing the difference between normal clotting and harmful clot formation can help individuals recognize when to seek medical attention, potentially preventing severe health outcomes.

3. Symptoms of Blood Clots
Blood clots, also known as thrombi, can develop in various parts of the body and cause significant health issues if not detected early. Recognizing the symptoms of blood clots is crucial to prevent complications such as pulmonary embolism or stroke. Some of the usual symptoms are:
-
Swelling: One of the hallmark signs of a blood clot is swelling, especially in the legs or arms. This swelling, known as edema, occurs when blood flow is blocked by the clot, causing fluid to build up in the affected area. The swelling is often localized, meaning it typically appears in one leg or arm rather than both. It may feel warm upon contact.
-
Pain or Tenderness: Pain in the area where the blood clot has formed is another common symptom. This pain can range from mild to severe and is often described as throbbing or cramping. The pain may worsen when walking or standing for prolonged periods, particularly in the calf or thigh if the clot is in the leg (known as deep vein thrombosis or DVT).
-
Discoloration of the Skin: The skin around the clot may appear reddish or bluish and can look different from the rest of the surrounding area. This discoloration is caused by restricted blood flow, which affects oxygen delivery to the tissues. In some cases, the skin may also feel warm or tender to the touch.
-
Shortness of Breath: If a blood clot travels to the lungs, it can cause pulmonary embolism, which is a life-threatening condition. Symptoms include sudden shortness of breath, chest pain (which can mimic a heart attack), rapid heartbeat, and sometimes coughing up blood.
-
Fatigue and Dizziness: Blood clots in major arteries can reduce the oxygen supply to vital organs, leading to symptoms like unexplained fatigue, dizziness, or fainting. These symptoms can be easy to dismiss but should be taken seriously, especially if combined with other signs of a clot.
Recognizing these early symptoms is essential because timely medical intervention can prevent a blood clot from becoming more dangerous. Ignoring or delaying treatment could result in severe complications, including heart attack, stroke, or long-term damage to the veins and tissues.
4. Causes of Blood Clots
Blood clots can form due to a variety of causes, many of which are preventable or manageable. Understanding these causes is critical for reducing the risk of developing clots in the first place. Here are some of the most common causes of blood clots:
-
Prolonged Immobility: One of the leading causes of blood clots is extended periods of immobility, such as during long flights, car rides, or bed rest after surgery. When you're immobile for long stretches, blood flow slows down, particularly in the lower extremities, creating an environment conducive to clot formation.
-
Medical Conditions: Certain health conditions increase the risk of blood clots. For instance, cancer and chemotherapy can make the blood more prone to clotting. Additionally, conditions like heart disease, diabetes, and inflammatory bowel disease (IBD) are also associated with higher clotting risks. Atrial fibrillation, a type of irregular heartbeat, can lead to blood pooling in the heart, increasing the risk of stroke-causing clots.
-
Surgery or Trauma: Surgery, particularly orthopedic surgeries like hip or knee replacements, increases the risk of developing blood clots. Trauma to the blood vessels during surgery or accidents can also lead to clot formation. Post-surgical patients are often prescribed anticoagulant medications to prevent clots.
-
Hormonal Changes: Hormonal contraceptives and hormone replacement therapy (HRT) can increase the likelihood of clot formation by altering the balance of clotting factors in the blood. Additionally, pregnancy is a known risk factor due to increased pressure on the veins in the pelvis and legs.
-
Lifestyle Factors: Smoking, obesity, and a sedentary lifestyle contribute significantly to blood clot formation. Smoking damages the lining of the blood vessels, which can promote clot formation, while obesity puts additional strain on the circulatory system. A lack of regular physical activity can also slow blood flow, particularly in the lower limbs, where clots often form.
Addressing these causes involves a combination of lifestyle changes and medical interventions. Staying active, maintaining a healthy weight, and quitting smoking can significantly reduce the risk of developing blood clots. In some cases, taking blood-thinning medications or wearing compression stockings may be necessary to prevent clot formation, especially for individuals with higher risk factors.

5. Risks Associated with Blood Clots
Certain risk factors can increase an individual's likelihood of developing blood clots. Understanding these risks is vital for prevention and early detection. Here are some of the primary risk factors associated with blood clots:
-
Age: Blood clots become more common as people age, particularly after the age of 60. This is largely due to a slowing circulatory system and the higher likelihood of having underlying health conditions that can lead to clotting.
-
Obesity: Being overweight or obese significantly increases the risk of blood clots, particularly in the legs. Extra weight puts pressure on the veins, slowing blood flow and making clots more likely to form.
-
Genetic Predispositions: Some people are born with genetic conditions that make their blood more likely to clot. For instance, Factor V Leiden is a genetic mutation that increases the likelihood of blood clot formation. If you have a family history of blood clots, your risk may be higher.
-
Sedentary Lifestyle: A lack of physical activity slows down circulation, especially in the legs. Prolonged periods of sitting or lying down, particularly after surgery or during long travel, can lead to blood clots forming in the deep veins, known as deep vein thrombosis (DVT).
-
Pregnancy and Postpartum: During pregnancy, increased hormone levels and pressure on the veins in the pelvis can lead to blood clots. The risk remains elevated for several weeks after giving birth, especially if there were complications during delivery or a C-section.
-
Previous History of Blood Clots: Individuals who have experienced a blood clot in the past are at greater risk of developing another one. Preventative measures, such as blood-thinning medications, are often prescribed to mitigate this risk.
Understanding these risk factors can help individuals take proactive steps to reduce their likelihood of developing blood clots. This may involve lifestyle adjustments, medical screenings, and close monitoring, particularly for those at higher risk due to genetic or medical factors.
6. Treatment Options for Blood Clots
When a blood clot is diagnosed, timely treatment is critical to prevent serious complications like pulmonary embolism or stroke. The treatment for blood clots typically depends on the location of the clot, the individual's overall health, and the severity of the clot. Here are some common treatment options:
-
Medications:
- Anticoagulants: Also known as blood thinners, anticoagulants such as warfarin, heparin, or newer drugs like rivaroxaban are commonly prescribed to prevent the clot from growing and to reduce the risk of new clots forming. These medications do not dissolve existing clots but help prevent further complications.
- Thrombolytics: In more severe cases, especially with life-threatening clots such as pulmonary embolisms, thrombolytic therapy may be used. These medications, sometimes referred to as clot-busters, help dissolve the clot but come with a higher risk of bleeding.
-
Compression Stockings: For patients with deep vein thrombosis (DVT), compression stockings are often recommended to improve blood flow in the legs and prevent swelling and complications such as post-thrombotic syndrome, which can lead to long-term pain and swelling.
-
Surgical Intervention: In rare cases where blood clots are life-threatening or do not respond to medications, surgery may be required. This can include procedures like thrombectomy, where the clot is physically removed from the blood vessel.
-
Lifestyle Changes: Patients recovering from blood clots are often advised to adopt lifestyle changes to prevent future occurrences. This can include regular physical activity, maintaining a healthy weight, and quitting smoking. Elevating the legs and staying hydrated during long periods of inactivity (such as flights or bed rest) can also help reduce the risk of clot formation.
The key to effective treatment is early diagnosis and intervention. If blood clots are detected early, treatment can prevent the clot from becoming more dangerous. In some cases, long-term use of blood thinners or other preventative measures may be necessary to reduce the risk of future clots.
7. Prevention Strategies
Blood clots, also known as deep vein thrombosis (DVT), are a serious medical condition that can lead to life-threatening complications, such as pulmonary embolism. While blood clots can sometimes form due to genetic factors or underlying health conditions, many are preventable through lifestyle changes. The following actionable tips can help reduce the risk of developing blood clots and improve overall circulation.
One of the most effective prevention strategies is regular exercise. Physical activity promotes healthy blood circulation, helping to prevent blood from pooling in the veins, which is a common cause of clot formation. Even moderate exercises like walking, swimming, or cycling for at least 30 minutes a day can significantly reduce your risk. If you have a sedentary job or spend long hours sitting, it's essential to take short breaks every hour to move around and stretch, as prolonged immobility is a key risk factor for clots.
Maintaining a healthy weight is another critical element in preventing blood clots. Obesity puts extra pressure on your veins, making it harder for blood to circulate efficiently. This increased pressure can lead to clot formation, especially in the legs. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains not only helps with weight management but also improves overall vascular health.
Staying hydrated is an often-overlooked strategy but plays a crucial role in preventing clots. Dehydration may lead to blood thickening, raising the chance of clot formation. Drinking enough water throughout the day keeps your blood flowing smoothly and reduces the risk of thickening. Aim for at least 8 glasses of water per day, and even more if you're exercising or living in a hot climate.
Another important preventive measure is avoiding smoking. Smoking damages the blood vessels and increases the risk of clotting by making blood more likely to clot. Quitting smoking can dramatically improve vascular health and lower your risk of DVT.
Finally, it's essential to follow any medical advice you receive regarding blood clot prevention, especially if you have a family history of clotting disorders or have undergone recent surgery. Medications like blood thinners may be prescribed to reduce your risk, and following your doctor's instructions is key to preventing complications.
Incorporating these prevention strategies into your daily routine can help you stay healthy and avoid the serious consequences of blood clots. Remember, small lifestyle changes can have a big impact on your long-term health.
8. When to Seek Medical Help
Recognizing the warning signs of a blood clot and seeking prompt medical attention can be lifesaving. While not all blood clots present obvious symptoms, there are key indicators you should never ignore.
Pain and swelling, particularly in the legs, are among the most common symptoms of a deep vein thrombosis. If you experience unexplained swelling, tenderness, or pain in one leg, especially if it feels warm to the touch, it's essential to seek medical help immediately. Blood clots can also cause discoloration of the skin in the affected area, which may appear red or blueish.
Another alarming symptom of a blood clot is shortness of breath. This may indicate that the clot has traveled to your lungs, resulting in a pulmonary embolism, which is a medical emergency. Other symptoms of a pulmonary embolism include sharp chest pain, rapid heart rate, coughing (sometimes with blood), and dizziness. These signs should never be ignored, as untreated pulmonary embolisms can be fatal.
Less common but still important symptoms include unexplained headaches or vision changes, which may suggest a clot in the brain. Blood clots can also form in the arms, abdomen, or other parts of the body, so it's important to be aware of any unusual or sudden pain.
If you suspect you have a blood clot, it's critical not to wait or self-diagnose. Immediate medical evaluation is necessary, as early detection and treatment greatly reduce the risk of serious complications. Blood clots can be treated with anticoagulant medications, which help to dissolve the clot or prevent it from growing larger. In more severe cases, surgical intervention may be needed to remove the clot.
Remember, time is of the essence when it comes to treating blood clots. If you or someone you know is experiencing any of the symptoms described, seek medical attention as soon as possible to ensure a safe outcome.
9. Living with Blood Clots
For individuals who have experienced a blood clot, managing the condition and preventing recurrence becomes a critical part of daily life. While living with a history of blood clots requires ongoing attention, it is possible to lead a healthy and active life by adopting the right strategies and mindset.
One of the most important aspects of managing blood clots is adhering to prescribed medications. Blood thinners or anticoagulants are commonly prescribed to reduce the risk of future clots. These medications help keep your blood at the right consistency to prevent clotting, but they also require regular monitoring by your healthcare provider. You may need periodic blood tests to ensure the medication is working effectively and that your dosage is correct.
In addition to medication, making lifestyle adjustments is key to reducing the risk of recurrence. Staying active and avoiding long periods of immobility are crucial for improving circulation. If you've had a clot in the past, your doctor may recommend wearing compression stockings, which help promote blood flow in the legs and reduce the risk of clotting. These stockings are particularly helpful for individuals who have to stand or sit for extended periods.
Maintaining a healthy diet and staying hydrated are just as important in managing life with a history of blood clots as they are in prevention. Reducing salt intake, eating heart-healthy foods, and avoiding excess alcohol can all contribute to better vascular health. If you're overweight, working with a healthcare professional to develop a plan for gradual weight loss can reduce strain on your veins and further lower your risk.
It's also essential to be aware of any new symptoms that may indicate a potential recurrence of blood clots. If you notice pain, swelling, or any of the other symptoms mentioned earlier, seek medical attention promptly. Early action can prevent issues and assist in managing the condition more efficiently.
Lastly, don't hesitate to seek support. Living with blood clots can be stressful, and connecting with others who share similar experiences can provide emotional relief and valuable insights. Support groups, whether online or in-person, offer a community of individuals who understand the challenges of managing this condition.
10. Conclusion
Blood clots are a serious health concern, but with the right knowledge and proactive steps, they can often be prevented or effectively managed. Whether you're focusing on prevention through regular exercise, healthy eating, and staying hydrated, or managing life with a history of clots through medication and lifestyle changes, taking control of your health is essential.
Recognizing the symptoms of a blood clot and knowing when to seek medical help can save lives. Awareness, early detection, and proper treatment are key to preventing serious complications like pulmonary embolism. Living with blood clots may require adjustments, but with the right resources and support, it's possible to lead a healthy and fulfilling life.
Frequently Asked Questions(FAQ's)
- What causes the risk of blood clots? Blood clots can form due to factors like prolonged inactivity, injury to a blood vessel, smoking, certain medications, and underlying health conditions such as heart arrhythmia, obesity, and cancer.
- What is the best treatment for blood clots? Treatment options include anticoagulant medications (blood thinners) like warfarin and heparin, thrombolytic medications to dissolve clots, and catheter-directed treatments. Always consult a healthcare provider for the best treatment plan.
- What are the symptoms of blood clots? Symptoms can include swelling, pain, redness, warmth in the affected area, shortness of breath, chest pain, and dizziness.
- What is the treatment for blood clotting problems? Treatment typically involves anticoagulant medications, lifestyle changes, and addressing any underlying conditions.
- How to remove blood clots naturally? Natural methods include staying hydrated, exercising regularly, and consuming foods like garlic, ginger, and turmeric.
- What food to avoid for a blood clot? Avoid refined and processed foods, sugary drinks, trans fats, and red and processed meats.
- Which fruit is good for blood clots? Fruits like pineapple (rich in bromelain) and kiwi are known to help reduce the risk of blood clots.
- What is the best drink for blood clots? Drinking plenty of water is essential. Herbal teas like green tea and ginger tea can also be beneficial.
- What reduces the risk of blood clots? Maintaining a healthy lifestyle with regular exercise, a balanced diet, staying hydrated, and avoiding smoking can help reduce the risk of blood clots.