1. Introduction
Blood transfusions are one of the most vital medical procedures in modern healthcare, playing a pivotal role in saving lives and improving the quality of care for patients facing critical health conditions. A blood transfusion is the process of transferring blood or blood products from one person (the donor) into the circulatory system of another person (the recipient). This procedure is often necessary in situations where a patient’s blood volume, red blood cells, or specific blood components have been significantly depleted due to surgery, injury, or disease.
The significance of blood transfusions cannot be overstated. For example, in trauma cases, patients who lose large amounts of blood during accidents or surgeries rely on transfusions to replace the lost volume and prevent shock. In cancer treatments, blood transfusions help replenish red blood cells or platelets that chemotherapy or radiation may reduce. This procedure is also crucial for patients with chronic conditions such as sickle cell anemia or hemophilia, who often require ongoing transfusions to manage their symptoms.
Beyond emergency and chronic care, blood transfusions have become routine procedures in hospitals worldwide. They enhance patient survival rates, aid in recovery from complex medical treatments, and offer critical support during surgical procedures. This introduction to blood transfusions sets the stage for a more detailed exploration of the different types of transfusions, each uniquely designed to meet specific medical needs.

2. Types of Blood Transfusions
There are several types of blood transfusions, each catering to particular medical conditions and patient needs. The four primary types are whole blood transfusions, red blood cell transfusions, platelet transfusions, and plasma transfusions. Each type serves a different purpose, ensuring that patients receive the precise care required to address their health concerns.
Whole Blood Transfusions
Whole blood transfusions involve transferring blood that contains all its components—red blood cells, white blood cells, plasma, and platelets. This type of transfusion is less common today but is still used in certain emergency situations, such as massive blood loss due to trauma or surgery. Whole blood transfusions are typically reserved for situations where a patient needs all components of blood, not just a specific element. It is particularly useful in restoring blood volume quickly in life-threatening cases.
Red Blood Cell Transfusions
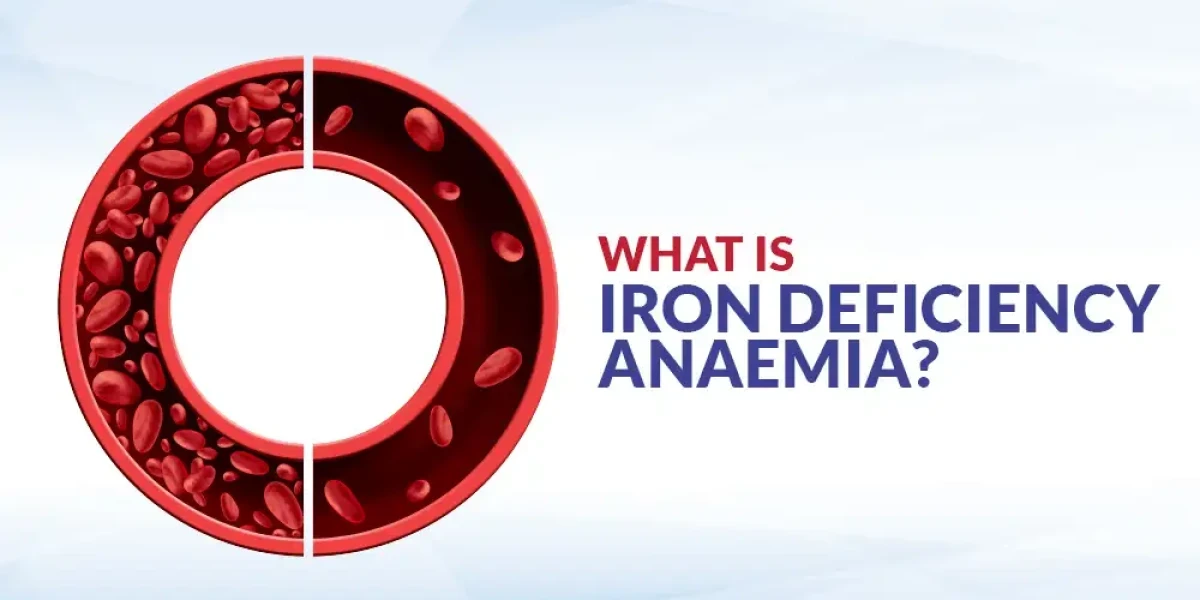
Red blood cell (RBC) transfusions are the most common type of blood transfusion. These transfusions are primarily used to treat anemia, a condition in which the body lacks sufficient healthy red blood cells to carry adequate oxygen to the tissues. Conditions like chronic kidney disease, bone marrow disorders, or severe blood loss can lead to a reduction in red blood cells, making RBC transfusions critical. By increasing the number of red blood cells in the bloodstream, these transfusions help restore normal oxygen levels in the body, improving energy, strength, and overall function for the patient.
Platelet Transfusions
Platelets play a crucial role in blood clotting, preventing excessive bleeding during injuries. Platelet transfusions are often required for patients who suffer from conditions that deplete platelet counts, such as leukemia, chemotherapy-induced bone marrow suppression, or certain autoimmune disorders. Without sufficient platelets, patients are at risk of uncontrolled bleeding, even from minor cuts or bruises. Platelet transfusions are particularly crucial before surgery or invasive procedures in patients with low platelet levels, ensuring that their blood can clot properly during and after the procedure.
Plasma Transfusions
Plasma is the liquid part of blood that contains important proteins like clotting factors and antibodies. Plasma transfusions are used to treat patients with liver disease, severe infections, or burns, where clotting factors are deficient. Patients who take medications like warfarin, which affect clotting ability, may also require plasma transfusions in emergency situations where rapid reversal of anticoagulation is necessary. Plasma transfusions help restore the body’s ability to clot blood properly, preventing excessive bleeding in critical cases.
3. Why Are Blood Transfusions Necessary?
Blood transfusions are life-saving interventions that are necessary in a wide range of medical conditions and emergencies. These include situations where the body's blood supply is critically low, or where specific components of blood (like red blood cells, platelets, or plasma) need replenishing to ensure proper bodily function. Transfusions can be required due to severe anemia, trauma, surgical procedures, and certain medical treatments, all of which can severely deplete a person’s blood supply and compromise their ability to carry oxygen and nutrients to tissues.
One of the most common reasons for blood transfusions is severe anemia. Anemia happens when the body doesn't have enough red blood cells to transport oxygen to tissues. This can be caused by chronic illnesses such as kidney disease, cancer, or bone marrow disorders, but it can also result from acute situations like heavy bleeding. Blood transfusions help restore red blood cells, improving oxygen transport and boosting energy levels in patients suffering from anemia.
Trauma and accidents are other critical situations where blood transfusions become vital. In cases of severe injury—especially those involving significant blood loss, such as car accidents or severe lacerations—the body may not be able to replace lost blood quickly enough to maintain normal functioning. Without a transfusion, the patient’s organs could fail due to lack of oxygen, potentially leading to death. By providing fresh blood, transfusions help stabilize the patient’s condition and support their recovery.
Surgical procedures, especially major ones such as heart surgeries, joint replacements, or organ transplants, often require blood transfusions. During surgery, blood loss is inevitable, and replacing this blood is essential to maintaining adequate blood volume and pressure. Certain cancer treatments, including chemotherapy, can also damage the body’s ability to produce blood cells, leading to a need for transfusions to restore proper levels of red blood cells, white blood cells, or platelets.
The life-saving potential of blood transfusions cannot be overstated. They play a crucial role in improving patient outcomes and recovery in a wide variety of medical situations. Whether it’s restoring lost blood after trauma or helping cancer patients recover from treatments, transfusions are a cornerstone of modern medical care. Moreover, they provide a temporary but critical bridge, giving the body time to heal while restoring essential blood components.
4. Blood Transfusion Procedure

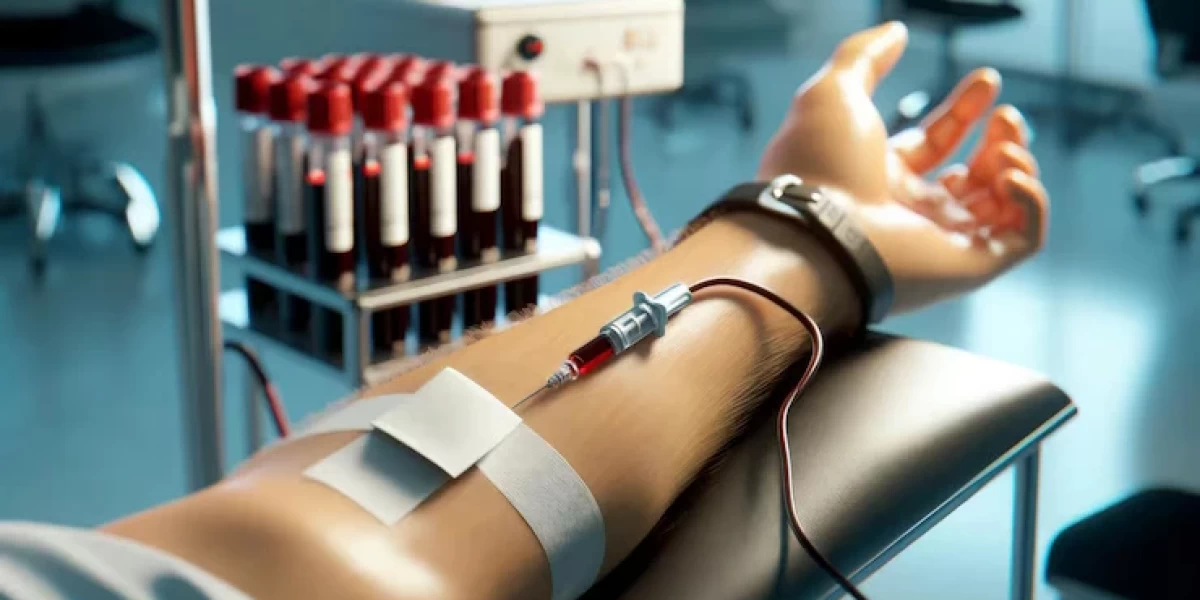
A blood transfusion is a carefully monitored medical procedure that involves multiple steps to ensure safety and compatibility. The process begins with an initial assessment, where healthcare providers evaluate the patient’s condition and determine the need for a transfusion. This is followed by blood type matching, a critical step that ensures the donor blood is compatible with the patient’s blood type to avoid dangerous immune reactions.
Before the transfusion, the patient undergoes blood tests to check their hemoglobin levels, blood type (ABO and Rh factor), and sometimes additional screenings to ensure that no harmful antibodies are present. This step is essential because incompatible blood transfusions can lead to serious complications, including hemolysis, where the immune system attacks the transfused blood cells. This makes precise blood typing and cross-matching vital parts of the process.
Once compatibility is confirmed, the transfusion is ready to begin. Healthcare professionals prepare the donor blood by labeling it with all necessary information and checking it thoroughly for contaminants or signs of infection. The actual transfusion typically takes place in a hospital setting or outpatient clinic under the supervision of nurses and doctors. The blood is administered intravenously, usually through a small catheter inserted into the patient's vein. The rate of transfusion depends on the patient’s condition and the volume of blood being administered, but a typical transfusion can take anywhere from 1 to 4 hours.
During the transfusion, the patient’s vital signs—such as heart rate, blood pressure, and temperature—are closely monitored to detect any signs of adverse reactions. In some cases, patients may experience mild symptoms like chills, fever, or rash, but serious reactions are rare due to rigorous safety protocols. Blood safety standards are high in most healthcare systems, with blood donations being tested for infectious diseases such as HIV, hepatitis, and syphilis.
At the conclusion of the transfusion, healthcare providers assess the patient to ensure they are stable and that the transfusion has had the desired effect. Depending on the situation, patients may require multiple transfusions over time, especially if they have chronic conditions that affect blood production, such as leukemia or sickle cell disease.
5. Before a Blood Transfusion
Before a blood transfusion, there are several preparatory steps taken to ensure the process is safe and effective for the patient. This begins with a thorough evaluation of the patient's medical history and current condition. The doctor will review any past blood transfusions, allergies, or reactions to ensure there are no contraindications. Blood tests are then conducted to determine the patient’s exact blood type, including the ABO group and Rh factor, which are critical for matching donor blood.
Another important step is obtaining informed consent from the patient. The healthcare provider will explain why the transfusion is necessary, what the procedure entails, and any potential risks involved. This discussion allows the patient to voice any concerns, ask questions, and provide consent. In some cases, patients may refuse a blood transfusion due to personal, religious, or cultural beliefs. In these instances, alternative treatments or strategies may be considered, although transfusion remains the most effective option in many cases.
Communication between the healthcare provider and the patient is crucial during this stage. Patients need to understand the potential benefits of the transfusion—such as improved oxygen levels, better energy, and faster recovery—as well as the risks, including the rare chance of adverse reactions like fever, allergic reactions, or infection. Patient education plays a key role in alleviating fears and ensuring that they feel comfortable with the procedure.
If the patient has any existing health conditions—such as heart disease or kidney problems—these are carefully considered before the transfusion, as some conditions may increase the risk of complications. Additional blood tests may be performed to screen for these risks. Furthermore, depending on the patient’s health status, medications may be administered before the transfusion to prevent allergic reactions or other potential issues.
In emergency situations, when blood transfusions must be given quickly, such as after an accident or severe trauma, the preparatory steps may be streamlined. In such cases, O-negative blood, known as the universal donor, may be used to ensure the patient receives blood quickly without waiting for detailed matching.
6. After a Blood Transfusion
After a blood transfusion, post-transfusion care is essential to ensure that the patient responds well to the treatment and that no adverse reactions occur. Immediately following the transfusion, the patient is monitored closely for any signs of complications. These may include fever, rash, shortness of breath, or chest pain, which can indicate an allergic reaction or other issues. While most transfusions are completed without problems, monitoring is critical to catch any issues early and respond appropriately.
Patients typically stay under observation for at least a few hours after the transfusion to ensure they are stable. Vital signs—such as blood pressure, heart rate, and oxygen levels—are checked regularly during this period. Any unusual symptoms are reported to the healthcare team, who can provide interventions as needed.
The patient’s overall condition is evaluated through follow-up blood tests, which assess whether the transfusion successfully improved hemoglobin levels or corrected any deficiencies. Depending on the reason for the transfusion, further treatments may be required. For instance, patients undergoing chemotherapy or radiation therapy may need additional transfusions to maintain healthy blood cell levels.
In the days following the transfusion, healthcare providers typically schedule follow-up visits to check the patient’s progress. They will review the effectiveness of the transfusion in addressing the underlying condition, such as anemia or blood loss, and determine whether further interventions are necessary.
The patient is also encouraged to report any delayed reactions that may occur after leaving the hospital. Although rare, some reactions to transfusions, such as delayed hemolytic reactions, may not manifest until days or weeks later. Symptoms like jaundice, dark urine, or fatigue should be reported immediately.
7. Blood Transfusion Risks
Blood transfusions are essential, life-saving procedures used in medical settings to replace lost blood during surgery, after trauma, or due to severe anemia. However, as with any medical procedure, they involve potential risks. While the majority of transfusions occur without complications, it's important to be aware of the possible adverse effects, even though serious incidents are rare.
One of the most common risks associated with blood transfusions is allergic reactions. These can occur when the recipient's immune system reacts to proteins in the donor blood. Symptoms typically include itching, hives, and in rare cases, anaphylaxis—a severe allergic reaction that requires immediate medical attention. Febrile non-hemolytic reactions are another common issue, characterized by fever and chills during or shortly after the transfusion. These reactions, though uncomfortable, are usually mild and can be managed effectively with antipyretics.
More serious complications, such as infections, are extremely rare thanks to rigorous screening and testing of donated blood. Infections from blood transfusions occur in less than 1 in 1.5 million transfusions for diseases like hepatitis or HIV. Modern blood banks adhere to strict protocols to minimize these risks, ensuring that the blood supply is as safe as possible.
One of the most serious but rare complications is Transfusion-Related Acute Lung Injury (TRALI). TRALI is a life-threatening condition that leads to sudden lung failure, typically within six hours of the transfusion. It occurs in approximately 1 in 5,000 transfusions, and while its exact cause is still being studied, it is thought to be related to antibodies in the donor blood interacting with the recipient’s immune system. TRALI requires immediate treatment, often in an intensive care setting, but with prompt intervention, most patients recover fully.
Other potential risks include transfusion-associated circulatory overload (TACO), which can occur when too much blood is transfused too quickly, leading to fluid overload and respiratory distress, especially in patients with heart or kidney conditions.
Overall, while blood transfusion risks do exist, they are carefully managed by healthcare providers. The U.S. Centers for Disease Control and Prevention (CDC) notes that severe complications occur in less than 0.01% of transfusions, reinforcing that the procedure is largely safe.
8. Benefits of Blood Transfusions
Despite the potential risks, the benefits of blood transfusions far outweigh the drawbacks, particularly in critical care settings. Blood transfusions are pivotal in saving lives, improving recovery, and enhancing the quality of life for countless patients. The primary benefit is improved oxygen delivery. Red blood cells play a key role in delivering oxygen across the body. In cases of severe blood loss or anemia, a transfusion restores the body's ability to circulate oxygen efficiently, preventing organ failure and death.
Another significant benefit is seen in post-surgical recovery. After major surgeries, particularly those involving significant blood loss like heart surgery or organ transplants, transfusions help restore blood volume and stability. This aids in quicker recovery, reduced complications, and lower rates of post-operative infections. In fact, studies show that patients receiving blood transfusions during surgery have a significantly higher survival rate, as their bodies are better equipped to heal and respond to surgical stress.
Blood transfusions are also critical in the treatment of chronic conditions like sickle cell disease and certain cancers. For patients undergoing chemotherapy, which can deplete red blood cells, transfusions help replenish their blood supply, improving energy levels and reducing fatigue. For those with sickle cell disease, regular blood transfusions help prevent pain episodes and reduce the risk of stroke by diluting the sickled cells in their bloodstream.
In emergency settings, such as after a traumatic injury or accident, rapid blood transfusions can mean the difference between life and death. In fact, transfusions administered within the first hour of trauma (the so-called "golden hour") drastically increase the chances of survival. According to the World Health Organization (WHO), blood transfusions reduce mortality in trauma patients by up to 30%, showcasing their life-saving power.
The benefits of blood transfusions also extend to individuals undergoing childbirth. Severe postpartum hemorrhage can occur during or after delivery, and blood transfusions can help manage this life-threatening condition, significantly improving maternal outcomes.
In conclusion, the life-saving benefits of blood transfusions—from improving oxygen delivery to boosting recovery in critical cases—highlight their indispensable role in modern healthcare.
9. What Kind of Reactions Can Happen from a Blood Transfusion?
Reactions to blood transfusions can vary from mild to severe, but most are manageable with prompt medical attention. The most common reaction is the febrile non-hemolytic reaction, where the patient develops a fever, often accompanied by chills, during or shortly after the transfusion. This reaction is usually a result of the body's response to white blood cells in the donor blood and can be treated with antipyretics such as acetaminophen.
Allergic reactions are another possibility. These are typically mild and manifest as itching or hives. In rare cases, a more severe allergic reaction known as anaphylaxis can occur, causing difficulty breathing, low blood pressure, and swelling. Anaphylaxis is a medical crisis that demands immediate treatment with epinephrine and other supportive interventions.
More serious reactions include hemolytic reactions, which occur when the immune system attacks the transfused red blood cells. This can happen when there is an incompatibility between the donor and recipient blood types. Symptoms of hemolytic reactions include fever, chest pain, back pain, and dark urine. Fortunately, with meticulous blood type matching, hemolytic reactions are exceedingly rare.
One of the rarest and most severe reactions is Transfusion-Related Acute Lung Injury (TRALI). As mentioned earlier, TRALI can lead to sudden lung failure, typically within six hours of the transfusion. Symptoms include difficulty breathing, low blood oxygen levels, and fluid buildup in the lungs. TRALI is a medical emergency that requires immediate attention and often intensive care support.
Delayed hemolytic reactions can also occur, typically days or weeks after the transfusion. These reactions happen when the body slowly starts to break down the transfused red blood cells. While not as immediately dangerous as acute hemolytic reactions, they can still cause significant complications, including jaundice and anemia.
Finally, patients may experience iron overload, particularly those who receive frequent transfusions, such as individuals with sickle cell disease or thalassemia. Excess iron from multiple transfusions can accumulate in the organs, particularly the heart and liver, leading to complications. Regular monitoring and treatments like chelation therapy can help manage this condition.
In summary, while reactions to blood transfusions can occur, healthcare professionals are well-equipped to manage them. Most reactions are mild and treatable, and strict screening processes significantly reduce the risk of more serious complications.
10. Conclusion
Blood transfusions are a cornerstone of modern medicine, offering life-saving benefits in emergency, surgical, and chronic care situations. While there are potential risks involved, the careful management of transfusion procedures and rigorous blood screening make serious complications extremely rare. The benefits, including improved oxygen delivery, enhanced post-surgery recovery, and increased survival rates, are immense and have a profound impact on patient outcomes.
Understanding both the risks and benefits of blood transfusions helps foster a greater appreciation for this critical medical procedure. As medical advancements continue, blood transfusions will remain an essential tool in healthcare, offering hope and healing to millions around the world.
Frequently Asked Questions(FAQ's)
- What does a blood transfusion do?
- A blood transfusion provides blood or blood components to replace what has been lost due to injury, surgery, or certain medical conditions. It helps restore healthy blood cells, clotting factors, or other essential components to the patient's circulation.
- How long do blood transfusions take?
- A blood transfusion typically takes between 1 to 4 hours, depending on the amount of blood needed and the specific components being transfused.
- What does it mean to give a blood transfusion?
- Giving a blood transfusion means transferring blood or blood components from a donor into a patient's bloodstream through an intravenous line (IV) to replace or supplement their own blood.
- What are the signs that you need a blood transfusion?
- Signs that you might need a blood transfusion include active bleeding, low hemoglobin levels (anemia), low platelet count (thrombocytopenia), and low white blood cell count.
- Who needs blood transfusion?
- People who need blood transfusions include those who have lost blood due to injury or surgery, individuals with certain medical conditions like anemia, cancer, hemophilia, or sickle cell disease, and those undergoing treatments that affect blood production.
- Is blood transfusion painful?
- The actual transfusion is not painful. You might feel a sharp prick when the needle is first inserted, but the transfusion itself is painless.
- What is the biggest risk of blood transfusion?
- The biggest risk of a blood transfusion is a reaction to the transfused blood, which can include allergic reactions, fever, or more severe complications like transfusion-related acute lung injury (TRALI) or hemolytic reactions.
- How much does a blood transfusion cost?
- The cost of a blood transfusion can vary widely depending on factors like location, hospital, and the specific components needed. It can range from a few hundred to several thousand dollars.
- What are the side effects of blood transfusion?
- Side effects of a blood transfusion can include mild reactions like fever, chills, or rash, as well as more serious complications like allergic reactions, infections, or lung injury.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.