ACE inhibitors are a class of drugs that are widely used to treat high blood pressure, heart failure, and chronic kidney disease. They work by blocking the action of an enzyme called angiotensin-converting enzyme (ACE), which is involved in the regulation of blood pressure and fluid balance in the body. By inhibiting ACE, these drugs reduce the production of a hormone called angiotensin II, which causes blood vessels to narrow and increase blood pressure. As a result, ACE inhibitors lower blood pressure and improve blood flow to the heart and kidneys.
ACE inhibitors have many benefits for patients with cardiovascular and renal conditions, such as reducing the risk of heart attack, stroke, and kidney failure. They also have some side effects, such as cough, low blood pressure, and high potassium levels. Therefore, they should be used with caution in certain situations, such as pregnancy, kidney impairment, and hyperkalemia. In some cases, ACE inhibitors may be combined with other drugs, such as angiotensin II receptor blockers (ARBs) or diuretics, to enhance their effects or reduce their side effects.
This article will provide a comprehensive overview of ACE inhibitors, including their definition, mechanism of action, indications, common types, benefits, side effects, contraindications, precautions, combination therapies, monitoring, and dosage. It will also answer some frequently asked questions about ACE inhibitors.
Understanding ACE
Angiotensin-converting enzyme (ACE) is a protein that is found in various tissues and organs of the body, such as the lungs, kidneys, blood vessels, heart, and brain. It is mainly responsible for converting a peptide called angiotensin I into a hormone called angiotensin II.
Angiotensin II is a key player in the renin-angiotensin-aldosterone system (RAAS), which is a complex hormonal system that regulates blood pressure, fluid balance, and electrolyte levels in the body. The RAAS is activated when the body senses a drop in blood pressure, blood volume, or sodium levels, such as in dehydration, blood loss, or heart failure. The RAAS works by increasing t he production of angiotensin II, which has several effects, such as:
he production of angiotensin II, which has several effects, such as:
- Constricting the blood vessels, which increases the resistance to blood flow and raises blood pressure.
- Stimulating the release of aldosterone, a hormone that causes the kidneys to retain sodium and water, which increases blood volume and blood pressure.
- Increasing the thirst and salt appetite, which leads to more fluid intake and retention, which increases blood volume and blood pressure.
- Enhancing the sympathetic nervous system, which increases the heart rate and contractility, which increases the cardiac output and blood pressure.
By increasing blood pressure and blood volume, the RAAS helps to restore the normal perfusion of vital organs, such as the brain, heart, and kidneys. However, when the RAAS is overactivated or dysregulated, it can cause harmful effects, such as hypertension, heart failure, kidney damage, and vascular inflammation.
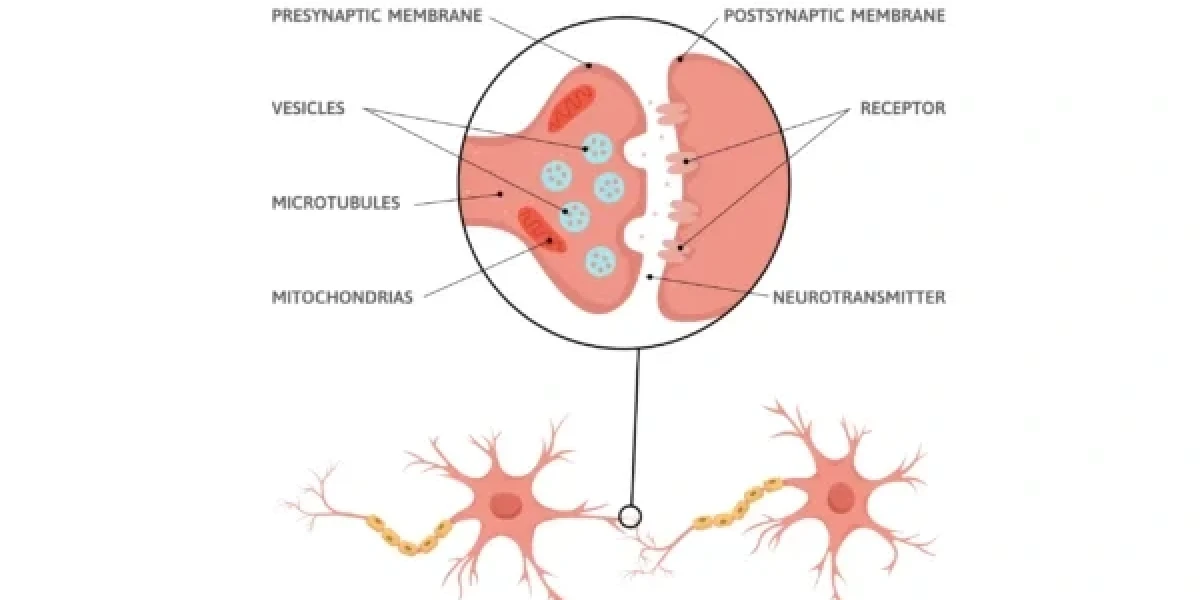
Mechanism of Action
ACE inhibitors are drugs that interfere with the RAAS by blocking the action of ACE. By inhibiting ACE, these drugs prevent the conversion of angiotensin I into angiotensin II, which reduces the levels of angiotensin II in the body. This prompts a few impacts, for example:
- Dilating the blood vessels, which lowers the resistance to blood flow and reduces blood pressure.
- Decreasing the secretion of aldosterone, which reduces the reabsorption of sodium and water by the kidneys, which lowers blood volume and blood pressure.
- Reducing the thirst and salt appetite, which decreases the fluid intake and retention, which lowers blood volume and blood pressure.
- Diminishing the sympathetic nervous system, which lowers the heart rate and contractility, which reduces the cardiac output and blood pressure.
By lowering blood pressure and blood volume, ACE inhibitors help to improve the blood flow to the heart and kidneys, which protects them from damage and improves their function. They also have anti-inflammatory and anti-fibrotic effects, which prevent the remodeling and scarring of the heart and blood vessels.
ACE inhibitors are indicated for the treatment of various cardiovascular and renal conditions, such as:
- Hypertension: ACE inhibitors are effective in lowering blood pressure in patients with hypertension, especially those with high renin levels, such as young, white, or non-obese patients. They are also recommended for patients with hypertension and other risk factors, such as diabetes, chronic kidney disease, or cardiovascular disease. ACE inhibitors can reduce the risk of cardiovascular events, such as heart attack, stroke, and death, in patients with hypertension.
- Heart failure: ACE inhibitors are beneficial in improving the symptoms and survival of patients with heart failure, especially those with reduced ejection fraction (HFrEF), which means that the heart is incapable to siphon sufficient blood to address the body's issues. They can also prevent or delay the progression of heart failure in patients with asymptomatic left ventricular dysfunction (ALVD), which means that the heart is weakened but not yet causing symptoms. ACE inhibitors can reduce the risk of hospitalization and death in patients with heart failure.
- Chronic kidney disease: ACE inhibitors are useful in slowing the decline of kidney function and preventing the development of end-stage renal disease (ESRD) in patients with chronic kidney disease, especially those with proteinuria, which means that there is excess protein in the urine. They can also reduce the risk of cardiovascular complications in patients with chronic kidney disease.
Common ACE Inhibitors
There are many types of ACE inhibitors available in the market, which differ in their chemical structure, pharmacokinetics, potency, and duration of action. Some of the common ACE inhibitors are:
- Enalapril: Enalapril is a prodrug, which means that it is inactive until it is converted into its active form, enalaprilat, by the liver. It has a half-life of about 11 hours and is excreted by the kidneys. It is available in oral tablets or injections. The usual dose range is 2.5 to 40 mg per day, divided into one or two doses.
- Lisinopril: Lisinopril is an active drug, which means that it does not need to be converted into another form by the body. It has a half-life of about 12 hours and is excreted by the kidneys. It is available in oral tablets. The usual dose range is 5 to 40 mg per day, taken once a day.
- Ramipril: Ramipril is a prodrug, which means that it is inactive until it is converted into its active form, ramiprilat, by the liver. It has a half-life of about 13 hours and is excreted by the kidneys and the bile. It is available in oral capsules or tablets. The usual dose range is 1.25 to 10 mg per day, taken once or twice a day.
- Captopril: Captopril is an active drug, which means that it does not need to be converted into another form by the body. It has a half-life of about 2 hours and is excreted by the kidneys. It is available in oral tablets. The usual dose range is 12.5 to 150 mg per day, divided into two or three doses.
Benefits and Side Effects
ACE inhibitors have many benefits for patients with cardiovascular and renal conditions, such as:
- Cardiovascular benefits: ACE inhibitors can lower blood pressure, improve blood flow to the heart, reduce the workload of the heart, prevent or reverse the remodeling and scarring of the heart and blood vessels, and decrease the risk of heart attack, stroke, and death.
- Renal protection: ACE inhibitors can protect the kidneys from damage caused by high blood pressure, diabetes, or other diseases, by reducing the pressure and proteinuria in the glomeruli, which are the filtering units of the kidneys. They can also delay the progression of chronic kidney disease and prevent the development of end-stage renal disease.
However, ACE inhibitors also have some side effects, such as:
- Cough: ACE inhibitors can cause a dry, persistent, and irritating cough in some patients, which may interfere with their quality of life and adherence to the treatment. The cough is due to the accumulation of bradykinin, a peptide that is normally degraded by ACE, in the lungs. The cough usually occurs within the first few weeks of starting the treatment and may resolve spontaneously or after discontinuing the drug. The cough is more common in women, smokers, and patients with asthma or allergies.
- Low blood pressure: ACE inhibitors can cause a sudden drop in blood pressure, especially in the first few doses or after increasing the dose, which may cause dizziness, fainting, or falls. The low blood pressure is due to the vasodilation and fluid loss caused by the drug. The low blood pressure is more likely in patients who are dehydrated, have low sodium levels, or are taking other blood pressure-lowering drugs, such as diuretics or nitrates. The low blood pressure can be prevented by starting with a low dose, increasing the dose gradually, and monitoring the blood pressure regularly.
- High potassium levels: ACE inhibitors can cause an increase in potassium levels in the blood, which may cause muscle weakness, irregular heartbeat, or cardiac arrest. The high potassium levels are due to the reduced secretion of aldosterone, which normally regulates the potassium balance in the body. The high potassium levels are more common in patients who have kidney impairment, diabetes, or heart failure, or are taking other drugs or supplements that increase potassium levels, such as potassium-sparing diuretics, angiotensin II receptor blockers, non-steroidal anti-inflammatory drugs, or potassium supplements. The high potassium levels can be prevented by monitoring the potassium levels regularly and avoiding excess potassium intake.
Contraindications and Precautions
ACE inhibitors are contraindicated in some situations, such as:
- Pregnancy: ACE inhibitors can cause fetal harm, such as growth retardation, kidney failure, skull defects, or death, if taken during pregnancy, especially in the second and third trimesters. Therefore, they should not be used by pregnant women or women who plan to become pregnant. If pregnancy is detected, the drug should be discontinued as soon as possible and alternative therapy should be initiated.
- Hyperkalemia: ACE inhibitors can worsen hyperkalemia, which is a condition of abnormally high potassium levels in the blood, which can cause life-threatening arrhythmias or cardiac arrest. Therefore, they should not be used by patients who have hyperkalemia or are at risk of developing it, such as those with kidney impairment, diabetes, heart failure, or taking other drugs or supplements that increase potassium levels.
- Kidney impairment: ACE inhibitors can impair the kidney function in some patients, especially those who have bilateral renal artery stenosis, which is a narrowing of the arteries that supply blood to the kidneys, or those who have severe dehydration, low blood pressure, or heart failure. Therefore, they should be used with caution and under close supervision by patients who have kidney impairment or are at risk of developing it, such as those with diabetes, hypertension, or chronic kidney disease. The kidney function should be monitored regularly and the dose should be adjusted accordingly.
Combination Therapies
ACE inhibitors may be combined with other drugs to enhance their effects or reduce their side effects, such as:
- ACE inhibitors and angiotensin II receptor blockers (ARBs): ARBs are another class of drugs that interfere with the RAAS by blocking the action of angiotensin II on its receptors. They have similar effects and indications as ACE inhibitors, but they do not cause cough or increase potassium levels. In some cases, ACE inhibitors and ARBs may be used together to achieve better blood pressure control or kidney protection, especially in patients who have resistant hypertension, heart failure, or chronic kidney disease. However, this combination may also increase the risk of low blood pressure, kidney impairment, or hyperkalemia, and should be used with caution and under close monitoring.
- ACE inhibitors and diuretics: Diuretics are drugs that increase the urine output and reduce the fluid retention in the body. They are often used to treat high blood pressure, heart failure, or edema. They can enhance the blood pressure-lowering effect of ACE inhibitors, but they can also cause low blood pressure, low sodium levels, or low potassium levels. Therefore, they should be used with caution and under close monitoring in combination with ACE inhibitors.
Monitoring and Dosage
ACE inhibitors require regular monitoring and dosage adjustments to ensure their safety and efficacy, such as:
- Regular blood pressure monitoring: ACE inhibitors can lower blood pressure, which is beneficial for patients with hypertension, heart failure, or chronic kidney disease. However, they can also cause low blood pressure, which can be dangerous for some patients, especially those who are dehydrated, have low sodium levels, or are taking other blood pressure-lowering drugs. Therefore, the blood pressure should be checked before starting the treatment, after each dose change, and periodically during the treatment. The blood pressure goal and the dose should be individualized according to the patient’s condition and response to the drug.
- Individualized dosage adjustments: ACE inhibitors have different pharmacokinetics, potency, and duration of action, which affect their dosing and frequency. The dose and frequency should be tailored to the patient’s condition, response, and tolerance to the drug. The dose should be started low and increased gradually until the desired effect is achieved or the maximum dose is reached. The dose should be reduced or discontinued if the patient experiences adverse effects, such as low blood pressure, high potassium levels, or kidney impairment.
Conclusion
ACE inhibitors are a class of drugs that are widely used to treat high blood pressure, heart failure, and chronic kidney disease. They work by blocking the action of ACE, which reduces the production of angiotensin II, which lowers blood pressure and improves blood flow to the heart and kidneys. They have many benefits for patients with cardiovascular and renal conditions, such as reducing the risk of heart attack, stroke, and kidney failure. They also have some side effects, such as cough, low blood pressure, and high potassium levels. They should be used with caution in certain situations, such as pregnancy, hyperkalemia, or kidney impairment. They may be combined with other drugs, such as ARBs or diuretics, to enhance their effects or reduce their side effects. They require regular monitoring and dosage adjustments to ensure their safety and efficacy.
FAQ
- What are the differences between ACE inhibitors and ARBs?
- ACE inhibitors and ARBs are both drugs that interfere with the RAAS, but they have different mechanisms of action. ACE inhibitors block the action of ACE, which prevents the conversion of angiotensin I into angiotensin II, while ARBs block the action of angiotensin II on its receptors. They have similar effects and indications, but they have different side effects. ACE inhibitors can cause cough or increase potassium levels, while ARBs do not. ARBs can cause angioedema, which is a swelling of the face, lips, tongue, or throat, while ACE inhibitors do not.
- Can I take ACE inhibitors with alcohol?
- ACE inhibitors can interact with alcohol, which can increase the risk of low blood pressure, dizziness, or fainting. Therefore, it is advisable to limit or avoid alcohol consumption while taking ACE inhibitors. If you drink alcohol, you should do so moderately and with caution, and monitor your blood pressure and symptoms closely.
- Can I take ACE inhibitors with grapefruit juice?
- ACE inhibitors can interact with grapefruit juice, which can affect their absorption, metabolism, and excretion. This can alter their blood levels and effects, which can be either increased or decreased. Therefore, it is advisable to avoid or limit grapefruit juice consumption while taking ACE inhibitors. If you drink grapefruit juice, you should do so at least 4 hours before or after taking ACE inhibitors, and monitor your blood pressure and symptoms closely.
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.