Introduction
Diabetes, a chronic condition affecting millions worldwide, arises when the body cannot regulate blood sugar levels effectively. This inability can lead to long-term complications, impacting organs, blood vessels, and nerves. One of the lesser-known but critical complications linked to diabetes is the risk of seizures, which can stem from fluctuations in blood sugar levels or other diabetes-related factors. Understanding the symptoms, causes, and treatments for seizures in individuals with diabetes is essential for managing both conditions effectively and improving quality of life. By increasing awareness, individuals and caregivers can take proactive steps to prevent and address these potentially life-threatening events. Diabetes and Seizures
Understanding Diabetes
Diabetes is a metabolic disorder characterized by chronic hyperglycemia, or high blood sugar levels, resulting from either insufficient insulin production, impaired insulin action, or both. The condition is primarily classified into three main types:
-
Type 1 Diabetes: An autoimmune disorder where the body's immune system attacks insulin-producing beta cells in the pancreas. This type typically develops during childhood or adolescence and requires lifelong insulin therapy.
-
Type 2 Diabetes: A more common form linked to insulin resistance and often associated with lifestyle factors such as obesity and physical inactivity. It typically develops in adulthood but is increasingly seen in younger populations due to rising rates of childhood obesity.
-
Gestational Diabetes: Develops during pregnancy when hormonal shifts hinder the body's insulin efficiency. Though it often subsides after giving birth, it heightens the risk of future Type 2 diabetes.
Diabetes impacts the body by causing fluctuating glucose levels, leading to damage in multiple systems over time. Proper blood sugar regulation is critical, as persistently high levels (hyperglycemia) or low levels (hypoglycemia) can result in severe complications. High blood sugar damages nerves and blood vessels, while low blood sugar, often a side effect of diabetes medication, can directly trigger seizures. Hence, understanding diabetes management, including medication, diet, and lifestyle interventions, is vital for mitigating associated risks, including seizures. Diabetes and Seizures

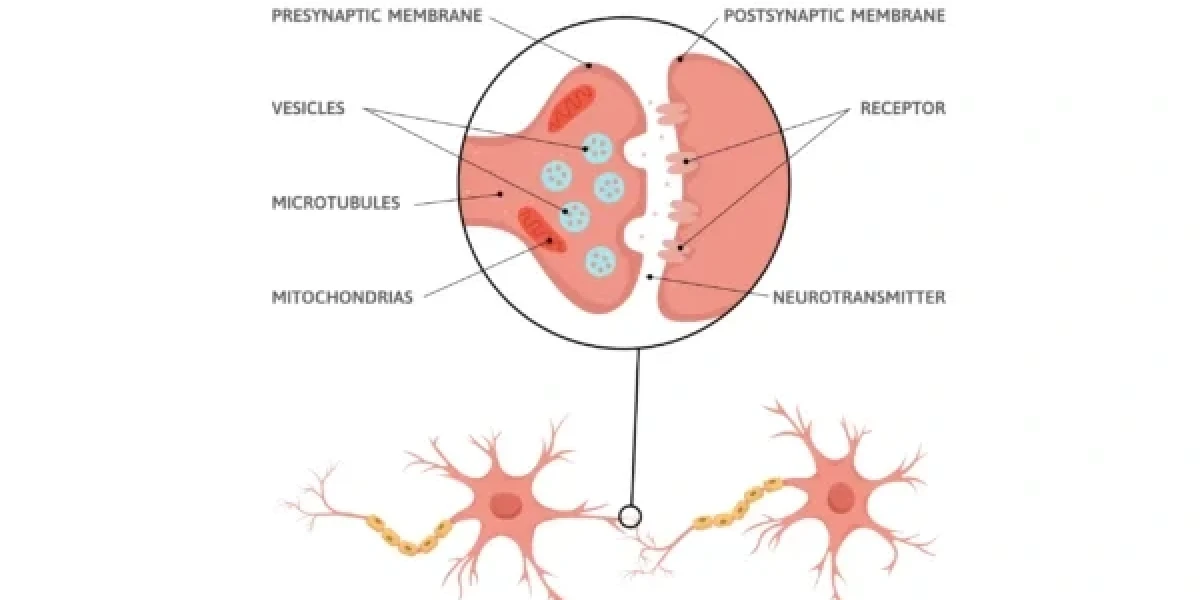
The Link Between Diabetes and Seizures
The relationship between diabetes and seizures is rooted in the delicate balance required to maintain stable blood sugar levels. When blood sugar drops too low (hypoglycemia) or rises too high (hyperglycemia), it can disrupt normal brain function, potentially triggering seizure activity. Hypoglycemia, in particular, is a leading cause of seizures in diabetic patients. This occurs when the brain is deprived of sufficient glucose, its primary energy source, resulting in abnormal electrical activity that manifests as a seizure. Diabetes and Seizures
On the other hand, hyperglycemia can also cause seizures, albeit through different mechanisms. Prolonged high blood sugar levels may lead to a rare but severe condition known as nonketotic hyperosmolar hyperglycemia. This state causes significant dehydration and electrolyte imbalances, which can disrupt neuronal function and lead to seizures. Furthermore, diabetes-related complications such as neuropathy, kidney dysfunction, and medication side effects may increase susceptibility to seizures.
Another aspect to consider is the role of insulin therapy and other diabetes medications. While these treatments are essential for managing blood sugar, incorrect dosing or timing can lead to sudden drops in glucose levels, heightening the risk of hypoglycemic seizures. Thus, effective diabetes management requires precise monitoring of blood sugar levels and awareness of symptoms that could indicate an impending seizure. Understanding these mechanisms not only highlights the intricate link between diabetes and seizures but also underscores the importance of early intervention and preventative care.
Symptoms of Seizures in Diabetic Patients
Recognizing the symptoms of seizures in diabetic patients is crucial for timely intervention. Generalized seizures, such as tonic-clonic seizures, are characterized by sudden loss of consciousness, convulsions, and muscle stiffness. However, in diabetic individuals, the symptoms can sometimes overlap with or be masked by signs of a hypoglycemic episode, complicating diagnosis and treatment.
Common symptoms of seizures in diabetic patients include:
- Loss of Consciousness: A hallmark of generalized seizures, this may occur suddenly and without warning.
- Involuntary Movements: Uncontrolled jerking or twitching of muscles, particularly in the arms and legs.
- Confusion or Disorientation: Following a seizure, individuals may feel disoriented, confused, or experience memory lapses (known as the postictal state).
In addition to these generalized symptoms, hypoglycemic episodes in diabetics may present unique warning signs:
- Sweating
- Shakiness or Tremors
- Hunger
- Rapid Heartbeat
- Behavioral Changes: Irritability, aggression, or anxiety, which may precede a seizure if hypoglycemia worsens.
Hyperglycemia-induced seizures, though less common, can be preceded by symptoms like extreme thirst, frequent urination, and dehydration. In both cases, the severity and progression of symptoms depend on how quickly blood sugar levels are corrected.
Identifying these symptoms promptly can help prevent severe complications. For caregivers, understanding the distinct and overlapping signs of seizures and diabetes-related episodes is vital for ensuring the safety and well-being of diabetic individuals at risk of seizure activity. Diabetes and Seizures
Causes of Seizures in Diabetic Patients
Seizures in individuals with diabetes can arise from a range of factors directly or indirectly related to the condition. The two most common triggers are extremes in blood sugar levels—hypoglycemia and hyperglycemia. Both can disrupt normal brain function, leading to abnormal electrical activity that manifests as seizures.
-
Hypoglycemia: This is the leading cause of seizures in diabetic patients. Hypoglycemia occurs when blood glucose levels drop below 70 mg/dL, depriving the brain of its primary energy source. Common causes include missed meals, excessive insulin doses, or intense physical activity. Severe hypoglycemia can result in neuroglycopenia, a state where the brain cannot function properly, triggering seizures.
-
Hyperglycemia: Although less frequent than hypoglycemia-induced seizures, prolonged high blood sugar levels can also cause seizures. Hyperglycemia may lead to a condition called nonketotic hyperosmolar hyperglycemia, where severe dehydration and electrolyte imbalances disrupt normal neuronal function. This condition primarily affects older adults and those with poorly controlled diabetes.
-
Medication Mismanagement: Incorrect insulin dosing or improper use of diabetes medications can cause rapid fluctuations in blood sugar levels, increasing the risk of seizures. Medications for co-existing conditions, such as anti-hypertensives, may also interact with diabetes treatments, indirectly contributing to seizure risks.
-
Diabetic Complications: Chronic diabetes complications, such as diabetic neuropathy and kidney disease, can heighten seizure susceptibility. Renal dysfunction, in particular, may cause toxin buildup in the blood, affecting brain function and potentially triggering seizures. Diabetes and Seizures
-
Additional Triggers: Stress, infections, alcohol consumption, or sleep deprivation can exacerbate existing vulnerabilities in diabetic individuals, further increasing the likelihood of seizure episodes.
Understanding the diverse causes of seizures in diabetic patients highlights the critical need for vigilant blood sugar management and awareness of potential triggers. Proactive prevention strategies can significantly reduce the risk of seizures and associated complications.
Diagnosis of Seizures in Diabetic Patients
Diagnosing seizures in diabetic patients requires a comprehensive approach to identify the underlying cause and ensure appropriate treatment. The process involves gathering a detailed medical history, conducting physical and neurological examinations, and employing diagnostic tests to confirm the seizure's nature and origin. Diabetes and Seizures
-
Medical History: Physicians begin by reviewing the patient’s history of diabetes management, recent blood sugar fluctuations, and previous seizure episodes. Information about lifestyle habits, medication adherence, and family history of seizures or neurological conditions is also crucial.
-
Physical Examination: A thorough physical and neurological exam assesses the patient’s overall health, signs of injury from recent seizures, and any indications of underlying complications like neuropathy or dehydration.
-
Blood Tests: Laboratory tests play a vital role in identifying potential triggers. Blood glucose levels are measured to determine if hypoglycemia or hyperglycemia is involved. Additional tests, such as electrolyte panels and kidney function tests, may be conducted to rule out other contributing factors.
-
Electroencephalogram (EEG): An EEG records electrical activity in the brain, helping to confirm seizure activity and distinguish it from other neurological conditions. Abnormal patterns in brain waves can indicate specific seizure types and guide treatment.
-
Imaging Studies: In some cases, imaging techniques like MRI or CT scans are used to detect structural abnormalities, such as brain lesions, that may contribute to seizures.
Accurate diagnosis is essential for tailoring treatment strategies and addressing the root causes of seizures in diabetic patients. By combining medical expertise with advanced diagnostic tools, healthcare providers can help diabetic individuals manage their conditions effectively and reduce the risk of seizure recurrence. Diabetes and Seizures
Treatment Options for Seizures in Diabetic Patients
Effectively treating seizures in diabetic patients requires a comprehensive approach that addresses both the immediate seizure episode and the underlying diabetes-related triggers. Treatment options include pharmacological interventions, non-pharmacological strategies, and careful management of diabetes to minimize future risks. Diabetes and Seizures
-
Pharmacological Treatments:
Anticonvulsant medications are commonly prescribed to control seizure activity. Drugs such as levetiracetam, lamotrigine, or valproate may be used depending on the type of seizures and the patient’s overall health. In diabetic patients, it is crucial to select anticonvulsants that do not negatively interact with diabetes medications or exacerbate blood sugar fluctuations. Diabetes and Seizures
If hypoglycemia is the trigger, immediate treatment involves administering fast-acting carbohydrates, such as glucose tablets or sugary drinks, to restore blood sugar levels. Severe instances may necessitate intravenous glucose or glucagon injections. For hyperglycemia-related seizures, correcting blood sugar levels with insulin and rehydration therapy is essential.
-
Dietary Adjustments:
A well-balanced diet tailored to stabilize blood sugar levels plays a significant role in preventing seizures. Incorporating complex carbohydrates, lean proteins, and healthy fats can help maintain steady glucose levels throughout the day. Diabetic patients prone to seizures may benefit from consulting a dietitian for personalized meal planning.
-
Lifestyle Modifications:
Regular physical activity, adequate sleep, and stress management are critical for overall health and seizure prevention. However, exercise routines should be planned carefully to avoid hypoglycemia, especially in patients on insulin therapy. Patients are encouraged to monitor their blood sugar levels before and after exercise.
-
Patient Education and Support:
Empowering patients with knowledge about their condition is essential. Learning to recognize early signs of hypoglycemia, understanding proper medication usage, and knowing how to respond to a seizure can significantly improve outcomes. Support groups and counseling may also help patients manage the emotional stress associated with living with diabetes and seizures.
A combination of these treatment strategies ensures a holistic approach to managing seizures in diabetic individuals, improving their quality of life and reducing recurrence risks.
Prevention Strategies
Prevention is the cornerstone of reducing seizure risks in diabetic patients. By adopting proactive measures and adhering to diabetes management plans, individuals can effectively lower the likelihood of seizure episodes. Diabetes and Seizures
-
Regular Blood Sugar Monitoring:
Frequent blood sugar checks are vital to detect and address fluctuations before they lead to complications. Advanced glucose monitoring systems, such as continuous glucose monitors (CGMs), provide real-time data, enabling better control.
-
Medication Adherence:
Consistently taking prescribed medications at the correct dosage and times is crucial. Patients should work closely with their healthcare provider to adjust insulin or other treatments as needed to avoid extreme highs or lows in blood sugar.
-
Balanced Diet and Hydration:
Following a diabetes-friendly diet helps maintain stable glucose levels. Eating small, regular meals, avoiding excessive sugar, and staying hydrated are essential steps in preventing hypoglycemia and hyperglycemia.
-
Lifestyle Choices:
Incorporating exercise into daily routines can improve insulin sensitivity and glucose control. However, exercising responsibly—monitoring blood sugar levels and carrying quick sources of glucose—is essential. Additionally, avoiding alcohol and ensuring sufficient sleep are critical for maintaining brain and overall health.
-
Recognizing and Addressing Triggers:
Identifying patterns or activities that precede seizures, such as stress or missed meals, allows for better preparation and prevention. For example, managing stress through mindfulness or therapy can help mitigate seizure risks.
-
Emergency Preparedness:
Diabetic patients should always carry a medical alert bracelet and a supply of fast-acting glucose. Family members and caregivers must be educated on recognizing seizures and providing first aid.
By combining these prevention strategies with effective diabetes management, patients can significantly reduce the risk of seizures and enjoy a healthier, more stable life.
Living with Diabetes and Seizures
Managing both diabetes and seizures presents unique challenges, but with proper strategies, individuals can lead fulfilling lives. The key lies in adopting a proactive approach that emphasizes self-awareness, education, and robust support systems. Diabetes and Seizures
-
Building a Support System:
Living with chronic conditions like diabetes and seizures can be overwhelming without adequate support. Building a network of family, friends, healthcare providers, and community support groups can help individuals feel less isolated. Support groups provide a platform for sharing experiences, learning new coping mechanisms, and fostering a sense of community.
-
Education and Self-Management:
Understanding the intricacies of both diabetes and seizures is critical for effective self-management. Patients should educate themselves about the triggers, warning signs, and management techniques for both conditions. This includes recognizing early signs of hypoglycemia, tracking blood sugar levels, and knowing how to respond during a seizure. Regular consultations with healthcare professionals and attending workshops can enhance knowledge and confidence.
-
Coping Strategies:
Emotional well-being is an integral part of managing chronic illnesses. Stress, anxiety, and depression are common among individuals dealing with diabetes and seizures, but effective coping strategies can help. Mindfulness practices, such as meditation or yoga, can reduce stress levels and improve overall health. Therapy or counseling offers additional support, enabling individuals to navigate emotional challenges effectively.
-
Lifestyle Adaptations:
Adopting a lifestyle that prioritizes health and stability is essential. This includes adhering to a well-balanced diet, maintaining a consistent exercise routine, and ensuring adequate sleep. Creating routines for medication schedules, meal times, and physical activity can help maintain stable blood sugar levels and minimize seizure risks.
-
Emergency Preparedness:
Being prepared for emergencies provides peace of mind. Carrying a medical alert bracelet, emergency contact information, and supplies like glucose tablets or glucagon injectors ensures quick and effective responses during critical situations. Educating caregivers about seizure first aid and diabetes management further enhances safety. Diabetes and Seizures
By embracing these strategies, individuals can manage the complexities of living with diabetes and seizures while maintaining a high quality of life. A positive outlook and commitment to health empower patients to navigate their conditions with resilience and determination. Diabetes and Seizures
Conclusion
Diabetes and seizures are interconnected conditions that require diligent management and understanding. This guide has highlighted the importance of recognizing the relationship between fluctuating blood sugar levels and seizure activity, identifying symptoms, and addressing the root causes. From exploring effective treatments to implementing practical prevention strategies, every step contributes to better health outcomes.
Living with diabetes and seizures is undoubtedly challenging, but through education, support systems, and proactive lifestyle choices, individuals can thrive. Awareness of triggers, adherence to medication plans, and maintaining a balanced diet are key to minimizing risks. Additionally, fostering emotional well-being and preparedness for emergencies ensures a comprehensive approach to managing both conditions. Diabetes and Seizures
If you or a loved one is living with diabetes and seizures, seeking guidance from healthcare professionals is essential. They can provide tailored advice, create effective management plans, and offer support at every step of the journey. With the right knowledge, tools, and support, individuals can take control of their health and live fulfilling, stable lives.
Frequently Asked Questions(FAQs)
01. What causes seizures in diabetics?
Seizures in diabetics are primarily caused by extreme fluctuations in blood sugar levels. Hypoglycemia (low blood sugar) is the most common cause, but hyperglycemia (high blood sugar) can also lead to seizures.
02. Can you live a normal life with seizure medication?
Yes, many people with epilepsy or seizure disorders live normal, active lives while taking seizure medication. It's important to follow the prescribed treatment plan, monitor for side effects, and work closely with healthcare providers.
03. What is the difference between diabetic and epileptic seizures?
Diabetic seizures are caused by extreme blood sugar levels (either too high or too low), while epileptic seizures are due to abnormal electrical activity in the brain and are often recurrent.
04. What is the first aid treatment for diabetes?
First aid for diabetes involves monitoring blood sugar levels, administering insulin or glucose as needed, and seeking medical help if blood sugar levels are dangerously high or low.
05. What is the first treatment for diabetes?
The first treatment for diabetes typically involves lifestyle changes such as a healthy diet, regular exercise, and weight management, along with medications like metformin to control blood sugar levels.
06. What to do after a diabetic seizure?
After a diabetic seizure, it's important to check blood sugar levels, provide fast-acting carbohydrates if blood sugar is low, and seek medical attention if necessary.
07. What are the major causes of seizures?
Major causes of seizures include epilepsy, head injuries, infections, genetic factors, stroke, and metabolic imbalances like those seen in diabetes.
08. What food is good after a seizure?
After a seizure, it's good to consume simple carbohydrates like fruit juice or glucose tablets to quickly raise blood sugar levels if they were low.
09. What are 5 signs your blood sugar is too high?
Five signs of high blood sugar include frequent urination, increased thirst, blurred vision, fatigue, and headaches.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.