Introduction
Brucellosis, a pervasive zoonotic disease, continues to pose significant challenges to global public health and agriculture. Caused by bacteria of the genus Brucella, this infectious disease not only affects a variety of domestic animals but also poses a substantial risk to humans, particularly those in close contact with livestock. The ramifications of brucellosis are far-reaching, often leading to economic losses in agricultural communities due to reduced productivity and increased veterinary costs. Furthermore, the disease's ability to transfer from animals to humans highlights its public health importance, necessitating a thorough understanding of its symptoms, causes, treatment, and preventive measures. This article delves into the multifaceted nature of brucellosis, shedding light on its impact and providing insights into effective management strategies.
What is Brucellosis?
Brucellosis is classified as an infectious disease triggered by bacteria belonging to the genus Brucella. Recognized for its zoonotic nature, this disease predominantly affects livestock, including cattle, goats, sheep, and swine. In terms of geographical distribution, brucellosis remains prevalent in regions with extensive agricultural practices and animal husbandry. Countries in the Mediterranean basin, parts of Asia, Africa, and Latin America report higher incidence rates, highlighting the disease’s widespread reach. Understanding the connection between livestock and brucellosis is crucial, as infected animals act as reservoirs, facilitating the transmission to humans through direct contact or consumption of contaminated animal products. This dual threat underscores the necessity of awareness and preventive measures to curb the spread of brucellosis.
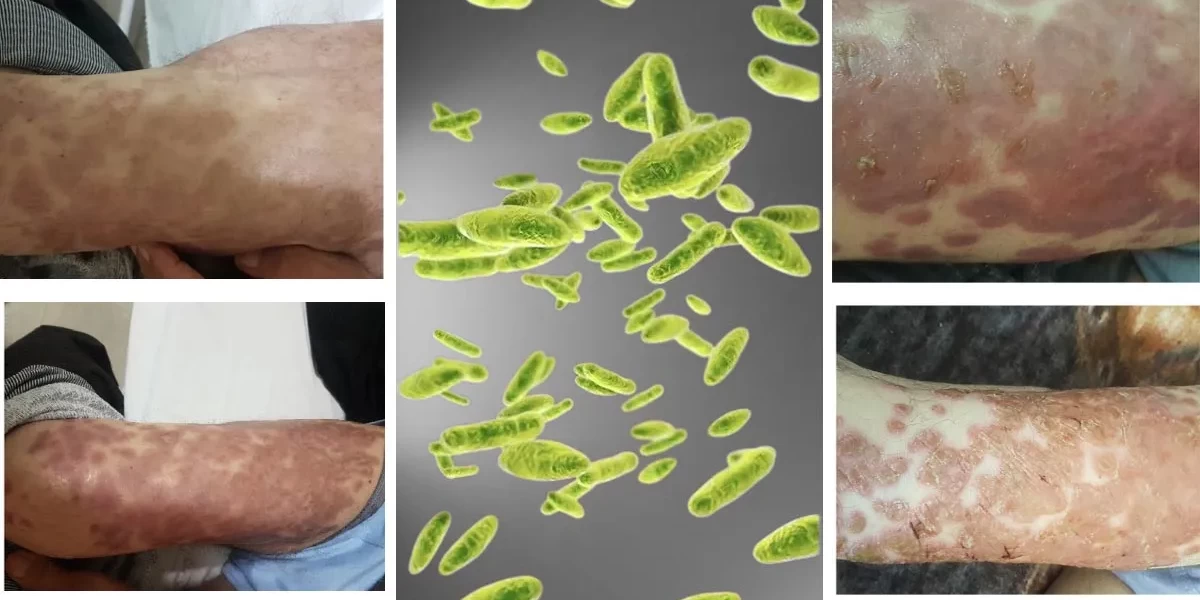
Symptoms of Brucellosis
Brucellosis can present a variety of symptoms, many of which are non-specific and can mimic other illnesses, making diagnosis challenging. The symptoms of brucellosis can be either acute or chronic, with varying degrees of severity depending on the individual and the length of the infection. Here's a closer look at the common symptoms associated with brucellosis:
1. Fever and Sweats
One of the most common symptoms of brucellosis is fever. In fact, the fever experienced by those infected with Brucella bacteria is often referred to as "undulant fever" because it tends to rise and fall over time. This irregular fever pattern can last for several weeks or even months. Alongside fever, patients often experience night sweats, which can be profuse and may even have a distinctive foul odor.
2. Fatigue and Malaise
Another key symptom of brucellosis is extreme fatigue. Those infected with the bacteria often feel physically drained and may struggle with normal daily activities. This fatigue can be accompanied by a general feeling of malaise, where the individual feels unwell without any specific cause. In some cases, this exhaustion can persist even after other symptoms have subsided.
3. Joint and Muscle Pain
Brucellosis often affects the musculoskeletal system, leading to joint and muscle pain. This pain is typically felt in the larger joints, such as the knees, hips, and lower back. In some cases, the inflammation in these joints can become severe enough to cause swelling and restricted movement. Chronic brucellosis can even lead to more permanent joint damage if left untreated.
4. Headache and Neurological Symptoms
Headaches are another common symptom of brucellosis. These can range from mild to severe and may be accompanied by other neurological symptoms such as depression, anxiety, or even cognitive difficulties. In rare cases, brucellosis can lead to complications such as meningitis, which is an infection of the membranes surrounding the brain and spinal cord.
5. Chronic Complications
If left untreated, brucellosis can result in chronic complications, such as recurring fever, joint pain, and fatigue. Some individuals may develop conditions like endocarditis (infection of the heart valves) or osteomyelitis (bone infection). Chronic brucellosis can significantly reduce an individual's quality of life and lead to long-term disability.
Risk Factors
Brucellosis is more common in certain populations due to their occupation, lifestyle, or geographic location. Understanding the risk factors can help in identifying individuals who may be more vulnerable to the infection.
1. Occupational Risk
Certain occupations put individuals at higher risk of contracting brucellosis. Farmers, veterinarians, slaughterhouse workers, and laboratory personnel are more likely to come into contact with infected animals or animal products. These individuals may handle animals that are infected with Brucella bacteria or work in environments where the bacteria are present.
2. Consumption of Unpasteurized Dairy Products
One of the main ways humans contract brucellosis is through the consumption of unpasteurized dairy products. Milk, cheese, and other dairy products that have not been pasteurized can harbor Brucella bacteria, especially if they come from infected animals. In regions where unpasteurized dairy products are commonly consumed, the risk of brucellosis is significantly higher.
3. Geographic Location
Brucellosis is more prevalent in certain parts of the world, particularly in regions where livestock farming is widespread and pasteurization of dairy products is not consistently practiced. Countries in the Mediterranean, the Middle East, South America, and Central Asia report higher rates of brucellosis. Travelers to these regions may also be at risk if they consume local dairy products or come into contact with infected animals.
4. Weakened Immune System
Individuals with weakened immune systems, such as those with HIV/AIDS or individuals undergoing treatments like chemotherapy, are at higher risk of severe brucellosis infections. Their bodies may struggle to fight off the bacteria, leading to more serious complications.
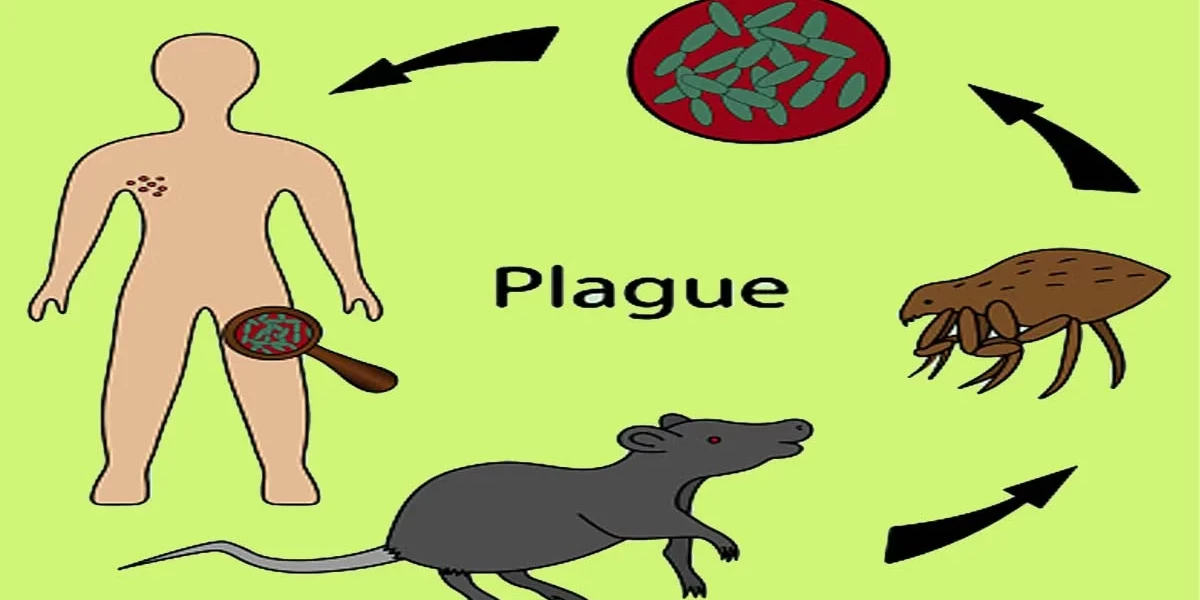
Causes of Brucellosis
Brucellosis is caused by bacteria from the genus Brucella. These bacteria are small, gram-negative coccobacilli that primarily infect animals but can also infect humans.
1. The Brucella Bacteria
There are several species of Brucella bacteria that can cause brucellosis in humans. The most common species include:
- Brucella melitensis (commonly found in sheep and goats)
- Brucella abortus (commonly found in cattle)
- Brucella suis (commonly found in pigs)
- Brucella canis (commonly found in dogs)
Each species is adapted to a specific animal host, but all can be transmitted to humans under the right conditions.
2. Impact on the Body
When Brucella bacteria enter the body, they can spread through the bloodstream and infect various organs, including the liver, spleen, and bones. Once inside the body, the bacteria replicate and evade the immune system, leading to persistent infections that can last for weeks or months if untreated.
3. Transmission Between Animals
Brucellosis is primarily an animal disease. Infected animals can spread the bacteria through their milk, urine, and reproductive fluids. The bacteria can survive outside the host for extended periods, especially in cold and humid environments, increasing the likelihood of transmission to other animals or humans.
How is Brucellosis Transmitted?
Understanding how brucellosis is transmitted is crucial for preventing the spread of the disease, both in humans and animals.
1. Direct Contact with Infected Animals
Humans can contract brucellosis through direct contact with infected animals or their bodily fluids. This is particularly common in individuals who handle livestock, such as farmers or veterinarians. The bacteria can infiltrate the body via cuts or scrapes on the skin, or through the mucous membranes of the eyes, nose, or mouth.
2. Consumption of Contaminated Food or Water
As mentioned earlier, one of the most common routes of transmission is through the consumption of contaminated food or water. Unpasteurized milk or dairy products from infected animals are the main culprits, but contaminated meat or water sources can also pose a risk.
3. Inhalation of Aerosols
Another way brucellosis can be transmitted is through the inhalation of aerosols containing Brucella bacteria. This can happen in environments where the bacteria are present in high concentrations, such as slaughterhouses or laboratories. Inhalation is a less common route of transmission but poses a risk for those working in high-exposure settings.
4. Person-to-Person Transmission
While rare, there have been reports of person-to-person transmission of brucellosis. This can occur through blood transfusions, organ transplants, or even from mother to child during childbirth or breastfeeding.
Complications of Untreated Brucellosis
If brucellosis is not diagnosed and treated promptly, the infection can cause long-term complications. Chronic brucellosis can lead to issues such as arthritis, endocarditis (infection of the heart valves), and inflammation of the liver or spleen. In some cases, it can also affect the nervous system, causing meningitis or other neurological conditions.
The risk of these complications increases the longer the infection remains untreated. Chronic brucellosis can significantly impact a person's quality of life, causing persistent pain, fatigue, and difficulty performing daily activities.
Diagnosis and Tests
Diagnosing brucellosis is challenging because its symptoms mimic many other illnesses. A thorough medical history and examination are essential, especially for those in high-risk occupations or those who have recently traveled to areas where brucellosis is more prevalent.
The two primary diagnostic tests for brucellosis are blood cultures and serological tests. Blood cultures are used to detect the presence of Brucella bacteria in the bloodstream, but the results may take time, and in some cases, the bacteria may not grow well in culture. Serological tests, such as the enzyme-linked immunosorbent assay (ELISA), detect antibodies against Brucella, helping to confirm the diagnosis.
Despite these tests, false negatives can occur, and multiple tests may be needed to confirm the infection. The challenge lies in early detection because delaying diagnosis can lead to prolonged illness and more severe complications.
Management and Treatment
Once diagnosed, brucellosis is treated with a combination of antibiotics. The most common treatment regimen includes doxycycline and rifampin, usually taken for at least six weeks. In more severe cases, other antibiotics like streptomycin or gentamicin may be added to the treatment plan.
The duration of antibiotic therapy is crucial to prevent relapses. Brucellosis is notorious for being a stubborn infection, and incomplete treatment can lead to recurrence. Adhering to the full course of antibiotics is vital, even if symptoms improve before the treatment period ends. Early and consistent treatment can prevent complications and ensure a full recovery.
Challenges in Treating Brucellosis
One of the challenges in treating brucellosis is the potential for antibiotic resistance. Prolonged antibiotic use can also cause side effects, such as gastrointestinal issues or liver problems, making it essential to monitor patients closely during treatment. In some cases, patients may need to switch to alternative antibiotics if they experience severe side effects or if the bacteria show resistance.
Prevention
Preventing brucellosis starts with minimizing exposure to the Brucella bacteria. Vaccinating livestock is one of the most effective strategies for reducing the risk of transmission. Additionally, proper food handling practices, such as pasteurizing milk and thoroughly cooking meat, can prevent infection.
Public health education is critical in raising awareness about brucellosis, especially in high-risk areas. Informing the public about the dangers of consuming unpasteurized dairy products and the importance of vaccinating animals can help reduce the incidence of the disease.
Living With Brucellosis
For individuals diagnosed with brucellosis, managing the disease involves regular follow-up care to monitor for potential complications and to ensure that the infection is fully resolved. Lifestyle adjustments may include taking precautions to avoid spreading the infection to others and adhering to a healthy diet to support recovery.
Long-term management may be required in cases of chronic brucellosis, where individuals need ongoing medical supervision to manage symptoms and prevent relapses. Support from healthcare providers, along with a commitment to following treatment plans, can help patients lead a normal life despite the challenges posed by brucellosis.
Conclusion
Brucellosis is a serious infection that can cause a wide range of symptoms, from fever and fatigue to chronic joint pain and neurological issues. Certain populations, such as farmers and those who consume unpasteurized dairy products, are at higher risk for contracting the disease. By understanding the causes and transmission routes of brucellosis, individuals and public health officials can take steps to prevent its spread.
Frequently Asked Questions(FAQ's)
What is the treatment plan for brucellosis?
- The treatment plan for brucellosis involves a combination of antibiotics to control symptoms and prevent complications. Commonly used antibiotics include doxycycline, rifampin, streptomycin, and gentamicin. Treatment usually lasts for at least six to eight weeks.
What is the drug treatment for Brucella?
- The drug treatment for Brucella involves antibiotics such as doxycycline, rifampin, aminoglycosides (streptomycin or gentamicin), trimethoprim/sulfamethoxazole (TMP-SMX), and quinolones (ciprofloxacin or ofloxacin).
What is the treatment for brucellosis in cattle?
- There is no practical treatment for brucellosis in cattle. Infected cattle are usually quarantined and may be euthanized to prevent the spread of the disease. Prevention measures, such as vaccination and testing, are crucial to control the disease in cattle.
How can brucellosis be prevented?
Brucellosis can be prevented by:
- Consuming only pasteurized milk and dairy products.
- Wearing protective gear (goggles, gloves) when handling potentially infected animals or carcasses.
- Ensuring proper vaccination and testing of livestock.
- Practicing good hygiene and sanitation measures.
What is the recent treatment of brucellosis?
- Recent treatments for brucellosis still rely on a combination of antibiotics, but research is ongoing to find more effective and shorter-duration treatments. Multidrug regimens remain the mainstay of therapy.
Who treats brucellosis?
- Brucellosis is typically treated by infectious disease specialists who specialize in diagnosing and managing infections.
What are the symptoms of brucellosis in cattle?
Symptoms of brucellosis in cattle include:
- Abortion or stillbirths.
- Retained placenta.
- Reduced milk production.
- Infertility.
What are the complications of brucellosis?
Complications of brucellosis can include:
- Endocarditis (infection of the heart lining).
- Arthritis (joint inflammation).
- Chronic fatigue and weakness.
- Infection of the central nervous system.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.