Diabetes is a multifaceted and widespread medical ailment that impacts millions of individuals globally. In this comprehensive guide, we will delve into the scientific aspects of diabetes, covering everything from its types and causes to managing the condition and the latest advancements in diabetes research.
Introduction
Diabetes, often referred to as diabetes mellitus, is a chronic disease characterized by elevated levels of blood sugar or glucose. The condition can have far-reaching effects on an individual's health and overall quality of life.
Types of Diabetes
Type 1 Diabetes
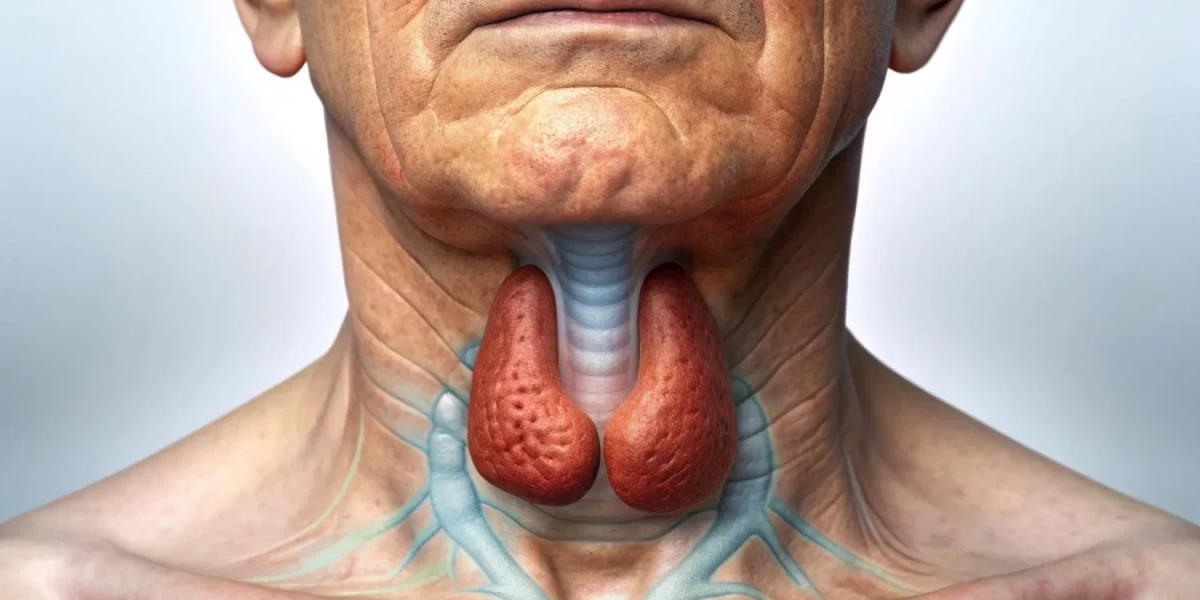
Type 1 diabetes is a chronic autoimmune condition in which the body's own immune system attacks and destroys the insulin-producing beta cells in the pancreas. Insulin is a hormone that helps glucose enter cells from the bloodstream and be used as energy. Without insulin, glucose builds up in the blood and can lead to serious health problems.
Type 1 diabetes can develop at any age, but it is most common in children and young adults. It is estimated that over 1.9 million Americans have type 1 diabetes, and about 40,000 new cases are diagnosed each year.
Type 2 Diabetes
Type 2 diabetes is a persistent ailment that impacts the way your body converts food into energy. Your body breaks down most of the food you eat into sugar (glucose), and then releases it into your bloodstream. When your blood glucose levels increase, a message is relayed to your pancreas to discharge insulin. Insulin acts like a key, unlocking the door to your cells so that glucose can get inside for energy.
With type 2 diabetes, either your body's cells resist the effects of insulin, or your pancreas doesn't produce enough insulin to meet your body's needs. Consequently, glucose accumulates in your bloodstream. Over time, elevated blood sugar levels can harm your nerves, blood vessels, and organs.
Gestational Diabetes
Gestational diabetes is a form of diabetes that emerges while a woman is pregnant. It affects about 2-10% of all pregnancies. Gestational diabetes typically resolves after childbirth, yet women with a history of gestational diabetes face an elevated likelihood of developing type 2 diabetes in the future.
Lifestyle elements that may elevate your susceptibility to type 2 diabetes encompass:
- Being overweight or obese
- Genetic predisposition to type 2 diabetes.
- Being physically inactive
- Eating a healthy diet
- Smoking
Genetic factors that can increase your risk of type 2 diabetes include:
- Having certain gene variants
- Having a racial or ethnic background that is at higher risk
Diabetes Risk Factors
There are a number of risk factors that can increase your risk of developing diabetes, including:
- Age: Your susceptibility to developing type 2 diabetes rises with advancing years.
- Family history: If you have a parent, brother, or sister with type 2 diabetes, you are at increased risk of developing the condition yourself.
- Race or ethnicity: People of certain races and ethnicities, such as African Americans, Hispanic Americans, Native Americans, and Asian Americans, are at increased risk of developing type 2 diabetes.
- Weight: Being overweight or obese is a major risk factor for type 2 diabetes.
- Physical inactivity: People who are not physically active are at increased risk of developing type 2 diabetes.
- Diet: Eating a diet that is high in processed foods, sugary drinks, and unhealthy fats can increase your risk of developing type 2 diabetes.
- High blood pressure: Elevated blood pressure may raise your likelihood of developing type 2 diabetes.
- High cholesterol: Having high cholesterol levels can increase your risk of developing type 2 diabetes.
- Polycystic ovary syndrome (PCOS): PCOS is a hormonal disorder that can cause a number of health problems, including type 2 diabetes.
- Gestational diabetes: Gestational diabetes is a form of diabetes that can emerge during pregnancy. Women with gestational diabetes face an elevated likelihood of developing type 2 diabetes in the future.
Symptoms of Diabetes
Diabetes is a long-term medical condition that impacts the way your body processes food to produce energy. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disorder where your immune system targets and eradicates the insulin-producing cells in your pancreas. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Without insulin, sugar levels increase in your bloodstream. Type 2 diabetes is the most commonly encountered form of diabetes. It transpires when your body loses its sensitivity to insulin or does not generate adequate insulin.
Symptoms of type 1 and type 2 diabetes are similar, but they may develop more slowly in type 2 diabetes.
Some of the most common symptoms of diabetes include:
- Increased thirst: When your blood sugar levels are high, your kidneys try to remove the excess glucose from your blood. This can lead to dehydration and increased thirst.
- Frequent urination: As your kidneys try to remove excess glucose from your blood, you may need to urinate more often.
- Extreme hunger: High blood sugar levels can signal to your brain that you are hungry, even if you have just eaten.
- Unexplained weight loss: High blood sugar levels can cause your body to break down muscle and fat for energy. This can lead to unexplained weight loss.
- Fatigue: High blood sugar levels can damage your nerves and blood vessels, which can lead to fatigue.
- Blurred vision: High blood sugar levels can damage the lenses in your eyes, which can lead to blurred vision.
- Slow-healing sores: High blood sugar levels can damage your nerves and blood vessels, which can make it difficult for sores to heal.
- Numbness or tingling in the hands or feet: High blood sugar levels can damage your nerves, which can lead to numbness or tingling in your hands and feet.
Other symptoms of diabetes may include:
- Headaches: Elevated blood glucose levels can lead to migraines.
- Skin infections: People with diabetes are more likely to develop skin infections.
- Yeast infections: People with diabetes are more likely to develop yeast infections.
- Mood changes: High blood sugar levels can cause mood swings, such as irritability and depression.
If you are experiencing any of the symptoms of diabetes, it is important to see a doctor right away. Early diagnosis and treatment can help to prevent serious complications of diabetes.
Here is a more detailed look at some of the most common symptoms of diabetes:
Increased thirst: When your blood sugar levels are high, your kidneys try to remove the excess glucose from your blood. This can lead to dehydration and increased thirst. You may find yourself drinking more water than usual, even at night.
Frequent urination: As your kidneys try to remove excess glucose from your blood, you may need to urinate more often. You may also find that you need to urinate more frequently at night.
Extreme hunger: High blood sugar levels can signal to your brain that you are hungry, even if you have just eaten. This may result in excessive consumption and increased body weight.
Unexplained weight loss: High blood sugar levels can cause your body to break down muscle and fat for energy. This can lead to unexplained weight loss, even if you are eating more than usual.
Fatigue: High blood sugar levels can damage your nerves and blood vessels, which can lead to fatigue. You may feel tired and weak all the time, even after getting a good night's sleep.
Blurred vision: High blood sugar levels can damage the lenses in your eyes, which can lead to blurred vision. You may have difficulty seeing clearly, especially when reading or driving.
Slow-healing sores: High blood sugar levels can damage your nerves and blood vessels, which can make it difficult for sores to heal. You may notice that minor cuts and scrapes take longer to heal than usual.
Numbness or tingling in the hands or feet: High blood sugar levels can damage your nerves, which can lead to numbness or tingling in your hands and feet. You may also experience pain or burning sensations in your hands and feet.
Other symptoms of diabetes may include:
- Headaches
- Skin infections
- Yeast infections
- Mood changes
If you are experiencing any of the symptoms of diabetes, it is important to see a doctor right away. Early diagnosis and treatment can help to prevent serious complications of diabetes.
Here are some tips for managing the symptoms of diabetes:
- Drink plenty of fluids: Drinking plenty of fluids will help to prevent dehydration and increased thirst. Strive to consume a minimum of eight glasses of water daily.
- Eat a healthy diet: Eating a healthy diet can help to control your blood sugar levels. Avoid sugary drinks and processed foods. Focus
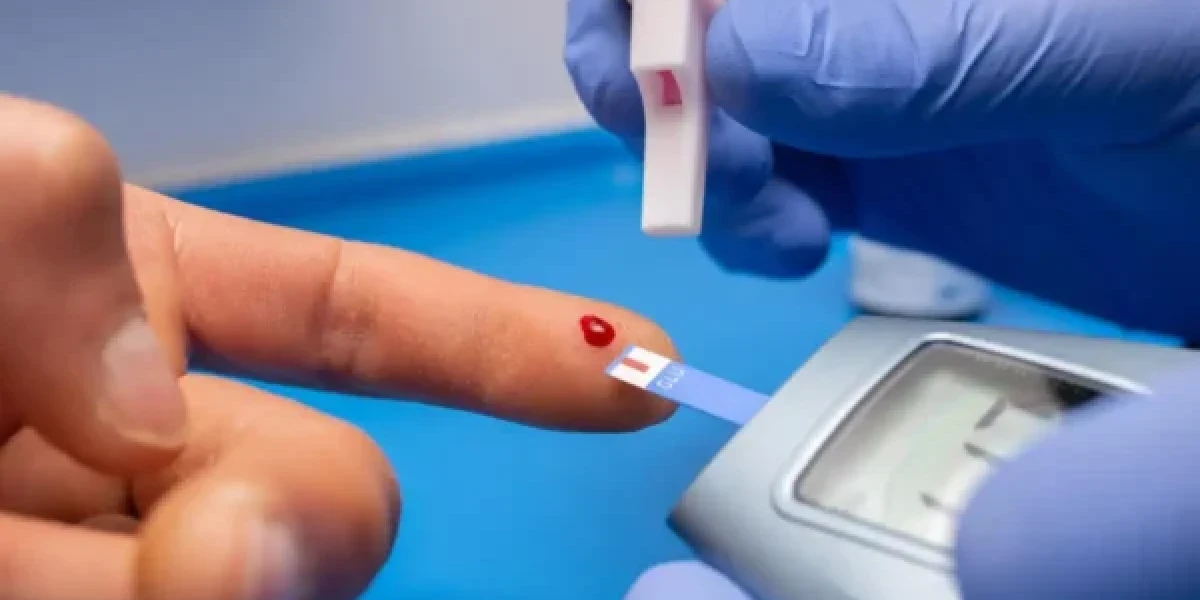
Diagnosis and Testing
Diabetes is diagnosed with a blood test. Diabetes can be diagnosed through two primary categories of blood tests:
- Fasting blood sugar test: This test measures your glucose level after an 8-hour fast.
- Oral glucose tolerance test (OGTT): This test measures your blood sugar level before and after you drink a sugary beverage.
If your blood sugar level is above the normal range on either of these tests, your doctor may diagnose you with diabetes.
Types of diabetes tests
There are a number of different diabetes tests that can be used to diagnose and manage diabetes. The most common tests are:
- Fasting blood sugar (FBS): This test measures your blood sugar level after you have not eaten for at least 8 hours. A normal FBS level is less than 100 mg/dL.
- Random blood sugar (RBS): This test measures your blood sugar level at any time of day, without regard to when you last ate. A normal RBS level is less than 180 mg/dL.
- Oral glucose tolerance test (OGTT): This test measures your blood sugar level before and after you drink a sugary beverage. A normal OGTT result is a blood sugar level of less than 200 mg/dL two hours after drinking the sugary beverage.
- Glycated hemoglobin (A1C): This test measures your average blood sugar level over the past 2-3 months. An A1C level within the normal range is less than 5.7%.
Diagnosis of diabetes
To diagnose diabetes, your doctor will need to see two abnormal blood sugar test results. For example, if you have an FBS of 126 mg/dL or higher on two separate days, you will be diagnosed with diabetes.
Diagnosis of prediabetes
your blood glucose levels are elevated but do not reach the threshold for a diabetes diagnosis, you might be in a prediabetic state. Prediabetes is a condition in which your blood sugar levels are elevated, but you do not yet meet the criteria for diabetes. People with prediabetes are at increased risk of developing type 2 diabetes and other health problems, such as heart disease and stroke.
If you have prediabetes, your doctor will recommend lifestyle changes to help you lower your blood sugar levels and reduce your risk of developing type 2 diabetes.
The Role of Insulin
Insulin is a hormone that plays a vital role in regulating blood sugar levels. After you eat, your blood sugar levels rise. This signals your pancreas to release insulin. Insulin subsequently attaches to receptors on your cells, facilitating the entry of glucose into the cells for energy utilization.
Insulin additionally aids in the storage of surplus glucose in the liver and muscles. When your blood sugar levels drop between meals, the liver releases stored glucose back into the bloodstream. This helps to ensure your blood sugar remains at a typical level.
Insulin Resistance
Insulin resistance is a condition in which your cells don't respond properly to insulin. This can happen for a number of reasons, including inactivity, obesity, and certain medical conditions.
When your cells are resistant to insulin, they don't take up as much glucose from the bloodstream. This might cause increased blood sugar levels.
Diabetes Complications
Cardiovascular Complications
Diabetes is a long-term condition that impacts the way your body converts food into energy. High blood sugar levels from diabetes can damage your blood vessels and nerves, which can lead to heart disease and stroke.
People with diabetes are twice as likely to have heart disease or stroke as people without diabetes. Diabetes can also lead to other cardiovascular complications, such as peripheral artery disease (PAD) and heart failure.
What causes diabetes cardiovascular complications?
Elevated blood glucose levels can harm your blood vessels through various mechanisms
- Atherosclerosis: High blood sugar can cause plaque to build up on the walls of your arteries. This can narrow or block your arteries, reducing blood flow to your heart and other organs.
- Hypertension: High blood sugar can also lead to high blood pressure. High blood pressure puts extra strain on your heart and blood vessels, making them more likely to rupture.
- Dyslipidemia: High blood sugar can also change the levels of fat and cholesterol in your blood. This can increase your risk of developing high cholesterol and triglycerides, which can contribute to atherosclerosis.
Types of diabetes cardiovascular complications
The most common diabetes cardiovascular complications are:
- Coronary heart disease (CHD): CHD is a type of heart disease that occurs when the arteries that supply blood to your heart become narrowed or blocked. This can lead to a heart attack.
- Stroke: A stroke occurs when the blood supply to your brain is interrupted or reduced, depriving part of the brain of oxygen and nutrients. Brain cells enter a state of demise in mere minutes.
- Peripheral artery disease (PAD): PAD is a condition that affects the arteries in your legs and feet. It may result in discomfort, lack of sensation, and a pins-and-needles sensation in your lower limbs. In severe cases, PAD can lead to gangrene and amputation.
- Heart failure: Heart failure is a condition in which your heart muscle is weakened or damaged and cannot pump enough blood to meet your body's needs.
Kidney Complications
Diabetes is a chronic medical issue that hampers your body's ability to convert food into energy. This can lead to serious health complications, including kidney disease.
Diabetic kidney disease (DKD) is a common complication of type 1 and type 2 diabetes. It is the primary factor responsible for end-stage renal disease (ESRD) in the United States. ESRD is a condition in which your kidneys can no longer filter waste products from your blood. People with ESRD need dialysis or a kidney transplant to survive.
What is diabetic kidney disease?
Diabetic kidney disease (DKD) is a form of chronic renal disease resulting from diabetes. It occurs when damage to the blood vessels in your kidneys prevents them from working properly. This can lead to a buildup of waste products in your blood, which can damage other organs in your body.
Risk factors for diabetic kidney disease
The following factors increase your risk of developing DKD:
- Long-standing diabetes
- Poor blood sugar control
- High blood pressure
- High cholesterol
- A family history of kidney disease
- Smoking
- Obesity
Stages of diabetic kidney disease
DKD has five stages, based on the severity of kidney damage:
- Stage 1: Early kidney damage, with no symptoms.
- Stage 2: Mild kidney damage, with no symptoms.
- Stage 3: Moderate kidney damage, with mild symptoms such as high blood pressure and protein in the urine.
- Stage 4: Severe kidney damage, with symptoms such as high blood pressure, protein in the urine, and anemia.
- Stage 5: End-stage renal disease (ESRD), with kidney failure and symptoms such as fatigue, shortness of breath, and swelling in the legs and feet.
Nerve Damage
Diabetes nerve damage, also known as diabetic neuropathy, is a common complication of diabetes. It occurs when high blood sugar levels damage the nerves throughout the body. Diabetic neuropathy can affect any nerve, but it most often damages nerves in the legs and feet.
Types of Diabetic Neuropathy
There are four main types of diabetic neuropathy:
- Peripheral neuropathy: This is the most common type of diabetic neuropathy. It affects the nerves in the hands and feet. Symptoms of peripheral neuropathy can include numbness, tingling, burning pain, weakness, and difficulty with balance and coordination.
- Autonomic neuropathy: This type of diabetic neuropathy affects the nerves that control the body's involuntary functions, such as digestion, heart rate, and blood pressure. Symptoms of autonomic neuropathy can include constipation, diarrhea, urinary incontinence, erectile dysfunction, and dizziness.
- Focal neuropathy: This type of diabetic neuropathy affects a single nerve or group of nerves. It can cause weakness, numbness, or pain in the affected area.
- Proximal neuropathy: This type of diabetic neuropathy is rare. It affects the nerves in the thighs, buttocks, and hips. Symptoms of proximal neuropathy can include weakness, pain, and wasting of the muscles in the affected areas.
Causes of Diabetic Neuropathy
High blood sugar levels can damage the nerves in several ways. Over time, high blood sugar levels can damage the blood vessels that supply the nerves with oxygen and nutrients. This can lead to nerve damage. Additionally, high blood sugar levels can damage the nerves directly.
Risk Factors for Diabetic Neuropathy
The following factors can increase your risk of developing diabetic neuropathy:
- Poor blood sugar control
- Long duration of diabetes
- Smoking
- Obesity
- High blood pressure
- High cholesterol levels
- Kidney disease
Symptoms of Diabetic Neuropathy
Symptoms of diabetic neuropathy can vary depending on the type and severity of the nerve damage. Some common symptoms include:
- Numbness
- Tingling
- Burning pain
- Weakness
- Difficulty with balance and coordination
- Constipation
- Diarrhea
- Urinary incontinence
- Erectile dysfunction
- Dizziness
- Vision problems
- Digestive problems
- Heart problems
Diagnosis of Diabetic Neuropathy
Your doctor can diagnose diabetic neuropathy by performing a physical exam and asking about your symptoms. Your doctor may also order tests, such as nerve conduction studies and electromyography, to assess the damage to your nerves.
Treatment for Diabetic Neuropathy
There is no cure for diabetic neuropathy, but there are treatments that can help to manage the symptoms and prevent further nerve damage. Treatment options for diabetic neuropathy include:
- Good blood sugar control: This is the most important thing you can do to prevent and manage diabetic neuropathy.
- Lifestyle changes: This includes eating a healthy diet, exercising regularly, and quitting smoking.
- Medication: There are a number of medications that can help to relieve the pain and other symptoms of diabetic neuropathy.
- Physical therapy: Physical therapy can help to improve your balance, coordination, and strength.
- Surgery: In some cases, surgery may be necessary to correct nerve damage.
Preventing Diabetic Neuropathy
The best way to prevent diabetic neuropathy is to keep your blood sugar levels under control. You can do this by following your doctor's treatment plan and making healthy lifestyle choices.
Management and Treatment
Medications
There are many different types of diabetes medications available, each with its own unique mechanism of action and side effects. The best medication for you will depend on your individual needs and circumstances.
Type 1 diabetes
Type 1 diabetes is an autoimmune disease in which your body attacks the cells in your pancreas that produce insulin. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Without insulin, there is a buildup of glucose in the bloodstream.
People suffering from type 1 diabetes can't survive without insulin injections. There are many different types of insulin available, including short-acting, intermediate-acting, and long-acting insulin. Your doctor will help you choose the right type of insulin for you and teach you how to inject it properly.
Type 2 diabetes
Type 2 diabetes is the most prevalent type of diabetes. It develops when your body exhibits insulin resistance or fails to produce an adequate amount of insulin.
There are many different types of diabetes medications available for people with type 2 diabetes. Several frequently prescribed drug categories are:
- Metformin: Metformin is the first-line medication for most people with type 2 diabetes. It helps to lower blood sugar levels by reducing the amount of glucose produced by the liver and improving the body's sensitivity to insulin.
- Sulfonylureas: Sulfonylureas work by increasing the amount of insulin released by the pancreas.
- Meglitinides: Meglitinides also work by increasing the amount of insulin released by the pancreas, but they do so in a different way than sulfonylureas.
- Thiazolidinediones: Thiazolidinediones help to lower blood sugar levels by improving the body's sensitivity to insulin.
- DPP-4 inhibitors: DPP-4 inhibitors work by blocking the action of a hormone that breaks down GLP-1, a hormone that helps to lower blood sugar levels.
- GLP-1 receptor agonists: GLP-1 receptor agonists are injectable medications that mimic the effects of GLP-1. They are very effective at lowering blood sugar levels and can also help to reduce weight and improve cardiovascular health.
- SGLT2 inhibitors: SGLT2 inhibitors work by causing the kidneys to excrete excess glucose in the urine. They can be very effective at lowering blood sugar levels and can also help to reduce weight and blood pressure.
Combination therapy
Many people with type 2 diabetes need to take a combination of two or more different medications to control their blood sugar levels. Your doctor will work with you to choose the best combination therapy for you.
Side effects of diabetes medications
All medications can have side effects. Some of the most common side effects of diabetes medications include:
- Metformin: Upset stomach, diarrhea, gas
- Sulfonylureas: Hypoglycemia (low blood sugar), weight gain
- Meglitinides: Hypoglycemia, weight gain
- Thiazolidinediones: Weight gain, fluid retention, heart failure
- DPP-4 inhibitors: Headache, nausea, diarrhea
- GLP-1 receptor agonists: Nausea, vomiting, diarrhea, stomach pain
- SGLT2 inhibitors: Urinary tract infections, increased risk of amputation
If you are experiencing any side effects from your diabetes medication, talk to your doctor. They may be able to adjust your dose or switch you to a different medication.
Choosing the right diabetes medication for you
There are many factors to consider when choosing a diabetes medication, including:
- Your blood sugar levels
- Your age
- Your overall health
- Your lifestyle
- The cost of the medication
Your doctor will work with you to choose the best diabetes medication for your individual needs and circumstances.
Managing your diabetes
In addition to taking medication, there are other things you can do to manage your diabetes, such as:
- Eating a healthy diet
- Exercising regularly
- Maintaining a healthy weight
- Monitoring your blood sugar levels regularly
By managing your diabetes, you can help to reduce your risk of complications, such as heart disease, stroke, and kidney disease.
Lifestyle Changes
Diabetes is a chronic (long-lasting) health condition that affects how your body turns food into energy. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease in which your body attacks and destroys the cells in your pancreas that make insulin. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Without insulin, glucose builds up in your blood. Type 2 diabetes is the most common form of diabetes. It occurs when your body becomes resistant to insulin or doesn't make enough insulin.
Diabetes can lead to serious health complications, such as heart disease, stroke, kidney disease, blindness, nerve damage, and amputation. However, lifestyle changes can help to manage diabetes and prevent or delay complications.
What are the benefits of lifestyle changes for diabetes?
Lifestyle changes can have a number of benefits for people with diabetes, including:
- Lower blood sugar levels
- Reduced risk of complications
- Improved overall health and well-being
What lifestyle changes are recommended for people with diabetes?
The following lifestyle changes are recommended for people with diabetes:
- Eat a healthy diet. A healthy diet for diabetes is low in processed foods, sugary drinks, and saturated and unhealthy fats. It is also high in fruits, vegetables, and whole grains.
- Exercise regularly. Aim to complete 30 minutes of moderately strenuous exercise on a regular basis.
- Maintain a healthy weight. Managing diabetes can be more challenging for individuals who are overweight or obese.Losing even a small amount of weight can have a big impact on blood sugar levels.
- Quit smoking. Smoking can damage your blood vessels and make it more difficult to control your blood sugar levels.
How to make diabetes lifestyle changes
Making diabetes lifestyle changes can be challenging, but it is important to remember that you are not alone. There are many resources available to help you get started and stay on track.
Here are some tips for making diabetes lifestyle changes:
- Set realistic goals. Don't try to change everything at once. Start with small changes that you can make and stick to.
- Find a support system. Having friends or family members who are also making lifestyle changes can make it easier to stay motivated.
- Talk to your doctor or a registered dietitian. They can help you create a personalized plan for eating healthy and exercising safely.
Examples of diabetes lifestyle changes
Here are some examples of diabetes lifestyle changes that you can make:
Diet:
- Eat plenty of fruits and vegetables. Fruits and vegetables are low in calories and high in nutrients, including fiber and vitamins.
- Choose whole grains over refined grains. Whole grains are a good source of fiber, which can help to control blood sugar levels.
- Limit processed foods, sugary drinks, and saturated and unhealthy fats. Processed foods, sugary drinks, and saturated and unhealthy fats can all contribute to high blood sugar levels.
- Read food labels carefully. Pay attention to the serving size and the amount of calories, carbohydrates, fat, and sugar in each serving.
Exercise:
- Strive for a minimum of 30 minutes of moderate-intensity physical activity on a daily basis.
- If you are a beginner in exercise, begin at a gentle pace and progressively extend the duration of your workouts on a weekly basis.
- Be sure to have a conversation with your medical practitioner before beginning any new fitness regimen.
Weight loss:
- If you are overweight or obese, losing even a small amount of weight can have a big impact on your blood sugar levels.
- Aim to lose 5-10% of your body weight.
- You can lose weight by eating a healthy diet and exercising regularly.
Smoking cessation:
- Ceasing tobacco use is among the most beneficial actions you can take for your well-being
- There are many resources available to help you quit smoking, such as nicotine replacement therapy and counseling.
Diet and Nutrition
Diabetes is a persistent (long-term) medical condition that impacts the way your body converts food into energy. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disorder characterized by the immune system's assault on the pancreatic cells that generate insulin. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Insulin deficiency or resistance to insulin are the underlying factors in Type 2 diabetes, leading to elevated blood glucose levels.
Diet and nutrition play an important role in managing diabetes. Eating a healthy diet can help you control your blood sugar levels, maintain a healthy weight, and reduce your risk of developing complications from diabetes.
What is a healthy diet for people with diabetes?
A healthy diet for people with diabetes is similar to a healthy diet for everyone else. It should be rich in fruits, vegetables, and whole grains. It should also be low in saturated and trans fats, cholesterol, and added sugar.
Here are some specific tips for eating a healthy diet with diabetes:
- Choose whole grains over refined grains. Whole grains are a good source of fiber, which can help to slow the absorption of sugar into your bloodstream.
- Eat plenty of fruits and vegetables. Fruits and vegetables have a low calorie content and are rich in essential nutrients such as fiber, vitamins, and minerals.
- Choose lean protein sources. Lean protein options like poultry, seafood, legumes, and soybean products are both low in saturated fat and calories.
- Limit saturated and trans fats. Saturated and trans fats have the potential to elevate your cholesterol levels, thereby enhancing the likelihood of heart disease.
- Limit cholesterol. Cholesterol can also raise your cholesterol levels and increase your risk of heart disease.
- Limit added sugar. Added sugar can raise your blood sugar levels and contribute to weight gain.
What foods should people with diabetes avoid?
People with diabetes should avoid foods that are high in sugar, saturated and trans fats, and cholesterol. These foods can raise your blood sugar levels and increase your risk of developing complications from diabetes.
Here are some specific examples of foods that people with diabetes should avoid:
- Sugar-sweetened drinks, such as soda, juice, and sports drinks
- Candy, cookies, and other sweets
- Pastries, white bread, and other refined grains
- Fried foods, such as French fries and chicken nuggets
- Fatty meats, such as bacon and sausage
- High-fat dairy products, like whole milk and cheese.
Meal planning for people with diabetes
Meal planning can help people with diabetes to manage their blood sugar levels. When planning meals, it is important to consider the amount and type of carbohydrates in each food. Carbohydrates are broken down into glucose, which is the main source of energy for your body.
Here are some tips for meal planning for people with diabetes:
- Spread your carbohydrates throughout the day. Eating three regular meals and two to three snacks each day can help to keep your blood sugar levels stable.
- Choose low-glycemic index (GI) carbohydrates. Low-GI carbohydrates are broken down more slowly into glucose, which helps to prevent blood sugar spikes.
- Include fiber at every meal. Fiber helps to slow the absorption of sugar into your bloodstream.
- Pair carbohydrates with protein and healthy fats. Protein and healthy fats can help to slow the absorption of sugar into your bloodstream and keep you feeling full longer.
Exercise and diabetes
Exercise is another important part of managing diabetes. Exercise helps to lower your blood sugar levels, improve your insulin sensitivity, and promote weight loss.
Adults with diabetes should aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity each week. They should also do strength-training exercises at least twice a week.
Exercise and Diabetes
Diabetes is a persistent (long-term) medical condition that impacts the way your body converts food into energy. There are two main types of diabetes: type 1 and type 2.
Type 1 diabetes is an autoimmune condition where your immune system targets and eliminates the pancreatic cells responsible for producing insulin. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Without insulin, glucose accumulates in your bloodstream.
Type 2 diabetes is the most prevalent type of diabetes. It develops when your body's responsiveness to insulin decreases or when your body doesn't produce a sufficient amount of insulin.
Exercise is an important part of managing diabetes. It can help to lower your blood sugar levels, improve your insulin sensitivity, and reduce your risk of developing complications of diabetes.
Body
How does exercise help to manage diabetes?
Exercise helps to manage diabetes in a number of ways. Initially, it aids in reducing your blood sugar levels. During exercise, your muscles utilize glucose as a source of energy. This can help to reduce the amount of glucose in your bloodstream.
Second, exercise improves your insulin sensitivity. Insulin sensitivity is how well your cells respond to insulin. When your cells are more insulin sensitive, they are better able to take up glucose from your bloodstream.
Third, exercise can help to reduce your risk of developing complications of diabetes. Complications of diabetes can include heart disease, stroke, kidney disease, and blindness. Exercise can help to reduce your risk of developing these complications by lowering your blood sugar levels, improving your cholesterol levels, and reducing your blood pressure.
What types of exercise are best for people with diabetes?
All types of exercise are beneficial for people with diabetes. However, some types of exercise are better than others for people with diabetes.
Aerobic exercise is the best type of exercise for people with diabetes. Aerobic exercise is any type of exercise that gets your heart rate up and your breathing going. Examples of aerobic exercise include walking, running, biking, swimming, and dancing.
Resistance exercise is also beneficial for people with diabetes. Resistance exercise is any type of exercise that works your muscles against resistance. Examples of resistance exercise include lifting weights, using resistance bands, and doing bodyweight exercises such as push-ups and sit-ups.
How much exercise should people with diabetes do?
The American Diabetes Association recommends that adults with diabetes get at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise each week. They also recommend that adults with diabetes do resistance exercise that works all major muscle groups at least two times per week.
How to start an exercise program
If you are new to exercise, it is important to start slowly and gradually increase the amount of exercise you do each week. It is also important to talk to your doctor before starting an exercise program, especially if you have any health problems.
Here are some tips for starting an exercise program:
- Start with 10-15 minutes of exercise three times per week.
- Gradually increase the amount of time you exercise each week until you are reaching the recommended amount of exercise.
- Discover a pastime that you find pleasurable and that aligns with your daily routine
- Set realistic goals.
- Listen to your body and take breaks when you need them.
Monitoring Blood Sugar
Diabetes is a persistent medical condition that impacts the way your body converts food into fuel. When you eat, your body breaks down carbohydrates into glucose, or blood sugar. Insulin, a hormone produced by your pancreas, helps glucose enter your cells.
People with diabetes either don't make enough insulin or their cells don't respond properly to insulin. This can lead to high blood sugar levels, which can damage your nerves, blood vessels, and organs over time.
Blood sugar monitoring is an essential part of diabetes management. It helps you track your blood sugar levels and identify patterns. This information can help you adjust your diabetes treatment plan, such as your insulin dosage, diet, and exercise routine.
Why is blood sugar monitoring important?
Blood sugar monitoring is important for a number of reasons, including:
- To prevent diabetes complications. High blood sugar levels can damage your nerves, blood vessels, and organs over time. This can lead to serious health problems, such as heart disease, stroke, kidney disease, blindness, and nerve damage.
- To avoid high and low blood sugar levels. High blood sugar levels (hyperglycemia) can cause symptoms such as thirst, fatigue, and blurred vision. Low blood sugar levels (hypoglycemia) can cause symptoms such as dizziness, shakiness, and confusion. Severe hypoglycemia can be life-threatening.
- To track the effectiveness of your diabetes treatment plan. Blood sugar monitoring can help you see how your diabetes treatment plan is working and make adjustments as needed.
How to monitor your blood sugar
There are two main ways to monitor your blood sugar:
- Self-monitoring of blood glucose (SMBG): This involves testing your blood sugar levels using a blood glucose meter. SMBG is the most common way to monitor blood sugar levels.
- Continuous glucose monitoring (CGM): This involves wearing a device that measures your blood sugar levels every few minutes. CGM can be more convenient than SMBG, but it is also more expensive.
How often should you monitor your blood sugar?
How often you need to monitor your blood sugar depends on your type of diabetes, your treatment plan, and your overall health. Your doctor will work with you to create a blood sugar monitoring plan that is right for you.
Here are some general guidelines for blood sugar monitoring:
- People with type 1 diabetes typically need to monitor their blood sugar levels four to eight times a day.
- People with type 2 diabetes who take insulin typically need to monitor their blood sugar levels three to four times a day.
- People with type 2 diabetes who take oral medications or make lifestyle changes may only need to monitor their blood sugar levels once or twice a day.
- Pregnant women with diabetes need to monitor their blood sugar levels more often, typically six to eight times a day.
Interpreting your blood sugar results
Your blood sugar levels should be within a certain range, depending on your type of diabetes and your treatment plan. Your doctor will work with you to set target blood sugar levels.
If your blood sugar levels are above or below your target range, you may need to adjust your diabetes treatment plan. For example, you may need to take more insulin, change your diet, or exercise more.
Tips for blood sugar monitoring
- Make sure to wash your hands thoroughly with soap and water before and after testing your blood sugar.
- Use a clean lancet each time you test your blood sugar.
- Prick your finger on the side, not the tip.
- Apply a small amount of pressure to your finger to get a drop of blood.
- Place the drop of blood on the test strip and insert it into the blood glucose meter.
- Wait for the meter to display your blood sugar reading.
- Record your blood sugar results in a logbook or tracking app.
Support and Education
There are many different types of diabetes support and education available, including:
- Individual counseling: Individual counseling can be a great way to get personalized support and education from a diabetes care and education specialist.
- Group classes: Group classes can be a good way to learn from and support other people with diabetes.
- Online resources: There are many online resources available that can provide information and support on diabetes management.
Benefits of diabetes support and education
Diabetes support and education can offer a number of benefits, including:
- Improved knowledge of diabetes management: Diabetes support and education can help people with diabetes learn about the different aspects of diabetes management, such as blood sugar monitoring, meal planning, exercise, and medication.
- Increased confidence and self-efficacy: Diabetes support and education can help people with diabetes feel more confident and capable of managing their diabetes.
- Better blood sugar control: Diabetes support and education can help people with diabetes improve their blood sugar control, which can reduce their risk of complications.
- Reduced risk of complications: Diabetes support and education can help people with diabetes reduce their risk of complications such as heart disease, stroke, kidney disease, and blindness.
Promising Research and Developments
Diabetes is a chronic health condition that affects how your body turns food into energy. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune condition where the immune system targets and eradicates the insulin-producing cells in the pancreas. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Insulin deficiency leads to an accumulation of glucose in your bloodstream. Type 2 diabetes, the most prevalent type of diabetes, develops when your body exhibits resistance to insulin or fails to produce an adequate amount of insulin
While there is no cure for diabetes, there are many promising research and developments underway. These new discoveries could lead to better treatments and, one day, a cure for diabetes.
Body
Stem cell therapy
Stem cell therapy is a promising new approach to treating type 1 diabetes. Stem cells are undifferentiated cells that have the potential to develop into any type of cell in the body. Researchers are working to develop stem cell therapies that can replace the destroyed insulin-producing beta cells in people with type 1 diabetes.
In one clinical trial, researchers at Harvard University transplanted stem cell-derived beta cells into 17 people with type 1 diabetes. After one year, all of the participants were able to produce some insulin on their own, and many were able to reduce their insulin injections.
Islet transplantation
Islet transplantation is another promising treatment approach for type 1 diabetes. Islets are clusters of cells from the pancreas that include insulin-producing beta cells. In islet transplantation, surgeons transplant islets from a donor into a person with type 1 diabetes.
Islet transplantation has been shown to be effective in controlling blood sugar levels and reducing the risk of complications from diabetes. However, it is a complex procedure with a number of risks, and it is not suitable for everyone.
Artificial pancreas
An artificial pancreas is a device that would monitor blood sugar levels and deliver insulin automatically, as needed. This would eliminate the need for people with type 1 diabetes to test their blood sugar levels and inject insulin multiple times a day.
Researchers are developing several different types of artificial pancreas systems. Some systems use a continuous glucose monitor (CGM) to track blood sugar levels and an insulin pump to deliver insulin. Other systems are more complex and include a computer chip that makes decisions about how much insulin to deliver.
New diabetes medications
Researchers are also developing new diabetes medications that are more effective and have fewer side effects than existing medications. For example, a new class of drugs called SGLT2 inhibitors has been shown to be very effective in lowering blood sugar levels and reducing the risk of heart disease and stroke in people with type 2 diabetes.
Living with Diabetes
Diabetes is a lifelong condition, but it can be managed with lifestyle changes, medication, or insulin therapy. Living with diabetes can be challenging, but it is important to remember that you are not alone. There are many resources available to help you manage your diabetes and live a healthy and fulfilling life.
Conclusion
This comprehensive guide has covered the essential aspects of diabetes, from understanding the types and causes to managing the condition, preventing it, and addressing its impact on special populations. We've explored ongoing research, psychosocial considerations, community support, and the promising future of diabetes care. With this knowledge, individuals and communities can make informed decisions to tackle diabetes effectively, improving the health and well-being of millions.
FAQs (Frequently Asked Questions)
- What is diabetes?
Diabetes is a persistent condition that impacts the way your body converts food into fuel.
- What are the types of diabetes?
There are two main types of diabetes: type 1 and type 2.
- Type 1 diabetes is an autoimmune condition where the body's immune system targets and eliminates the insulin-producing cells in the pancreas Insulin is a hormone that helps glucose enter your cells from your bloodstream. Without insulin, glucose accumulates in your bloodstream.
- Type 2 diabetes is the most prevalent type of diabetes. It develops when your body becomes unresponsive to insulin or doesn't produce an adequate amount of insulin.
- What are the symptoms of diabetes?
Some of the common symptoms of diabetes are:
- Increased thirst
- Frequent urination
- Extreme hunger
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Pins and needles
- How is diabetes diagnosed?
Diabetes is diagnosed with a blood test. The most common blood tests used to diagnose diabetes are the fasting blood sugar test and the oral glucose tolerance test.
- How is diabetes treated?
There is no cure for diabetes, but it can be managed with lifestyle changes, medication, or insulin therapy.
- Lifestyle changes: Eating a healthy diet, exercising regularly, and maintaining a healthy weight are the first line of treatment for type 2 diabetes. Lifestyle changes can also help to improve blood sugar control and reduce the risk of complications in people with type 1 diabetes.
- Medication: There are a variety of medications available to treat diabetes. Oral medications are often the first line of treatment for type 2 diabetes. Injectable medications may also be used, either alone or in combination with oral medications. People with type 1 diabetes need to take insulin injections.
- Insulin therapy: Insulin therapy is a common treatment for type 1 diabetes and is also used in some cases of type 2 diabetes. Insulin is a hormone that helps glucose enter your cells from your bloodstream. Insulin can be administered via a syringe, pen, or pump.
- What are the complications of diabetes?
Over time, elevated blood sugar levels can harm your nerves, blood vessels, and organs. Diabetes can result in severe health issues, which include:
- Heart disease
- Stroke
- Kidney disease
- Blindness
- Nerve damage
- Amputation
- How can I prevent diabetes?
There is no foolproof way to prevent diabetes, but there are things you can do to reduce your risk, such as:
- Maintaining a healthy weight
- Eating a healthy diet
- Exercising regularly
- Getting regular checkups
- What is the difference between type 1 and type 2 diabetes?
Type 1 diabetes is a condition characterized by an autoimmune response where your immune system targets and eliminates the pancreatic cells responsible for producing insulin. Type 2 diabetes is the most common form of diabetes and occurs when your body becomes resistant to insulin or doesn't make enough insulin.
- Is there a cure for diabetes?
There is no cure for diabetes, but it can be managed with lifestyle changes, medication, or insulin therapy.
- How can I live a healthy life with diabetes?
There are many things you can do to live a healthy life with diabetes, such as:
- Monitoring your blood sugar levels regularly
- Eating a healthy diet
- Exercising regularly
- Taking your medications as prescribed
- Managing stress
- Getting regular checkups
Important Reminder:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.