Introduction
Botulism is a rare but potentially fatal illness that demands urgent attention due to its severe and life-threatening nature. Caused by the bacterium Clostridium botulinum, botulism has significant implications for public health. Understanding the types, symptoms, causes, and treatments of botulism is crucial in raising awareness and promoting preventive measures. Early diagnosis and prompt treatment can significantly improve outcomes and reduce the risk of severe complications. By delving into the intricacies of botulism, we aim to shed light on this critical health issue and empower individuals to recognize the signs and seek appropriate medical care.
What is botulism (Clostridium botulinum)?
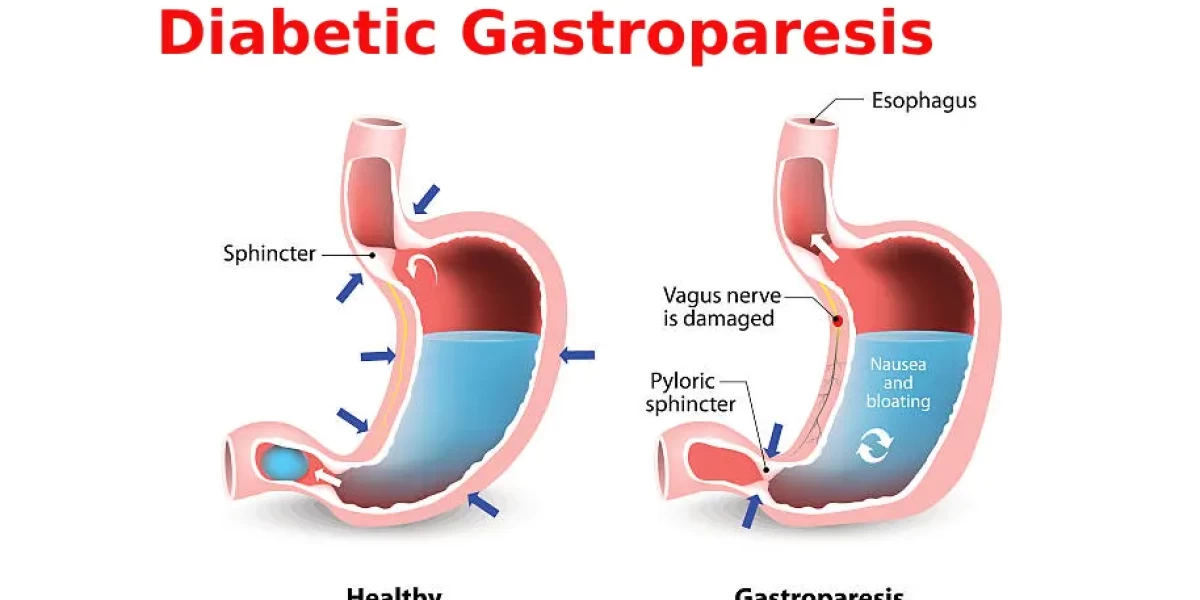
Botulism is a serious illness characterized by the production of a potent neurotoxin by the bacterium Clostridium botulinum. This anaerobic bacterium thrives in low-oxygen environments, such as improperly canned or preserved foods, wounds, and sometimes in the intestines of infants. The neurotoxin produced by Clostridium botulinum is one of the most potent toxins known to science, capable of causing paralysis and even death if not treated promptly.
The botulinum toxin targets the nervous system by interfering with the normal functioning of neurons. It blocks the release of acetylcholine, a neurotransmitter essential for muscle contraction, leading to muscle paralysis. The severity of botulism depends on the amount of toxin absorbed and the speed of medical intervention. Symptoms often include weakness, dizziness, double vision, difficulty speaking and swallowing, and paralysis that can progress to the respiratory muscles, making it difficult to breathe.
Given its rapid progression and potential severity, understanding the signs and symptoms of botulism is critical for early detection and treatment. Healthcare professionals must be vigilant in recognizing the symptoms and administering appropriate treatments, such as antitoxins, to neutralize the toxin and supportive care to assist with breathing and other functions. In conclusion, awareness and education about botulism are essential for preventing outbreaks and ensuring timely medical intervention, ultimately saving lives.
Types of Botulism
Botulism is a rare but serious illness caused by toxins produced by the bacterium Clostridium botulinum. There are several types of botulism, each with unique characteristics, modes of contraction, and risks. These include foodborne botulism, wound botulism, infant botulism, and adult intestinal colonization botulism. Understanding the differences between these types is crucial in recognizing symptoms early and preventing the spread of the disease.
1. Foodborne Botulism
Foodborne botulism occurs when people consume food that contains the botulinum toxin. This typically happens when food is improperly canned or preserved in low-oxygen environments where the bacteria can thrive. The toxin develops in anaerobic conditions, meaning it requires an environment with little to no oxygen. Common examples include home-canned vegetables, meats, and fish that have not been processed correctly.
Symptoms of foodborne botulism usually appear within 12 to 36 hours after ingestion and can include nausea, vomiting, abdominal pain, and, more critically, neurological symptoms like difficulty breathing, muscle weakness, and blurred vision. Since the toxin affects the nervous system, foodborne botulism can lead to paralysis if not treated promptly. People who practice home canning should be especially cautious about following safety guidelines to reduce the risk of contamination.
2. Wound Botulism
Wound botulism occurs when Clostridium botulinum bacteria infect a wound and produce toxins that spread throughout the body. Unlike foodborne botulism, which is ingested, this type is contracted through the contamination of wounds, especially those that are deep or punctured. Wound botulism has been increasingly linked to people who inject drugs, particularly black tar heroin users, as the drug can introduce bacteria into the body through unsterilized needles.
The symptoms of wound botulism resemble those of foodborne botulism, including muscle weakness, difficulty speaking, and problems with vision. However, wound botulism typically takes longer to develop, with symptoms appearing around 10 days after the initial infection. Immediate medical attention is necessary to prevent the toxin from spreading further and causing life-threatening complications.
3. Infant Botulism
Infant botulism affects babies under one year of age. This form of botulism occurs when an infant ingests Clostridium botulinum spores, which then grow and produce toxins in the baby's intestines. Unlike adults, infants do not have fully developed gut flora, which makes them more susceptible to the growth of harmful bacteria like C. botulinum.
The most common source of spores in infant botulism is honey, which is why it is advised not to feed honey to infants under one year of age. Symptoms of infant botulism include constipation, weak cry, poor feeding, and muscle weakness, often described as a "floppy baby" appearance. If left untreated, it can lead to respiratory failure. However, with early medical intervention, most infants recover fully.
4. Adult Intestinal Colonization Botulism
This rare form of botulism occurs in adults who have an underlying health condition that disrupts their normal gut flora, such as after long-term antibiotic use or certain gastrointestinal surgeries. Like infant botulism, adult intestinal colonization happens when spores of the bacterium colonize the intestines and produce toxins.
Symptoms of adult intestinal botulism are similar to other forms of the disease, including muscle paralysis, blurred vision, and difficulty swallowing. Although rare, it is important to recognize the risk factors associated with this type of botulism, especially in people with weakened immune systems or compromised gastrointestinal health.
Symptoms of Botulism

Botulism's symptoms are alarming due to the toxin’s effect on the nervous system. The onset of symptoms varies depending on the type of botulism and how the toxin enters the body. Understanding these symptoms is key to ensuring timely diagnosis and treatment, as botulism can be life-threatening if not addressed quickly.
1. Early Symptoms
In foodborne botulism, symptoms typically appear within 12 to 36 hours of consuming contaminated food. In cases of wound botulism, it may take 10 days or more after the infection of the wound. The first signs of botulism are often gastrointestinal, such as nausea, vomiting, or abdominal pain.
2. Neurological Symptoms
As the toxin spreads, it affects the body’s nervous system, causing more severe symptoms such as blurred vision, dry mouth, difficulty swallowing, slurred speech, and muscle weakness. These symptoms occur because the botulinum toxin blocks the nerve signals that trigger muscle contractions. Paralysis often starts with the face and neck muscles and can spread to the arms, chest, and legs.
3. Respiratory Complications
One of the most critical aspects of botulism is its impact on respiratory muscles. If not treated quickly, the toxin can paralyze these muscles, leading to difficulty breathing or respiratory failure. In severe cases, mechanical ventilation may be required to help the patient breathe until the effects of the toxin wear off.
Causes of Botulism
Botulism is caused by the bacterium Clostridium botulinum, which thrives in low-oxygen environments. The bacteria produce spores that can survive in harsh conditions, and these spores release the deadly toxin when they find the right environment to grow.
1. Low-Oxygen Environments
The most common environment for C. botulinum to thrive is in canned or preserved foods where oxygen is limited. Improperly processed or home-canned foods create an anaerobic environment, perfect for the bacteria to produce toxins. This is why proper food preservation techniques are critical in preventing foodborne botulism.
2. Contaminated Wounds
In the case of wound botulism, the bacteria enter through open wounds, particularly deep or punctured ones. Drug use, especially with unclean needles, increases the risk of contamination and subsequent infection with C. botulinum.
3. Infant and Adult Colonization
Infants can contract botulism by ingesting spores, often from honey or soil, which then grow in their immature digestive systems. Adults with compromised gut health can also develop a rare form of intestinal colonization botulism under specific conditions, such as after antibiotic use.
Risk Factors for Botulism
Certain factors increase the likelihood of contracting botulism, whether from food, wounds, or intestinal colonization.
1. Age
Infants under one year old are at a higher risk of developing botulism due to their undeveloped gut flora. Adult intestinal colonization is also more common in older adults or those with compromised gut health.
2. Health Conditions
People with gastrointestinal disorders, those who have undergone specific surgeries, or those with compromised immune systems are at higher risk for adult intestinal colonization botulism. Similarly, people with open wounds or skin injuries are more susceptible to wound botulism, particularly if the wound becomes infected with C. botulinum.
3. Lifestyle Factors
Lifestyle choices can also increase the risk of botulism. For example, people who consume home-canned foods without following proper safety measures are at higher risk for foodborne botulism. Drug users, particularly those injecting black tar heroin, are at risk for wound botulism due to the unsterile conditions in which the drug is often prepared and injected.
Diagnosis of Botulism
1 Medical History
The diagnosis of botulism begins with a thorough medical history. Doctors will ask about recent consumption of canned or preserved foods, potential exposure to contaminated wounds, or drug use. Infants who develop botulism may have ingested honey or been exposed to soil.
2 Physical Examination
Physical examination is crucial for identifying botulism. During the exam, doctors assess muscle strength, reflexes, and neurological function. They will look for signs such as drooping eyelids, difficulty speaking, and weakness, which are hallmark symptoms of the toxin's impact on the nervous system.
3 Laboratory Tests
To confirm the diagnosis, laboratory tests are necessary. These may include:
- Toxin detection: Blood, stool, or food samples can be tested for the botulinum toxin.
- Electromyography (EMG): This test measures muscle response to nerve stimulation and can help identify muscle weakness caused by botulism.
- Lumbar puncture: In cases of infant botulism, a spinal tap may be conducted to rule out other neurological conditions.
Early diagnosis is essential, as botulism can progress rapidly. If left untreated, the condition can cause respiratory failure and death, making timely intervention critical.
Treatments for Botulism
1 Antitoxin Administration
Once botulism is diagnosed, the first line of treatment is the administration of an antitoxin. The antitoxin works by neutralizing the circulating botulinum toxin, preventing it from binding to nerve endings. While it cannot reverse damage already done, it can prevent further damage from occurring.
- Equine-derived antitoxin: This is used for treating adults and children with foodborne or wound botulism.
- Human-derived antitoxin: Specifically for infants, this antitoxin helps treat infant botulism.
2 Supportive Care
Since botulism affects the muscles involved in breathing, patients often require supportive care. This can include:
- Mechanical ventilation: For those experiencing respiratory failure.
- Feeding tubes: If swallowing becomes difficult.
- Physical therapy: To help regain muscle strength as recovery progresses.
Patients may need weeks or even months of supportive care to recover fully from botulism. Early intervention can significantly improve outcomes and prevent long-term complications.
Prevention of Botulism
Safe Food Handling and Canning Techniques
The key to preventing botulism lies in proper food handling and canning techniques. When preserving food at home:
- Sterilize equipment: Ensure all equipment used in canning is sterilized.
- Pressure cooking: Use a pressure cooker to kill any botulism spores that may be present.
- Avoid damaged cans: Do not consume food from bulging or damaged cans, as they may harbor the botulinum toxin.
Raising Awareness and Educating Others
Education plays a vital role in preventing botulism. Informing others about the risks associated with improper food preservation and the dangers of contaminated wounds can save lives. Encourage friends and family to stay informed and practice safe food handling techniques.
Conclusion
Botulism is a serious condition that requires prompt diagnosis and treatment. By understanding the symptoms, risk factors, and methods of prevention, you can protect yourself and others from this potentially life-threatening illness. Early intervention is crucial, so if you suspect you or someone you know has been exposed to the botulinum toxin, seek medical attention immediately. Together, we can reduce the risks associated with botulism through awareness and education.
Frequently Asked Questions(FAQ's)
1. Can botulism be cured?
Botulism can be treated with antitoxins and supportive care, but recovery may take time, especially if respiratory failure occurs.
2. How quickly does botulism progress?
Symptoms usually appear within 12 to 36 hours after exposure, and without treatment, the illness can progress rapidly, leading to severe complications.
3. Is it safe to eat home-canned food?
Yes, but only if proper canning techniques are followed, including the use of pressure cookers to kill any potential spores.
4. Can infants develop botulism from honey?
Yes, infants under one year old should not consume honey, as it can contain Clostridium botulinum spores that can cause infant botulism.
5. What should I do if I suspect botulism?
Seek immediate medical attention. Early diagnosis and treatment are critical to preventing serious complications.
6. What are the 3 types of botulism?
The three main types of botulism are:
- Foodborne botulism: Occurs when someone consumes food contaminated with the botulinum toxin.
- Infant botulism: Happens when infants ingest spores of the bacteria, which then grow and release toxins in the intestines.
- Wound botulism: Arises when the bacteria infect a wound and produce toxins.
7. What are the causes and symptoms of botulism?
Causes: Botulism is caused by toxins produced by the bacterium Clostridium botulinum. The bacteria thrive in low-oxygen environments, such as improperly canned foods, or wounds.
Symptoms: Common symptoms include:
- Muscle weakness
- Difficulty swallowing or speaking
- Double or blurred vision
- Dry mouth
- Paralysis, which can lead to respiratory failure if not treated promptly
8. What is the best treatment for botulism?
The best treatment includes:
- Antitoxins: Administered to neutralize the botulinum toxin in the body.
- Supportive care: Such as mechanical ventilation if breathing is affected.
- Wound care: If wound botulism is present, the infected tissue may need to be surgically cleaned and treated with antibiotics.
9. What are the different types of botulinum toxin?
There are seven types of botulinum toxin, labeled A through G. However, types A, B, E, and rarely F are known to cause illness in humans. Type C and D primarily affect animals, while type G is less understood.
10. What is botulinum toxin type A treatment?
Botulinum toxin type A, commercially known as Botox, is used for:
- Medical treatments: Managing conditions like muscle spasticity, chronic migraines, and hyperhidrosis (excessive sweating).
- Cosmetic procedures: Reducing wrinkles and fine lines by temporarily paralyzing facial muscles.
11. What are the four types of neurotoxins?
The four primary types of neurotoxins include:
- Botulinum toxin
- Tetrodotoxin
- Saxitoxin
- α-latrotoxin
12. What is neurotoxin treatment?
Treatment depends on the specific neurotoxin involved. In general:
- Antitoxins: For toxins like botulinum, specific antitoxins can neutralize their effects.
- Symptomatic treatment: Managing symptoms such as muscle paralysis or breathing difficulties.
- Supportive care: Sometimes, this includes ventilators or pain management, depending on the toxin's effects.
13. What are the 5 neurotoxins?
Five well-known neurotoxins include:
- Botulinum toxin
- Tetrodotoxin
- Saxitoxin
- Mercury
- Lead
14. What is botulinum toxin type B?
Botulinum toxin type B, also known by the brand name Myobloc, is another form of botulinum used for medical treatments. It’s primarily employed when patients are resistant to type A treatments. It helps treat conditions like cervical dystonia (a painful neck muscle condition) by reducing muscle contractions.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.