Acetylcholine (ACh) is a chemical messenger that plays a vital role in the functioning of the nervous system. It is involved in various processes such as transmitting nerve impulses, regulating heart rate, controlling gastrointestinal functions, and facilitating memory and learning. Acetylcholine also has implications in several neurological disorders, such as Alzheimer’s disease and Parkinson’s disease, and can be affected by various medications. In this article, we will explore the structure, function, regulation, and medical relevance of acetylcholine, as well as the current research and future directions in this field.
Introduction
Acetylcholine is an organic compound that belongs to the class of molecules called neurotransmitters. Neurotransmitters are substances that carry signals between neurons (nerve cells) and other cells in the body. Acetylcholine is one of the most abundant and widely distributed neurotransmitters in the nervous system, and the only one that is used in both the central nervous system (CNS) and the peripheral nervous system (PNS).
Significance in the nervous system
Acetylcholine is essential for the communication and coordination of the nervous system. It mediates various functions such as sensory perception, motor control, attention, arousal, sleep, and cognition. Acetylcholine also modulates the activity of other neurotransmitters, such as dopamine, serotonin, and norepinephrine, and influences the release of hormones, such as cortisol and insulin.
Historical background
Acetylcholine was first discovered in 1914 by Henry Hallett Dale, who isolated it from animal tissues and showed that it mimicked the effects of stimulating the vagus nerve, which is responsible for slowing down the heart rate. In 1921, Otto Loewi demonstrated that acetylcholine was released from the vagus nerve and acted on the heart muscle cells, thus proving that it was a neurotransmitter. In 1936, Dale and Loewi shared the Nobel Prize in Physiology or Medicine for their discoveries. Since then, acetylcholine has been extensively studied and found to have multiple roles in the nervous system and beyond.
Structure of Acetylcholine
Chemical composition
Acetylcholine is composed of two parts: an acetyl group (CH3CO) and a choline group (CH2CH2N+(CH3)3). The acetyl group is derived from acetyl-CoA, a molecule that is involved in energy metabolism, and the choline group is derived from dietary sources, such as eggs, milk, and liver. The acetyl group and the choline group are joined by an ester bond, which makes acetylcholine a type of ester.
Molecular structure
Acetylcholine has a simple molecular structure, with a molecular formula of C7H16NO2 and a molecular weight of 146.2 g/mol. It has a tetrahedral shape, with four bonds around the central nitrogen atom. The nitrogen atom has a positive charge, which makes acetylcholine a quaternary ammonium compound. The oxygen atom of the acetyl group has a double bond, which makes acetylcholine a carboxylic acid ester.
Synthesis and breakdown
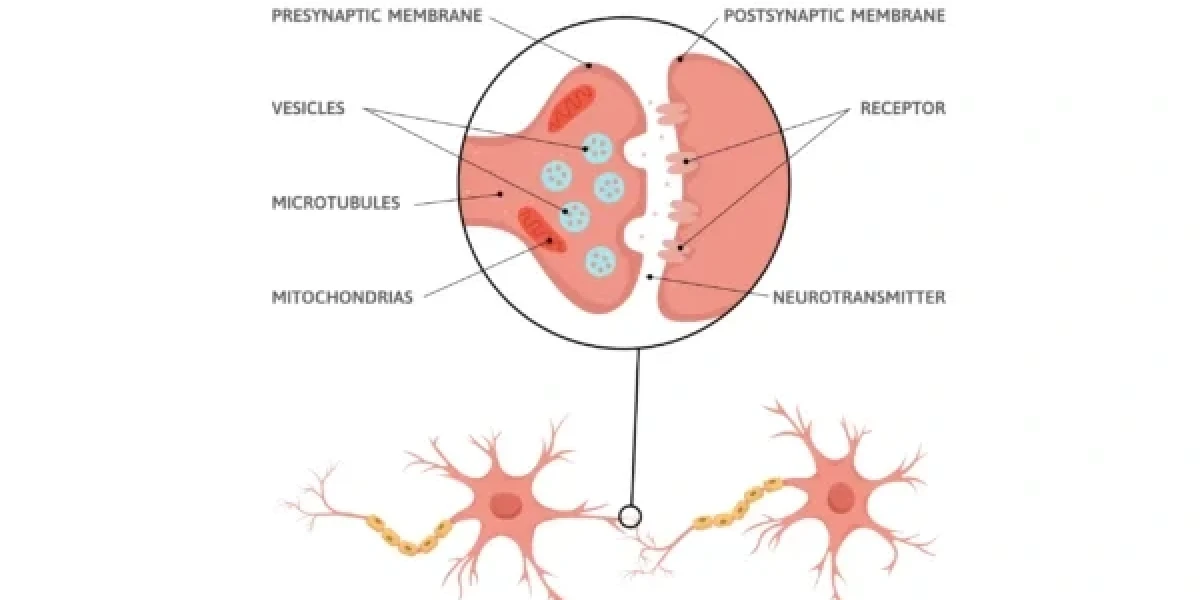
Acetylcholine is synthesized in the cytoplasm of the presynaptic neuron (the neuron that releases the neurotransmitter) by the enzyme choline acetyltransferase (ChAT), which transfers the acetyl group from acetyl-CoA to the choline group. The resulting acetylcholine is then stored in vesicles (small sacs) in the presynaptic terminal, ready to be released when the neuron is stimulated.
Acetylcholine is broken down in the synaptic cleft (the space between the presynaptic and postsynaptic neurons) by the enzyme acetylcholinesterase (AChE), which hydrolyzes the ester bond and splits acetylcholine into acetate and choline. The acetate is recycled into acetyl-CoA, and the choline is taken up by the presynaptic neuron via a transporter protein, to be reused for acetylcholine synthesis.
Functions of Acetylcholine
Neurotransmitter role
Acetylcholine acts as a neurotransmitter in both the CNS and the PNS, where it carries signals from one neuron to another, or from a neuron to a target cell, such as a muscle cell or a gland cell. Acetylcholine is released from the presynaptic neuron when an action potential (an electrical impulse) reaches the presynaptic terminal, causing the vesicles to fuse with the membrane and release their contents into the synaptic cleft. Acetylcholine then binds to specific receptors on the postsynaptic cell, triggering a response that depends on the type and location of the receptor.
Transmission of nerve impulses
Acetylcholine is involved in the transmission of nerve impulses in various pathways and circuits in the CNS and the PNS. For example, acetylcholine is involved in:
- The somatic nervous system, which controls voluntary movements of the skeletal muscles. Acetylcholine is released from the motor neurons that innervate the muscle fibers, causing them to contract.
- The autonomic nervous system, which regulates involuntary functions of the internal organs, such as the heart, lungs, blood vessels, digestive system, and urinary system. Acetylcholine is released from the preganglionic neurons that synapse with the postganglionic neurons in the autonomic ganglia, as well as from the postganglionic neurons that innervate the target organs, depending on the branch of the autonomic nervous system.
- The sensory nervous system, which conveys information from the sensory receptors, such as the eyes, ears, nose, tongue, and skin, to the brain. Acetylcholine is released from the sensory neurons that synapse with the interneurons or the projection neurons in the spinal cord or the brainstem, as well as from the projection neurons that relay the information to the higher brain regions, such as the thalamus, the cortex, and the limbic system.
Neuromuscular junction communication
Acetylcholine is the primary neurotransmitter at the neuromuscular junction, which is the synapse between a motor neuron and a skeletal muscle fiber. Acetylcholine is released from the motor neuron when an action potential reaches the presynaptic terminal, causing the vesicles to fuse with the membrane and release their contents into the synaptic cleft. Acetylcholine then binds to nicotinic receptors on the muscle fiber, causing them to open and allow sodium and potassium ions to flow across the membrane. This depolarizes the muscle fiber, triggering an action potential that propagates along the muscle fiber and causes it to contract.
Involvement in the parasympathetic nervous system
Acetylcholine is the main neurotransmitter of the parasympathetic nervous system, which is the branch of the autonomic nervous system that is responsible for the “rest and digest” functions of the body. The parasympathetic nervous system counteracts the effects of the sympathetic nervous system, which is the branch of the autonomic nervous system that is responsible for the “fight or flight” response. Acetylcholine is released from both the preganglionic and the postganglionic neurons of the parasympathetic nervous system, and acts on various target organs, such as the heart, lungs, blood vessels, digestive system, and urinary system.
Regulation of heart rate
Acetylcholine is released from the postganglionic neurons of the parasympathetic nervous system that innervate the sinoatrial node (SA node), which is the natural pacemaker of the heart. Acetylcholine binds to muscarinic receptors on the SA node, causing them to open and allow potassium ions to flow out of the cell. This hyperpolarizes the SA node, slowing down the rate of spontaneous depolarization and thus the heart rate.
Control of gastrointestinal functions
Acetylcholine is released from the postganglionic neurons of the parasympathetic nervous system that innervate the smooth muscles and the glands of the gastrointestinal tract. Acetylcholine binds to muscarinic receptors on the smooth muscles, causing them to contract and increase the motility and peristalsis of the gastrointestinal tract. Acetylcholine also binds to muscarinic receptors on the glands, stimulating the secretion of saliva, gastric acid, bile, pancreatic juice, and intestinal juice.
Acetylcholine Receptors
Acetylcholine receptors are proteins that are embedded in the membrane of the postsynaptic cell, and that bind to acetylcholine and trigger a response. There are two primary kinds of acetylcholine receptors: nicotinic receptors and muscarinic receptors. They differ in their structure, location, distribution, and physiological effects.
Nicotinic receptors
Nicotinic receptors are ionotropic receptors, which means that they are directly coupled to ion channels. When acetylcholine binds to nicotinic receptors, it causes the ion channel to open and allow sodium and potassium ions to flow across the membrane. This depolarizes the postsynaptic cell, making it more likely to fire an action potential. Nicotinic receptors are named after nicotine, a substance that can also activate them.
Location and distribution
Nicotinic receptors are found in both the CNS and the PNS, where they mediate fast and excitatory synaptic transmission. They are located on:
- The neuromuscular junction, where they are expressed on the skeletal muscle fibers and cause muscle contraction.
- The autonomic ganglia, where they are expressed on the postganglionic neurons of both the sympathetic and the parasympathetic nervous system, and modulate the activity of the target organs.
- The brain, where they are expressed on various regions and circuits, such as the basal forebrain, the midbrain, the hippocampus, the amygdala, the cortex, and the cerebellum, and regulate various cognitive functions, such as attention, learning, memory, and reward.
Physiological effects
Nicotinic receptors have various physiological effects, depending on the type and location of the postsynaptic cell. Some of the effects are:
- Muscle contraction, which is caused by the depolarization of the muscle fibers at the neuromuscular junction.
- Autonomic regulation, which is caused by the modulation of the postganglionic neurons and the target organs in the autonomic nervous system.
- Cognitive enhancement, which is caused by the stimulation of the cholinergic neurons and the release of other neurotransmitters, such as dopamine, serotonin, and norepinephrine, in the brain.
Muscarinic receptors
Muscarinic receptors are metabotropic receptors, which means that they are indirectly coupled to ion channels via G proteins and second messengers. When acetylcholine binds to muscarinic receptors, it activates a G protein, which in turn activates or inhibits an enzyme or an ion channel, leading to various cellular responses. Muscarinic receptors are named after muscarine, a substance that can also activate them.
Location and distribution
Muscarinic receptors are found mainly in the PNS, where they mediate slow and inhibitory synaptic transmission. They are located on:
- The heart, where they are expressed on the SA node and the atrioventricular node (AV node), which are responsible for the generation and conduction of the cardiac impulses.
- The smooth muscles, where they are expressed on the walls of the blood vessels, the lungs, the digestive system, the urinary system, and the reproductive system, and cause muscle relaxation or contraction.
- The glands, where they are expressed on the salivary glands, the lacrimal glands, the sweat glands, the gastric glands, the pancreatic glands, and the intestinal glands, and stimulate or inhibit the secretion of fluids.
- The brain, where they are expressed on various regions and circuits, such as the basal forebrain, the midbrain, the hippocampus, the amygdala, the cortex, and the cerebellum, and regulate various cognitive functions, such as attention, learning, memory, and reward.
Physiological effects
Muscarinic receptors have various physiological effects, depending on the type and location of the postsynaptic cell. Some of the effects are:
- Heart rate reduction, which is caused by the hyperpolarization of the SA node and the AV node at the heart.
- Smooth muscle regulation, which is caused by the opening or closing of the potassium or calcium channels on the smooth muscles of the internal organs.
- Glandular secretion, which is caused by the activation or inhibition of the enzymes or the ion channels on the glands of the body.
- Cognitive modulation, which is caused by the alteration of the neuronal excitability and the synaptic plasticity in the brain.
Role in Cognitive Function
Memory and learning processes
Acetylcholine is crucial for the formation and consolidation of memory and learning in the brain. Acetylcholine enhances the synaptic plasticity, which is the ability of the synapses to change their strength and efficiency in response to the neural activity. Acetylcholine also modulates the long-term potentiation (LTP) and the long-term depression (LTD), which are the processes that underlie the storage and retrieval of information in the brain. Acetylcholine is especially important for the declarative memory, which is the memory of facts and events, and the spatial memory, which is the memory of locations and directions.
Implications in neurodegenerative diseases
Acetylcholine is implicated in several neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease, which are characterized by the progressive loss of neurons and cognitive functions. Acetylcholine is particularly affected in Alzheimer’s disease, where the cholinergic neurons in the basal forebrain degenerate and the levels of acetylcholine in the cortex and the hippocampus decline. This leads to the impairment of memory, attention, language, and reasoning. Acetylcholine is also affected in Parkinson’s disease, where the dopaminergic neurons in the midbrain degenerate and the levels of dopamine in the striatum decline. This leads to the impairment of motor control, mood, and motivation. Acetylcholine and dopamine interact with each other in the brain, and the imbalance of these neurotransmitters contributes to the symptoms and progression of these diseases.
Regulation of Acetylcholine Levels
Acetylcholinesterase and breakdown
Acetylcholinesterase is the enzyme that breaks down acetylcholine in the synaptic cleft, terminating its action and preventing its accumulation. Acetylcholinesterase is highly expressed in the neuromuscular junction, the autonomic ganglia, and the brain, where it regulates the levels and duration of acetylcholine signaling. Acetylcholinesterase is also involved in the development and maintenance of the synaptic structure and function, as well as in the modulation of the inflammatory and immune responses.
Choline uptake and synthesis
Choline uptake is the process that transports choline from the extracellular space into the presynaptic neuron, where it is used for the synthesis of acetylcholine. Choline uptake is mediated by a transporter protein called the high-affinity choline transporter (CHT), which is expressed on the presynaptic terminal. Choline uptake is dependent on the availability of choline in the synaptic cleft, which is determined by the balance between the release and the reuptake of acetylcholine, as well as by the dietary intake of choline. Choline uptake is also regulated by various factors, such as the neuronal activity, the hormonal status, and the genetic variations.
Medical Implications
Medications affecting acetylcholine
Acetylcholine is the target of various medications that can either enhance or inhibit its action in the nervous system. These medications can have various therapeutic or adverse effects, depending on the dose, the route of administration, and the type and location of the acetylcholine receptors.
Acetylcholinesterase inhibitors
Acetylcholinesterase inhibitors are drugs that block the activity of acetylcholinesterase, increasing the levels and duration of acetylcholine in the synaptic cleft. Acetylcholinesterase inhibitors are used to treat Alzheimer’s disease and other forms of dementia, as they can improve the cognitive functions and slow down the disease progression. Acetylcholinesterase inhibitors are also used to treat myasthenia gravis, a neuromuscular disorder that causes muscle weakness and fatigue, as they can enhance the muscle contraction and strength. Acetylcholinesterase inhibitors can have side effects, such as nausea, vomiting, diarrhea, abdominal pain, headache, dizziness, and bradycardia.
Anticholinergic drugs
Anticholinergic drugs are drugs that block the action of acetylcholine, decreasing the levels and duration of acetylcholine in the synaptic cleft. Anticholinergic drugs are used to treat various conditions, such as asthma, chronic obstructive pulmonary disease (COPD), overactive bladder, irritable bowel syndrome (IBS), motion sickness, and Parkinson’s disease, as they can relax the smooth muscles, reduce the glandular secretion, and suppress the tremor and rigidity. Anticholinergic drugs can have side effects, such as dry mouth, blurred vision, constipation, urinary retention, confusion, memory loss, and delirium.
Research and Future Directions
Ongoing studies
Acetylcholine is the subject of ongoing studies that aim to elucidate its role and mechanism in the nervous system and beyond. A portion of the flow research points are:
- The molecular and cellular basis of acetylcholine synthesis, release, reuptake, breakdown, and receptor activation and desensitization.
- The neural circuits and networks that involve acetylcholine and its interactions with other neurotransmitters and neuromodulators.
- The behavioral and cognitive functions that depend on acetylcholine and its modulation by various factors, such as stress, emotion, attention, arousal, sleep, and aging.
- The pathophysiology and pharmacology of acetylcholine in various neurological and psychiatric disorders, such as schizophrenia, depression, anxiety, epilepsy, and addiction.
- The role of acetylcholine in the peripheral tissues and organs, such as the immune system, the cardiovascular system, the metabolic system, and the reproductive system.
Potential therapeutic applications
Acetylcholine is the target of potential therapeutic applications that aim to improve the health and quality of life of the patients. Some of the future directions are:
- The development of novel and selective acetylcholine receptor agonists and antagonists, as well as acetylcholinesterase inhibitors and enhancers, that can modulate the acetylcholine signaling in a specific and effective way.
- The use of gene therapy, stem cell therapy, and optogenetics to restore or enhance the function of the cholinergic neurons and the acetylcholine receptors in the brain and the body.
- The use of non-invasive brain stimulation, such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), to modulate the activity of the cholinergic neurons and the acetylcholine receptors in the brain.
- The use of cognitive training, physical exercise, and dietary supplementation to boost the acetylcholine levels and the cognitive functions in the healthy and the diseased population.
Conclusion
Recapitulation of key points
Acetylcholine is a key molecule in neuroscience and medicine, as it plays a vital role in the functioning of the nervous system and the body. Acetylcholine is involved in various processes, such as transmitting nerve impulses, regulating heart rate, controlling gastrointestinal functions, and facilitating memory and learning. Acetylcholine also has implications in several neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease, and can be affected by various medications. Acetylcholine is regulated by various mechanisms, such as acetylcholinesterase and breakdown, choline uptake and synthesis, and receptor activation and desensitization. Acetylcholine is the subject of ongoing studies and potential therapeutic applications that aim to elucidate its role and mechanism, and to improve its function and modulation.
Importance of understanding acetylcholine in neuroscience and medicine
Understanding acetylcholine in neuroscience and medicine is important for several reasons, such as:
- To gain a deeper insight into the structure and function of the nervous system and the body, and how they interact and coordinate with each other.
- To discover the causes and consequences of the alterations and dysfunctions of acetylcholine in various neurological and psychiatric disorders, and how they affect the patients and the society.
- To develop new and better diagnostic tools, preventive strategies, and therapeutic interventions for the patients who suffer from acetylcholine-related diseases, and to improve their health and quality of life.
- To explore the possibilities and limitations of enhancing and optimizing the acetylcholine signaling and the cognitive functions in the healthy and the diseased population, and to evaluate the ethical and social implications of doing so.
FAQ
- What is acetylcholine?
- Acetylcholine is a chemical messenger that carries signals between neurons and other cells in the nervous system and the body.
- What are the functions of acetylcholine?
- Acetylcholine is involved in various functions, such as transmitting nerve impulses, regulating heart rate, controlling gastrointestinal functions, and facilitating memory and learning.
- What are the types of acetylcholine receptors?
- There are two principal sorts of acetylcholine receptors: nicotinic receptors and muscarinic receptors. They differ in their structure, location, distribution, and physiological effects.
- What are the diseases related to acetylcholine?
- Acetylcholine is implicated in several neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease, which are characterized by the progressive loss of neurons and cognitive functions.
- What are the medications affecting acetylcholine?
- Acetylcholine is the target of various medications that can either enhance or inhibit its action in the nervous system. These medications can have various therapeutic or adverse effects, depending on the dose, the route of administration, and the type and location of the acetylcholine receptors.
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.