Introduction
Diabetes is one of the most prevalent chronic health conditions globally, affecting millions of individuals and posing severe health risks when left untreated. Proper management is vital for reducing the complications associated with diabetes, such as cardiovascular disease, neuropathy, and more. Medications play a key role in blood sugar regulation, alongside lifestyle changes like diet and exercise. Among the options available, Ozempic and Metformin stand out as two effective medications for diabetes management. Choosing the right treatment can significantly impact health outcomes, making it essential to understand how each medication works and their specific benefits.
Overview of Diabetes and Its Management
Diabetes is characterized by elevated blood sugar levels due to the body's inability to produce or effectively use insulin. This metabolic disorder primarily encompasses type 1 and type 2 diabetes, with type 2 being the most common. Effective management focuses on maintaining healthy blood glucose levels through a combination of medications, diet modifications, physical activity, and regular monitoring. Different medications work through various mechanisms to regulate blood sugar, improve insulin sensitivity, and even reduce weight. Medications like Ozempic and Metformin, both commonly prescribed for type 2 diabetes, offer unique pathways to managing the disease, helping patients achieve optimal outcomes.
Purpose of the Comparison: Ozempic vs. Metformin
With numerous medications available, choosing the most suitable treatment for diabetes can be complex. Ozempic and Metformin are frequently prescribed and widely discussed due to their proven benefits. While Metformin has been a staple in diabetes care for decades, Ozempic offers a newer, innovative approach. The purpose of this comparison is to highlight the strengths and weaknesses of each medication, enabling patients and healthcare professionals to make more informed decisions. The right choice can make a significant difference in controlling blood sugar levels, improving overall health, and enhancing the quality of life for individuals living with diabetes. Ozempic and Metformin
Brief Introduction to Ozempic and Metformin
Ozempic, also known as semaglutide, is a glucagon-like peptide-1 (GLP-1) receptor agonist that works by stimulating insulin secretion and reducing appetite. It is primarily used for type 2 diabetes but also shows promise in weight management. On the other hand, Metformin, a biguanide, reduces glucose production in the liver and improves insulin sensitivity in the muscles, making it a long-standing first-line treatment for type 2 diabetes. These medications differ in their mechanisms, administration methods, and additional benefits, making them particularly important to compare when evaluating treatment options. Ozempic and Metformin
Importance of Choosing the Right Medication
The correct medication can improve blood sugar control, reduce complications, and potentially promote weight loss, all while minimizing side effects. Diabetes management is highly individualized, with factors like age, weight, other medical conditions, and specific health goals all influencing the choice of treatment. Comparing Ozempic and Metformin helps patients and healthcare providers better understand their respective benefits, risks, and limitations. An informed decision not only improves diabetes management but can also enhance a patient’s overall well-being and adherence to treatment. Ozempic and Metformin
Understanding Ozempic and Metformin: Background and Development
History of Ozempic
Ozempic was developed as part of a new class of GLP-1 receptor agonists. Approved by the FDA in 2017, it is administered via a weekly injection. This medication mimics the function of naturally occurring GLP-1 hormones, which regulate insulin and reduce appetite. Ozempic's development focused on enhancing blood sugar control while offering weight management benefits, making it a popular option in modern diabetes treatment protocols. Ozempic and Metformin
- Development and Approval Timeline
- The journey of Ozempic's approval involved years of clinical trials to ensure its efficacy and safety. Studies demonstrated its ability to significantly lower blood sugar levels, reduce HbA1c levels, and promote weight loss compared to other diabetes medications. The approval and subsequent incorporation into treatment guidelines highlight its role as an innovative solution for type 2 diabetes. Ozempic and Metformin
- Position in Diabetes Treatment Protocols
- Ozempic is considered a second-line or add-on therapy for patients who do not achieve adequate control with initial treatments like Metformin. It is especially recommended for those needing additional weight loss support or cardiovascular protection, showing its utility beyond glycemic control.
History of Metformin
Metformin, on the other hand, has a much longer history, tracing its roots back to the 1920s. Derived from a compound found in the French lilac plant, Metformin gained recognition for its ability to lower blood sugar without causing hypoglycemia. It was first introduced for diabetes management in the 1950s and remains a cornerstone of treatment for type 2 diabetes.
- Origins and Long-Standing Use
- Metformin has been prescribed worldwide for decades, earning a reputation as a safe, effective, and affordable first-line therapy. It is often used as the initial medication for newly diagnosed type 2 diabetes patients due to its proven benefits and minimal side effects. Ozempic and Metformin
- Effectiveness and Widespread Adoption
- The widespread adoption of Metformin can be attributed to its ability to improve insulin sensitivity and reduce glucose production, making it a highly effective option for managing type 2 diabetes. Its affordability, well-documented safety profile, and compatibility with other medications further solidify its position as a foundational treatment.
Major Differences Between Ozempic and Metformin

Understanding the distinctions between Ozempic and Metformin is essential for patients and healthcare providers managing type 2 diabetes. Ozempic (semaglutide) and Metformin are both medications designed to help control blood sugar, but they differ significantly in terms of drug classification, mechanisms of action, and overall applications. By examining their unique roles, individuals can better grasp how each drug fits into diabetes treatment plans. Ozempic and Metformin
Drug Classification
- GLP-1 Receptor Agonist (Ozempic)
Ozempic is classified as a GLP-1 (glucagon-like peptide-1) receptor agonist. These medications mimic the effects of the GLP-1 hormone, which is involved in insulin secretion, appetite regulation, and slowing gastric emptying. This multi-faceted approach results in improved blood sugar control and often helps patients achieve weight loss. GLP-1 receptor agonists like Ozempic are injectable medications, typically administered once weekly. Ozempic and Metformin
- Biguanide (Metformin)
Metformin, on the other hand, is a biguanide—a well-established and widely used oral medication for managing type 2 diabetes. Metformin works primarily by reducing glucose production in the liver and enhancing insulin sensitivity in muscle and fat tissues. It is often considered a first-line therapy due to its long-term safety profile, effectiveness, and affordability.
Mechanism of Action
- How Each Medication Affects Blood Sugar Regulation
Ozempic’s mechanism of action is centered on its role as a GLP-1 receptor agonist. By mimicking this hormone, it stimulates the pancreas to release insulin in response to meals, suppresses the release of glucagon (a hormone that raises blood sugar levels), and slows down stomach emptying, reducing post-meal spikes in glucose levels. This comprehensive effect often leads to weight reduction, which is particularly beneficial for type 2 diabetes patients who are overweight or obese.
- Metformin primarily works by inhibiting hepatic gluconeogenesis (the production of glucose in the liver). By decreasing the amount of glucose produced and improving peripheral glucose uptake, Metformin helps lower blood sugar without causing weight gain or a significant risk of hypoglycemia. Unlike Ozempic, it does not rely on insulin secretion to achieve its blood-sugar-lowering effects. Ozempic and Metformin
Eligibility for Use
- Who Benefits Most from Each Medication Type
Ozempic is generally recommended for adults with type 2 diabetes who have not achieved adequate blood sugar control with other medications, including Metformin. Its ability to promote weight loss makes it suitable for overweight or obese patients. Additionally, it can be used as a second-line treatment when Metformin alone does not suffice. It is less commonly prescribed for patients with a history of severe gastrointestinal disease.
- Metformin, meanwhile, is often the first medication prescribed to newly diagnosed type 2 diabetes patients. Its affordability, oral administration, and minimal side effects make it suitable for many individuals. Those with mild to moderate diabetes often see significant improvement with Metformin alone, although it may be contraindicated in patients with advanced kidney disease due to the risk of lactic acidosis. Ozempic and Metformin
Uses of Ozempic vs. Metformin
Primary Indications for Each Drug
The primary indication for Ozempic is to improve blood sugar levels in adults with type 2 diabetes, particularly when combined with diet and exercise. It is also approved for reducing cardiovascular risk in patients with diabetes and heart disease. Metformin is indicated as a first-line therapy to improve blood sugar control in patients with type 2 diabetes and can be used alone or with other medications. Ozempic and Metformin
- FDA-Approved Uses for Diabetes Management
Ozempic is specifically approved to manage blood sugar in type 2 diabetes patients, with evidence supporting its cardiovascular benefits. Metformin is approved to treat type 2 diabetes and is often used as a first-line therapy due to its efficacy, safety profile, and lower cost. It is also used in combination therapy when necessary.
- Off-Label Uses and Considerations
Ozempic has limited off-label uses, primarily focused on weight management. Metformin, however, is used off-label for conditions such as polycystic ovary syndrome (PCOS) due to its effects on insulin sensitivity and metabolic health. Research is ongoing regarding Metformin’s potential anti-aging and anti-cancer properties.
Effectiveness in Type 2 Diabetes Control
- Short- and Long-Term Impact on Blood Sugar Levels
Ozempic has demonstrated significant efficacy in reducing HbA1c levels, with many patients experiencing better glycemic control compared to those taking oral medications alone. It often results in meaningful weight loss, which can further improve metabolic health and reduce the long-term risk of complications.
- Metformin also effectively lowers blood glucose and HbA1c levels, particularly in the initial stages of treatment. While it does not lead to weight loss like Ozempic, its proven track record, affordability, and minimal side effects make it a cornerstone of type 2 diabetes management. Combining Metformin with other drugs, including Ozempic, often results in optimal long-term glycemic control. Ozempic and Metformin
How Ozempic and Metformin Work
A clear understanding of how Ozempic and Metformin function in controlling blood sugar levels can provide patients and healthcare providers with key insights into the best treatment options for managing type 2 diabetes. Both medications play critical roles in reducing blood glucose levels, but they differ in their mechanisms of action and how they are administered.
Ozempic: Mechanism of Action
- Role of GLP-1 in Blood Sugar Control
Ozempic (semaglutide) functions as a GLP-1 (glucagon-like peptide-1) receptor agonist. GLP-1 is an incretin hormone released by the intestines in response to food intake. It plays a vital role in blood sugar control by enhancing insulin secretion from the pancreas, inhibiting the release of glucagon (which raises blood sugar), and slowing gastric emptying to prevent sharp rises in blood glucose following meals. Ozempic and Metformin
- How Ozempic Modulates Glucose Levels
When administered, Ozempic binds to GLP-1 receptors and mimics the natural actions of this hormone, resulting in improved insulin release and reduced glucose output by the liver. By lowering blood sugar and promoting weight loss through appetite suppression, Ozempic addresses multiple metabolic dysfunctions seen in type 2 diabetes patients. Its long half-life allows for once-weekly dosing, improving patient adherence and providing consistent glycemic control.
Metformin: Mechanism of Action
- Reduction of Hepatic Glucose Production
Metformin works primarily by inhibiting hepatic gluconeogenesis, the process by which the liver produces glucose. By limiting excess glucose release into the bloodstream, Metformin helps to reduce fasting blood sugar levels. This action is critical in maintaining lower overall blood glucose levels in individuals with type 2 diabetes, where the liver's overproduction of glucose is a common problem. Ozempic and Metformin
- Effects on Insulin Sensitivity
In addition to its effects on the liver, Metformin enhances insulin sensitivity, particularly in muscle and fat tissues. This means that the body is able to utilize insulin more effectively, leading to better glucose uptake and reduced insulin resistance. Unlike Ozempic, Metformin does not rely on stimulating insulin secretion and does not typically cause weight gain. Its favorable impact on weight neutrality or slight weight loss further contributes to its utility in diabetes management.
Dosages, Forms, and Administration of Ozempic vs. Metformin
Proper administration and adherence to prescribed dosages of Ozempic and Metformin are essential for optimizing their therapeutic benefits. Their dosages and forms vary to meet different patient needs and treatment goals.
Ozempic Dosage and Administration
Ozempic is available in different strengths, with the common dosages being 0.25 mg, 0.5 mg, 1 mg, and 2 mg delivered via pre-filled pens. Typically, the initial dose starts at 0.25 mg once weekly to minimize gastrointestinal side effects, then gradually increases based on the patient's tolerance and treatment goals. Ozempic injections are administered subcutaneously in the abdomen, thigh, or upper arm. Ozempic and Metformin
Excel Table (Ozempic Dosage Example)
| Dosage |
Frequency |
Administration Method |
| 0.25 mg |
Once Weekly |
Subcutaneous Injection |
| 0.5 mg |
Once Weekly |
Subcutaneous Injection |
| 1 mg |
Once Weekly |
Subcutaneous Injection |
| 2 mg |
Once Weekly |
Subcutaneous Injection |
Metformin Dosage and Administration
Metformin comes in both immediate-release (IR) and extended-release (ER) tablets. Immediate-release tablets are usually started at a low dose (e.g., 500 mg once or twice daily) to reduce gastrointestinal side effects. Dosage can be titrated up to 2,000-2,500 mg per day based on patient needs. Extended-release forms provide more convenient once-daily dosing, often improving tolerance.
Excel Table (Metformin Dosage Example)
| Form |
Typical Starting Dose |
Maximum Dose |
Frequency |
| Immediate-Release |
500 mg once or twice daily |
2,500 mg/day |
2-3 times daily |
| Extended-Release |
500 mg once daily |
2,000 mg/day |
Once daily |
The different forms and dosing flexibility of Metformin make it suitable for gradual titration to achieve optimal blood sugar control. While Ozempic’s once-weekly injection schedule is ideal for convenience and sustained effects, Metformin’s oral dosing and affordability remain attractive features for diabetes management.
Side Effects of Ozempic vs. Metformin
Ozempic and Metformin are effective treatments for type 2 diabetes, but each has its unique profile of potential side effects. Understanding these is crucial for patients and healthcare providers to ensure optimal management and safety. While both medications can cause mild and serious side effects, their specific impacts and management strategies differ.
Mild Side Effects of Each Medication
| Ozempic |
Metformin |
| Nausea |
Nausea |
| Vomiting |
Diarrhea |
| Diarrhea |
Stomach upset |
| Constipation |
Bloating |
| Fatigue |
Loss of appetite |
| Mild stomach pain |
Mild weight loss |
| Loss of appetite |
Metallic taste |
Common, Non-Serious Side Effects for Each Drug
Ozempic frequently causes gastrointestinal side effects like nausea, vomiting, and diarrhea, especially when starting the medication or increasing the dose. Most patients see these symptoms decrease over time as their bodies adjust. Metformin’s mild side effects are also primarily gastrointestinal, including nausea, diarrhea, and bloating, often alleviated by taking the medication with food or switching to an extended-release formulation. Ozempic and Metformin
Management of Mild Side Effects
To manage Ozempic’s side effects, healthcare providers may suggest initiating therapy with a lower dose and gradually increasing it. Taking Ozempic with food may also minimize discomfort. For Metformin, starting at a low dose and titrating up helps mitigate side effects. Patients can also take the medication with meals to reduce stomach irritation.
Serious Side Effects of Each Medication
| Ozempic |
Metformin |
| Pancreatitis |
Lactic acidosis |
| Thyroid tumors (possible risk) |
Severe gastrointestinal distress |
| Hypoglycemia (when combined) |
Vitamin B12 deficiency |
| Severe allergic reactions |
Liver dysfunction (rare) |
Severe or Rare Adverse Effects
Ozempic has been linked to more severe issues like pancreatitis and a possible increased risk of thyroid tumors, as observed in animal studies. While thyroid cancer risk has not been conclusively shown in humans, it requires caution. Ozempic may also lead to hypoglycemia when used with other medications, such as insulin. Metformin, while generally safer, has a rare but serious risk of lactic acidosis, particularly in patients with kidney impairment. Vitamin B12 deficiency can occur with prolonged use, warranting regular monitoring.
Risk Factors and Monitoring Requirements
Patients using Ozempic should be monitored for symptoms of pancreatitis, such as severe abdominal pain, and be advised of potential thyroid concerns. Monitoring thyroid function may be suggested for at-risk patients. For Metformin, regular kidney function tests are recommended to reduce the risk of lactic acidosis. Patients with severe renal impairment are usually advised against using Metformin.
Ozempic vs. Metformin for Weight Loss
Ozempic and Weight Loss Potential
Ozempic has gained attention not just for its glycemic control but also for its weight-loss benefits. Clinical studies demonstrate significant weight loss among patients using Ozempic due to its appetite suppression, delayed gastric emptying, and improved insulin regulation. These effects make it especially appealing for individuals with type 2 diabetes who also struggle with obesity. Patients typically report a reduced desire to eat and better control over portions, contributing to overall calorie reduction.
- Clinical Studies on Weight Reduction
Multiple clinical trials have confirmed Ozempic’s weight-loss potential, showing reductions of up to 15% of body weight in some patients. This is achieved through its multi-pronged hormonal actions that extend beyond simply controlling blood glucose.
- Mechanisms Contributing to Weight Loss with Ozempic
Ozempic activates GLP-1 receptors, resulting in appetite suppression and delayed gastric emptying. This leads to reduced food intake and a longer feeling of fullness, which contribute to weight loss.
Metformin’s Role in Weight Management
While Metformin is not primarily used for weight loss, some patients experience modest weight reduction, likely due to improved insulin sensitivity and reduced appetite. This effect is less pronounced than that seen with Ozempic but can be beneficial for patients aiming for modest weight management alongside blood sugar control. Ozempic and Metformin
- Observed Weight-Related Effects
The weight-related impact of Metformin is often subtle. Some patients may experience mild weight loss or weight stabilization, which can positively impact blood sugar control. However, it is not considered a primary weight-loss medication.
- Suitability of Metformin for Patients Seeking Weight Loss
For individuals primarily aiming for significant weight loss, Metformin is not typically sufficient. Ozempic, with its demonstrated weight-loss benefits, may be a more suitable option, especially for patients with type 2 diabetes and obesity. However, healthcare providers assess each patient’s unique needs, preferences, and health conditions when prescribing a treatment plan. Ozempic and Metformin
Efficacy of Ozempic and Metformin in Glycemic Control
A comprehensive look at the efficacy of Ozempic (semaglutide) and Metformin in controlling blood sugar is crucial for understanding their role in type 2 diabetes management. These drugs target different pathways and have distinct clinical outcomes that make them suitable for diverse patient populations.
Ozempic Efficacy Studies
- Clinical Data on Blood Sugar Reduction
Clinical studies on Ozempic consistently demonstrate its powerful glucose-lowering capabilities. As a GLP-1 receptor agonist, Ozempic reduces blood sugar levels by stimulating insulin secretion in response to meals, suppressing glucagon release, and slowing gastric emptying. Trials like the SUSTAIN series have shown that patients taking Ozempic achieve significant reductions in fasting and postprandial blood glucose levels compared to placebo and even some other anti-diabetic agents. Many patients experience meaningful weight loss, which further enhances glycemic control and reduces cardiovascular risk factors.
- Benefits in HbA1c Levels and Daily Glucose Management
Ozempic effectively lowers HbA1c levels by as much as 1.5% to 2% in patients with type 2 diabetes. The reduction is often achieved within a few months of starting therapy and is maintained over the long term. Daily glucose fluctuations are also minimized, improving patients' overall glycemic control and quality of life. This makes Ozempic a valuable option, particularly for those who struggle to control blood sugar levels with oral medications alone. Ozempic and Metformin
Metformin Efficacy Studies
- Evidence on Blood Glucose Control
Metformin is a cornerstone in diabetes management due to its proven ability to lower blood glucose levels. Studies have repeatedly confirmed that it decreases hepatic glucose production and increases insulin sensitivity, leading to lower fasting blood sugar. As a first-line therapy, Metformin’s effectiveness is well-supported, especially in newly diagnosed patients. When combined with lifestyle modifications, it can lead to marked improvements in glycemic control, sometimes sufficient to delay the progression of diabetes.
- Long-Term Effects on HbA1c and Overall Diabetes Management
Metformin reduces HbA1c levels by approximately 1% to 1.5%, making it a robust option for initial diabetes therapy. While its effect may plateau over time, it remains a mainstay due to its cost-effectiveness, safety, and role in combination therapies. Its impact on reducing diabetes-related complications, including cardiovascular issues, further underscores its utility in long-term diabetes management. Ozempic and Metformin
Cost Comparison: Ozempic vs. Metformin
Pricing Overview and Insurance Coverage
Cost implications are important in deciding on treatments. Ozempic is a newer medication and generally more expensive than Metformin, reflecting its injectable form and novel mechanism of action. Without insurance, the monthly cost of Ozempic can exceed several hundred dollars. However, insurance coverage and manufacturer savings programs may reduce costs for eligible patients. Metformin, as a generic drug, is widely accessible and often costs less than $10 per month.
- Typical Out-of-Pocket Costs
Patients without insurance may find Ozempic challenging to afford due to high out-of-pocket costs. In contrast, Metformin is highly affordable for nearly all patients, whether through insurance plans or out-of-pocket purchases. This cost discrepancy influences patient adherence and may determine the suitability of each drug for individual cases.
- Insurance Support for Each Medication
Ozempic often requires prior authorization or evidence of failure with less expensive therapies, which can limit its accessibility. Metformin is almost universally covered without restrictions, making it an easy and accessible first-line choice for type 2 diabetes patients.
Cost-Effectiveness and Accessibility
The overall cost-effectiveness of Metformin makes it a staple in diabetes management. Ozempic’s higher price point can be justified by its superior glycemic control and weight loss benefits, but only when patients have the financial resources and insurance support to access it. This cost factor may impact patient compliance, with cheaper options like Metformin generally leading to better adherence.
Safety Profile and Monitoring for Ozempic vs. Metformin
Monitoring Requirements for Each Drug
Both Ozempic and Metformin require patient monitoring to ensure safety. Ozempic users may need regular assessments of kidney function, thyroid levels, and any potential gastrointestinal symptoms. Metformin requires monitoring for renal function due to its risk of lactic acidosis, especially in patients with chronic kidney disease. Periodic HbA1c checks are recommended for both drugs to evaluate treatment efficacy. Ozempic and Metformin
Frequency and Types of Tests Required
For Ozempic, thyroid ultrasounds and monitoring for symptoms of thyroid tumors are necessary due to a potential increased risk in animal studies. Metformin’s monitoring is simpler, primarily focusing on kidney function tests, particularly for patients with comorbid conditions.
Signs and Symptoms to Monitor for Side Effects
Ozempic’s side effects can include nausea, vomiting, and potential pancreatitis symptoms, which patients must be educated about. Metformin’s side effects are generally milder, including gastrointestinal discomfort such as bloating and diarrhea, but patients should watch for signs of lactic acidosis.
Safety in Long-Term Use
Long-term studies show that Ozempic is effective for sustained weight and blood sugar control but may require ongoing monitoring for thyroid cancer risks. Metformin’s long-term use is well-documented, with potential benefits extending beyond diabetes control, including cardiovascular protection and cancer prevention. For patients with comorbidities, both drugs require careful balancing of risks and benefits, often with a personalized treatment approach based on individual health profiles. Ozempic and Metformin
Contraindications for Ozempic and Metformin
When considering the use of Ozempic (semaglutide) and Metformin for managing type 2 diabetes, it’s important to understand the specific health conditions and patient factors that may limit or exclude their use. Both medications, though highly effective in blood sugar regulation, come with certain contraindications and potential risks when not used appropriately. Understanding who should avoid each medication helps ensure the best therapeutic outcomes and patient safety.
Who Should Avoid Ozempic?
Specific Health Conditions and Contraindications
Ozempic, a GLP-1 receptor agonist, is generally not recommended for patients with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2). These conditions are associated with an increased risk of thyroid cancer, and studies in animals have shown a potential link between GLP-1 receptor agonists and thyroid tumors, though this has not been conclusively proven in humans. As a result, patients with these risk factors should avoid Ozempic.
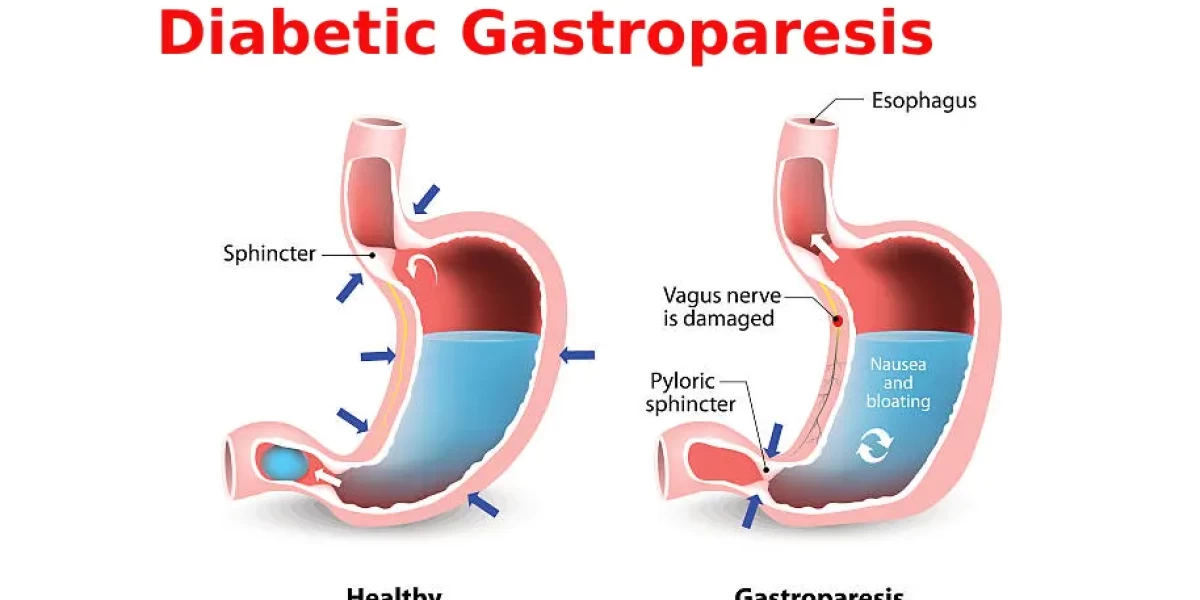
Additionally, Ozempic should not be used in patients with a history of severe gastrointestinal disorders such as gastroparesis, which causes delayed stomach emptying, as the medication's action of slowing gastric emptying can exacerbate these conditions. Ozempic is also contraindicated in individuals with diabetic ketoacidosis (DKA) and should be used with caution in patients with severe renal impairment. Pregnant or breastfeeding women should consult their healthcare provider before considering Ozempic, as its safety during pregnancy has not been established. Ozempic and Metformin
Who Should Avoid Metformin?
Conditions Under Which Metformin May Not Be Recommended
Metformin, a standard treatment for type 2 diabetes, is usually well tolerated. However, certain conditions may make it unsafe or inappropriate for use. Metformin is contraindicated in patients with severe kidney disease, particularly those with an estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m², as impaired kidney function increases the risk of lactic acidosis, a potentially fatal condition. It should also be used with caution in patients with moderate renal impairment, with dose adjustments typically required.
Patients with acute or chronic metabolic acidosis, including diabetic ketoacidosis, should not take Metformin due to the increased risk of lactic acidosis. Furthermore, individuals with a history of liver disease or heavy alcohol use may be at higher risk for complications with Metformin, as the drug can affect liver function and its clearance from the body. Metformin is also contraindicated during pregnancy due to concerns about its safety for the fetus, although it is sometimes used off-label in gestational diabetes under careful medical supervision.
Interactions of Ozempic and Metformin with Other Medications
Ozempic Drug Interactions
Ozempic interacts with several medications, and awareness of these interactions is crucial for patient safety. One notable interaction is with insulins and other glucose-lowering drugs, as using Ozempic in combination with insulin or sulfonylureas may increase the risk of hypoglycemia (low blood sugar). In such cases, dosage adjustments may be needed to avoid this side effect. Ozempic and Metformin
Ozempic can also interact with medications that affect gastrointestinal motility, such as opioid pain relievers, which could exacerbate its side effects of nausea and delayed gastric emptying. Additionally, medications that slow down the clearance of drugs via the kidneys, such as certain diuretics or ACE inhibitors, may require closer monitoring in patients using Ozempic. It's important to note that patients should inform their healthcare provider of all medications they are taking to assess potential interactions and adjust their treatment regimen accordingly. Ozempic and Metformin
Metformin Drug Interactions
Metformin also has a range of drug interactions that could affect its efficacy or lead to adverse effects. One of the most critical interactions is with medications that can impair kidney function, such as nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics, and contrast agents used in imaging tests. These drugs can increase the risk of lactic acidosis, so dose adjustments or temporary discontinuation of Metformin may be necessary when such drugs are prescribed.
Metformin can also interact with drugs that lower blood sugar, such as insulin or sulfonylureas, which may increase the risk of hypoglycemia. In these cases, careful monitoring of blood sugar levels is recommended. Additionally, certain antihypertensive medications, particularly ACE inhibitors and angiotensin II receptor blockers (ARBs), may alter Metformin’s effect, so patients should be closely monitored for signs of low blood pressure or kidney dysfunction.
Patient Experience and Satisfaction: Ozempic vs. Metformin
Patient Adherence and Convenience
Adherence to diabetes medication regimens can be challenging for many patients, and factors like dosage forms, frequency, and ease of use play a key role in long-term success. Ozempic is an injectable medication, administered once weekly. While the weekly injection may be convenient for some patients, others may find the injection process off-putting. However, it is generally well-tolerated, and the long-acting nature of Ozempic reduces the burden of daily dosing. For patients seeking an injectable therapy with fewer administration requirements, Ozempic offers a convenient option. Ozempic and Metformin
In contrast, Metformin is an oral medication, which tends to be preferred by many patients due to its ease of use. However, it is typically taken multiple times a day with meals to reduce gastrointestinal side effects like nausea or upset stomach. While Metformin is often the first choice due to its affordability and availability, its dosing schedule may be less convenient for those with busy lifestyles. Additionally, some patients experience side effects that can hinder adherence, though these are often manageable with adjustments to the dosage or administration.
Patient Reported Outcomes
Patient satisfaction with Ozempic and Metformin varies depending on individual needs and experiences. Many patients report positive outcomes with Ozempic, particularly due to its weight loss effects and its ability to reduce blood sugar levels effectively. However, some patients may experience gastrointestinal issues like nausea, particularly when starting the medication, though these typically subside with continued use. Patients who value the weight loss and long-term glucose control provided by Ozempic tend to have a favorable experience.
Metformin is also widely respected for its effectiveness in lowering blood glucose levels and has a strong track record for safety. However, gastrointestinal side effects, including diarrhea and bloating, are common complaints among Metformin users. Despite these side effects, many patients find Metformin manageable, especially once they adjust to the medication or switch to an extended-release formulation that may reduce these symptoms. Overall, patient satisfaction is high with Metformin due to its affordability, long-term track record, and efficacy in controlling blood sugar.
Environmental and Societal Impact of Ozempic vs. Metformin
When considering medications for managing type 2 diabetes, understanding their broader environmental and societal implications is important. Both Ozempic and Metformin are widely used, but they differ in their manufacturing processes, environmental footprint, and effects on healthcare systems. These differences can influence the long-term sustainability of diabetes care and access to treatment. Ozempic and Metformin
Manufacturing and Environmental Considerations
Sustainability of Production Methods
Ozempic and Metformin have different environmental impacts due to their distinct manufacturing processes. Ozempic, as a GLP-1 receptor agonist, requires complex biologic production methods. The synthesis of semaglutide, the active ingredient in Ozempic, involves biotechnological processes that often rely on specialized facilities. Biologic drug manufacturing can be resource-intensive, with higher energy consumption, waste production, and potential for environmental degradation in the supply chain. Additionally, as an injectable, Ozempic requires packaging in single-use vials or pens, which adds to the plastic waste burden.
Metformin, by contrast, is a small-molecule drug with simpler chemical synthesis. Its production process generally has a lower environmental impact in terms of energy use and waste generation. Since Metformin is an oral medication, it also avoids the need for injection devices and single-use plastic packaging. While Metformin’s manufacturing footprint is lower, it still requires resources such as raw materials and energy, though its overall environmental impact is typically considered less significant than that of Ozempic.
Impact on Healthcare Systems
Accessibility and Healthcare Resource Allocation
Ozempic and Metformin differ in terms of accessibility and how they affect healthcare systems. Metformin is widely available, affordable, and often included on essential medication lists in many countries. It is the first-line treatment for type 2 diabetes and is often prescribed as the go-to solution for managing blood sugar levels. Its affordability, in particular, makes it accessible to a larger population, including those in lower-income regions, thereby easing the burden on healthcare systems. Ozempic and Metformin
Ozempic, on the other hand, is a more expensive treatment due to its status as a biologic drug, which drives up healthcare costs. While it is highly effective, especially in patients with type 2 diabetes who are overweight or obese, its cost may limit its accessibility in certain parts of the world. In wealthier countries, insurance coverage may offset some of the expense, but in regions with less robust healthcare systems, the cost of Ozempic can present a barrier to access. As a result, healthcare resource allocation may be impacted, requiring prioritization of more affordable drugs like Metformin, especially in public health settings.
Summary
In summary, Ozempic and Metformin differ significantly in terms of their classification, mechanisms of action, and impact on diabetes care. Ozempic, a GLP-1 receptor agonist, is typically prescribed for patients who need additional support with blood sugar control, particularly those who are overweight or have cardiovascular disease. It is effective at lowering blood sugar and promoting weight loss but comes at a higher cost. Metformin, a biguanide, is the first-line therapy for type 2 diabetes, providing effective blood sugar control at a lower cost and with fewer side effects. While Ozempic may offer additional benefits, its accessibility is limited by its price.
Both medications contribute to managing type 2 diabetes, but their environmental impacts also reflect their respective production processes, with Metformin being less resource-intensive than Ozempic. Ozempic and Metformin
When choosing between Ozempic and Metformin, the decision should be based on the patient’s specific health needs, financial situation, and the guidance of a healthcare professional. Metformin remains the go-to treatment for most individuals with type 2 diabetes, offering broad accessibility and affordability. However, for patients who struggle with obesity or need more aggressive blood sugar control, Ozempic may be a beneficial option, particularly when combined with lifestyle changes. Ultimately, both medications have important roles in diabetes management, and a tailored approach is key to achieving optimal health outcomes.
Frequently Asked Questions (FAQs)
What are the key differences between Ozempic and Metformin?
The main differences lie in their drug classifications and mechanisms of action. Ozempic is a GLP-1 receptor agonist that helps lower blood sugar and promotes weight loss, while Metformin is a biguanide that reduces glucose production in the liver and improves insulin sensitivity.
Can Ozempic and Metformin be taken together?
Yes, Ozempic and Metformin can be prescribed together, as they work in different ways to manage blood sugar. Combining them can offer complementary benefits, especially for patients who need additional blood sugar control.
Which drug is better for weight loss?
Ozempic is generally considered more effective for weight loss due to its appetite-suppressing effects and ability to slow gastric emptying. While Metformin may contribute to modest weight loss, its primary focus is on blood sugar regulation rather than weight management.
What are the risks of long-term use for each medication?
Long-term use of Ozempic may lead to gastrointestinal issues like nausea, vomiting, or diarrhea. There is also a risk of pancreatitis and potential kidney issues with prolonged use. For Metformin, the most significant long-term risk is lactic acidosis, particularly in patients with kidney or liver issues. Regular monitoring is important to minimize these risks.
How do I choose between Ozempic and Metformin with my doctor’s guidance?
Your doctor will consider factors such as your blood sugar levels, weight, overall health, and medical history when recommending between Ozempic and Metformin. If Metformin alone is not enough to control your diabetes, Ozempic may be added.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.