Introduction
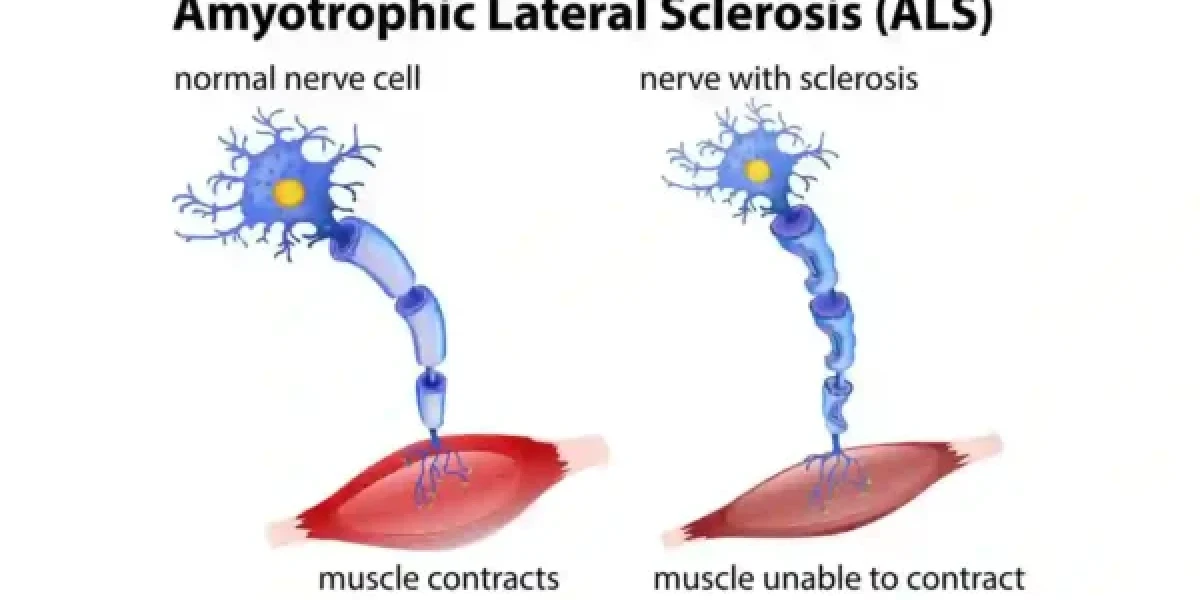
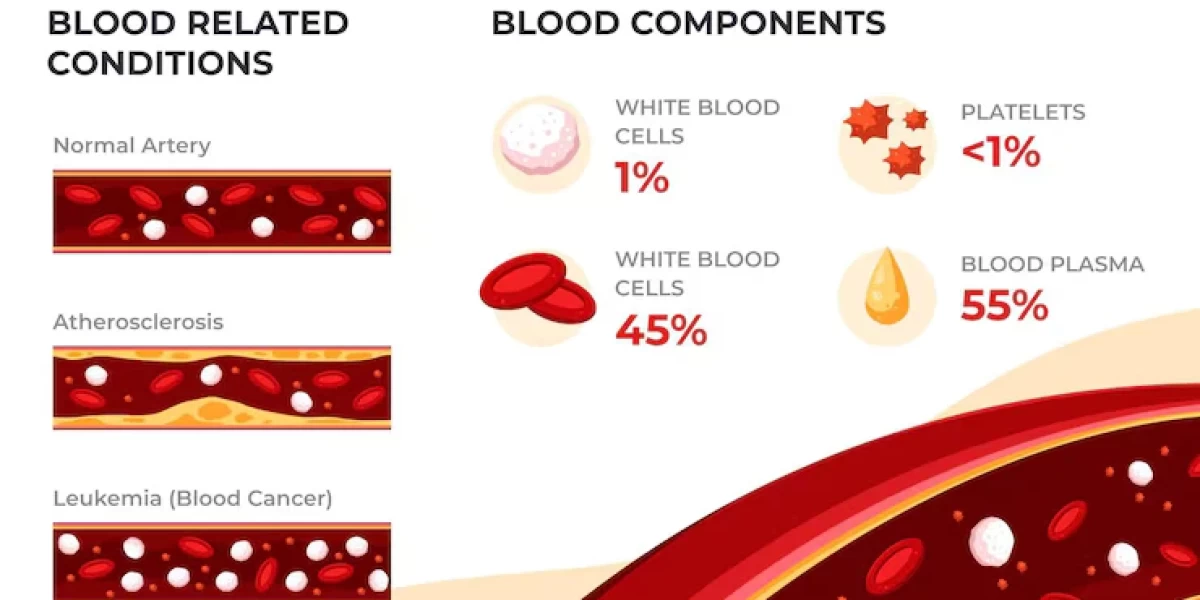
Amyotrophic lateral sclerosis (ALS), also known as motor neuron disease (MND) or Lou Gehrig’s disease, is a rare and terminal neurodegenerative disease that results in the progressive loss of motor neurons that control voluntary muscles. Motor neurons are nerve cells that extend from the brain to the spinal cord and from the spinal cord to the muscles throughout the body. When motor neurons degenerate and die, they stop sending signals to the muscles, causing them to weaken, atrophy, and eventually paralyze. ALS affects various parts of the body, such as the arms, legs, face, mouth, throat, and chest, and can impair the ability to move, speak, eat, and breathe. ALS usually starts in the hands, feet, arms, or legs, and then spreads to other regions of the body. The disease gets worse over time and has no cure. Most people with ALS die within 3 to 5 years after the onset of symptoms, usually from respiratory failure. ALS is often called Lou Gehrig’s disease after the famous baseball player who was diagnosed with it in 1939. ALS can affect anyone, anywhere, at any time, regardless of age, gender, race, or ethnicity. However, it is more common in people between 40 and 60 years old, and slightly more prevalent in men than in women. The exact cause of ALS is still unknown, but it is believed to involve a combination of genetic, environmental, and immunological factors. About 10% of ALS cases are inherited, while the rest are sporadic. ALS is one of the most common types of neurodegenerative diseases, along with Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease. Neurodegenerative diseases are characterized by the gradual and irreversible loss of neurons in the central nervous system, leading to cognitive, motor, and sensory impairments6. ALS is a devastating and incurable disease that affects not only the patients, but also their families, caregivers, and society. Therefore, it is important to raise awareness, support research, and provide care for people living with ALS.
Causes of ALS
The precise origin of ALS remains elusive, yet it is thought to encompass a mixture of genetic and environmental influences. Some of the main factors are:
- Genetic factors: About 10% of ALS cases are inherited, meaning that they are passed down from a parent to a child. These instances are referred to as familial amyotrophic lateral sclerosis (FALS). FALS can be caused by mutations in various genes that affect the function or survival of motor neurons. One of the most common gene mutations associated with FALS is the C9orf72 gene mutation, which accounts for about 40% of FALS cases and 5% to 10% of sporadic ALS cases. The C9orf72 gene mutation causes the formation of abnormal RNA and protein aggregates that may interfere with the normal functioning of motor neurons.
- Environmental factors: About 90% of ALS cases have no known genetic cause, and are known as sporadic ALS. These cases may be influenced by exposure to certain environmental factors that may trigger or worsen the disease. Some of the possible environmental factors are exposure to toxins, such as heavy metals, pesticides, or chemicals; trauma or physical injury, such as head injury, electric shock, or military service; and lifestyle factors, such as smoking, diet, or exercise. However, the evidence for these factors is not conclusive, and more research is needed to establish their role in ALS.
Symptoms of ALS
The symptoms of ALS vary from person to person, depending on which motor neurons are affected and how fast the disease progresses. The symptoms usually start in one part of the body, such as the arms, legs, face, or throat, and then spread to other regions over time. The symptoms can be classified into two categories: motor symptoms and non-motor symptoms. Some of the common symptoms are:
- Motor symptoms: These are the symptoms that affect the voluntary muscles, such as the muscles that control movement, speech, swallowing, and breathing. The motor symptoms of ALS include muscle weakness, which is the most common initial symptom and can affect any part of the body; difficulty speaking or swallowing, which can cause slurred speech, drooling, choking, or malnutrition; and muscle cramps and twitching, which can cause pain, stiffness, or spasms. The motor symptoms of ALS can lead to disability, paralysis, and respiratory failure.
- Non-motor symptoms: These are the symptoms that affect other aspects of the nervous system, such as the cognitive, emotional, and behavioral functions. The non-motor symptoms of ALS include cognitive changes, which can affect memory, attention, language, or executive functions; and emotional and behavioral changes, which can cause mood swings, depression, anxiety, apathy, or impulsivity. The non-motor symptoms of ALS can affect the quality of life, social relationships, and mental health of the patients and their caregivers.
Diagnosis of ALS
Diagnosing ALS is not easy, as there is no single test that can confirm the disease. A healthcare provider, such as a neurologist, will take a full medical history, conduct a physical exam, and order more specific tests to rule out other conditions that may mimic ALS or to support the diagnosis of ALS. Some of the tests that may be done are:
- Clinical evaluation: This involves a thorough examination of the person’s neurological function, such as reflexes, muscle strength, coordination, balance, sensation, and speech. The health care provider will also ask about the person’s symptoms, such as when they started, how they progressed, and how they affect the person’s daily activities. The clinical evaluation can help identify the pattern and extent of motor neuron involvement, as well as the presence of any non-motor symptoms, such as cognitive or emotional changes.
- Electromyography (EMG) and nerve conduction studies: These are tests that measure the electrical activity of the muscles and nerves. EMG involves inserting a thin needle electrode into various muscles and recording the signals that are generated when the muscles contract or relax. Nerve conduction studies involve attaching electrodes to the skin and stimulating the nerves with small electric shocks, and measuring the speed and strength of the nerve impulses. These tests can help detect the signs of motor neuron degeneration, such as reduced or abnormal muscle or nerve signals, and differentiate between upper and lower motor neuron involvement.
- Magnetic resonance imaging (MRI) and computerized tomography (CT) scans: These are imaging tests that produce detailed pictures of the brain and spinal cord. MRI uses a strong magnetic field and radio waves, while CT uses X-rays and a computer. These tests can help rule out other causes of the symptoms, such as tumors, infections, strokes, or injuries, that may affect the brain or spinal cord. They can also sometimes reveal the changes that are associated with ALS, such as atrophy or scarring of the motor cortex or the corticospinal tract.
Best Treatment for ALS
There is no cure for ALS, but there are treatments that can help slow down the progression of the disease, relieve the symptoms, prevent complications, and improve the quality of life of the person with ALS. The treatment plan is individualized and may involve a team of healthcare professionals, such as neurologists, physiatrists, respiratory therapists, speech therapists, physical therapists, occupational therapists, nutritionists, social workers, and psychologists. Some of the common treatments for ALS are:
- Symptomatic management: This involves using medications and therapies to address the specific symptoms that the person with ALS experiences, such as muscle spasms, pain, stiffness, cramps, twitching, drooling, depression, anxiety, or insomnia. Some of the medications that may be prescribed are antispasmodics, such as baclofen or tizanidine; analgesics, such as ibuprofen or acetaminophen; antidepressants, such as fluoxetine or sertraline; or sedatives, such as lorazepam or zolpidem. Some of the therapies that may be recommended are speech therapy, to help with communication and swallowing difficulties; physical therapy, to help with mobility and exercise; and occupational therapy, to help with daily activities and adaptive equipment.
- Supportive care: This involves using devices and interventions to assist the person with ALS with their breathing, feeding, and mobility needs, as the disease progresses and affects their ability to perform these functions independently. Some of the devices that may be used are braces, splints, canes, walkers, wheelchairs, or lifts, to help with muscle weakness and paralysis; feeding tubes, to help with nutrition and hydration; and noninvasive or invasive ventilation, to help with respiratory failure. The decision to use these devices depends on the person’s preferences, goals, and values, and should be discussed with the health care provider and the family or caregivers.
- Experimental treatments and clinical trials: These are treatments that are not yet approved by the Food and Drug Administration (FDA), but are being tested for their safety and effectiveness in treating ALS. Some of the experimental treatments that are currently being explored are riluzole and edaravone, which are the only two drugs that have been shown to slow down the progression of ALS by modulating the glutamate neurotransmission or reducing the oxidative stress; stem cell therapy, which involves transplanting stem cells into the spinal cord or the brain to replace the damaged motor neurons or support their survival; gene therapy, which involves delivering genes that can correct the genetic defects or modulate the expression of the genes that are involved in ALS; and immunotherapy, which involves using antibodies or vaccines to target the immune system or the inflammatory pathways that may contribute to ALS. Clinical trials are research studies that enroll people with ALS who are willing to try these experimental treatments and compare them with the standard treatments or placebos. Clinical trials are essential for advancing knowledge and finding new treatments for ALS, but they also involve potential risks and benefits that should be carefully considered before participating.
Palliative Care and Quality of Life
Palliative care is a type of care that focuses on improving the quality of life of people with life-limiting illnesses, such as ALS, and their families. Palliative care aims to relieve the physical, emotional, psychological, and spiritual suffering that may accompany the disease. Palliative care can be provided by a team of healthcare professionals, such as doctors, nurses, social workers, counselors, chaplains, and volunteers, who work together to address the needs and preferences of the person with ALS and their caregivers. Palliative care can be offered at any stage of the disease, along with other treatments, and can be delivered in various settings, such as home, hospital, hospice, or long-term care facility. Some of the aspects of palliative care for ALS are:
- Emotional and psychological support: People with ALS and their families may experience a range of emotions and psychological challenges, such as fear, anger, sadness, guilt, anxiety, depression, grief, or loss of meaning and purpose. Palliative care can provide emotional and psychological support through counseling, therapy, education, and support groups, to help them cope with these feelings and adjust to the changes and losses caused by the disease. Palliative care can also help them maintain their dignity, autonomy, and identity, and enhance their well-being and resilience.
- Hospice care: Hospice care is a specialized form of palliative care that is offered to people with ALS who have a life expectancy of six months or less, and who have decided to stop or limit life-prolonging treatments. Hospice care focuses on providing comfort and quality of life, rather than curing the disease. Hospice care can be provided by a team of hospice professionals and volunteers, who offer medical, nursing, social, spiritual, and bereavement care, as well as practical assistance and respite care, to the person with ALS and their family. Hospice care can be delivered in the person’s home, or in a hospice facility, depending on their needs and wishes. Hospice care can help the person with ALS die with dignity, peace, and comfort, and support their family during and after the dying process.
- End-of-life decision making: People with ALS and their families may face difficult decisions about their end-of-life care, such as whether to use feeding tubes, ventilation devices, or cardiopulmonary resuscitation, or where and how they want to die. Palliative care can help them make informed and personalized decisions, based on their values, beliefs, and goals, and communicate their wishes to their healthcare providers and loved ones. Palliative care can also help them complete advance directives, such as living wills or health care proxies, that specify their preferences and designate a surrogate decision-maker, in case they lose their ability to speak or make decisions. Palliative care can also help them resolve any conflicts or ethical dilemmas that may arise, and respect their choices and rights.
Prevention of ALS
There is no known way to prevent ALS, as the exact cause of the disease is still unclear. However, some studies have suggested that certain factors may reduce the risk or delay the onset of ALS, such as eating a diet rich in antioxidants, such as carotenoids, that can protect the neurons from oxidative stress and inflammation; avoiding exposure to toxins, such as heavy metals, pesticides, or chemicals, that may damage the neurons or the immune system; and maintaining a healthy lifestyle, such as exercising moderately, quitting smoking, and limiting alcohol consumption, that can improve the overall health and well-being. However, these factors are not conclusive, and more research is needed to establish their role in ALS prevention.
Therefore, the best way to prevent ALS is to raise awareness and advocate for more research funding and support for the disease. ALS is a rare and complex disease that is often underdiagnosed, underreported, and underfunded. By increasing the public and professional knowledge and understanding of ALS, more people with ALS can be identified and treated earlier, and more resources can be allocated to finding the cause, cure, and effective treatments for ALS. By advocating for more research funding and support, more scientists and clinicians can be motivated and enabled to conduct high-quality and innovative research on ALS, and more people with ALS can participate in clinical trials and benefit from new discoveries and therapies. By raising awareness and advocacy, more people with ALS can have access to better care and services, and more hope and dignity
Conclusion
ALS is a devastating and incurable disease that affects both the upper and lower motor neurons, leading to paralysis and death. The diagnosis of ALS is based on clinical evaluation, electromyography, nerve conduction studies, and magnetic resonance imaging, and computerized tomography scans. The treatment of ALS depends on symptomatic management, supportive care, experimental treatments, and clinical trials. The palliative care and quality of life of ALS involve emotional and psychological support, hospice care, and end-of-life decision-making. The prevention of ALS involves the lack of definitive preventive measures and the awareness and advocacy for research funding. The management of ALS requires a multidisciplinary care and support team, that can address the physical, emotional, psychological, and spiritual needs of the person with ALS and their family, and help them achieve their goals and preferences. By working together, the person with ALS, their family, and their healthcare providers can improve the quality of life and the quality of death of the person with ALS and hope for a better future.
FAQ
- Q: What is ALS and how does it affect the body?
- A: ALS, or amyotrophic lateral sclerosis, is a degenerative disease that affects the nerve cells in the brain and spinal cord that control voluntary muscle movements, such as chewing, walking, and talking. As these nerve cells die, the muscles get weaker and eventually paralyze. ALS affects various parts of the body, such as the arms, legs, face, mouth, throat, and chest, and can impair the ability to move, speak, eat, and breathe. There is no remedy for this incurable ailment.
- Q: What are the causes and risk factors of ALS?
- A: The exact cause of ALS is still unknown, but it is believed to involve a combination of genetic and environmental factors. About 10% of ALS cases are inherited, meaning that they are passed down from a parent to a child. These instances are referred to as familial Amyotrophic Lateral Sclerosis (FALS). FALS can be caused by mutations in various genes that affect the function or survival of motor neurons. One of the most common gene mutations associated with FALS is the C9orf72 gene mutation. About 90% of ALS cases have no known genetic cause and are known as sporadic ALS. These cases may be influenced by exposure to certain environmental factors that may trigger or worsen the disease, such as toxins, trauma, or lifestyle factors. However, the evidence for these factors is not conclusive, and more research is needed to establish their role in ALS. Some of the established risk factors for ALS are age, gender, race, ethnicity, and family history. ALS is more common in people between 40 and 60 years old, and slightly more prevalent in men than in women. ALS can affect anyone, anywhere, at any time, regardless of age, gender, race, or ethnicity.
- Q: What are the symptoms and complications of ALS?
- A: The symptoms of ALS vary from person to person, depending on which nerve cells are affected and how fast the disease progresses. The symptoms usually start in one part of the body, such as the arms, legs, face, or throat, and then spread to other regions over time. The symptoms can be classified into two categories: motor symptoms and non-motor symptoms. The motor symptoms of ALS include muscle weakness, difficulty speaking or swallowing, muscle cramps and twitching, and respiratory failure. The non-motor symptoms of ALS include cognitive changes, emotional and behavioral changes, and pain. The symptoms of ALS can lead to various complications, such as infections, malnutrition, dehydration, pressure sores, blood clots, depression, anxiety, and impaired quality of life.
- Q: How is ALS diagnosed?
- A: Diagnosing ALS is not easy, as there is no single test that can confirm the disease. A healthcare provider, such as a neurologist, will take a full medical history, conduct a physical exam, and order more specific tests to rule out other conditions that may mimic ALS or to support the diagnosis of ALS. Some of the tests that may be done are clinical evaluation, electromyography (EMG) and nerve conduction studies, and magnetic resonance imaging (MRI) and computerized tomography (CT) scans. The clinical evaluation involves a thorough examination of the person’s neurological function, such as reflexes, muscle strength, coordination, balance, sensation, and speech. The EMG and nerve conduction studies measure the electrical activity of the muscles and nerves and can help detect the signs of motor neuron degeneration. The MRI and CT scans produce detailed pictures of the brain and spinal cord and can help rule out other causes of the symptoms, such as tumors, infections, strokes, or injuries.
- Q: What are the best treatments and management strategies for ALS?
- A: There is no cure for ALS, but there are treatments and management strategies that can help slow down the progression of the disease, relieve the symptoms, prevent complications, and improve the quality of life of the person with ALS and their family. The treatment and management plan is individualized and may involve a team of healthcare professionals, such as neurologists, physiatrists, respiratory therapists, speech therapists, physical therapists, occupational therapists, nutritionists, social workers, and psychologists. Some of the common treatments and management strategies for ALS are symptomatic management, supportive care, experimental treatments and clinical trials, and palliative care and quality of life. Symptomatic management involves using medications and therapies to address the specific symptoms that the person with ALS experiences, such as muscle spasms, pain, stiffness, cramps, twitching, drooling, depression, anxiety, or insomnia. The supportive care involves using devices and interventions to assist the person with ALS with their breathing, feeding, and mobility needs, as the disease progresses and affects their ability to perform these functions independently. The experimental treatments and clinical trials involve testing new drugs or therapies that may slow down the disease or improve the symptoms, such as riluzole, edaravone, stem cell therapy, gene therapy, or immunotherapy. The palliative care and quality of life involve providing emotional, psychological, spiritual, and end-of-life support to the person with ALS and their family, and helping them cope with the disease and its impact.
- Q: How can ALS be prevented?
- A: There is no known way to prevent ALS, as the exact cause of the disease is still unclear. However, some studies have suggested that certain factors may reduce the risk or delay the onset of ALS, such as eating a diet rich in antioxidants, avoiding exposure to toxins, and maintaining a healthy lifestyle. However, these factors are not conclusive, and more research is needed to establish their role in ALS prevention. Therefore, the best way to prevent ALS is to raise awareness and advocate for more research funding and support for the disease. ALS is a rare and complex disease that is often underdiagnosed, underreported, and underfunded. By increasing the public and professional knowledge and understanding of ALS, more people with ALS can be identified and treated earlier, and more resources can be allocated to finding the cause, cure, and effective treatments for ALS. By advocating for more research funding and support, more scientists and clinicians can be motivated and enabled to conduct high-quality and innovative research on ALS, and more people with ALS can participate in clinical trials and benefit from new discoveries and therapies. By raising awareness and advocacy, more people with ALS can have access to better care and services, and more hope and dignity.
- Q: What are the challenges and difficulties that people with ALS face?
- A: People with ALS face many challenges and difficulties, such as physical, emotional, psychological, social, and financial. Physically, they have to deal with the loss of muscle function and independence, and the need for constant care and assistance. Emotionally, they have to cope with the fear, anger, sadness, grief, and loss of meaning and purpose that the disease brings. Psychologically, they have to adjust to the changes and losses caused by the disease, and maintain their dignity, autonomy, and identity. Socially, they have to communicate and interact with their family, friends, and health care providers, and deal with the stigma and isolation that the disease may cause. Financially, they have to manage the costs and expenses of the disease, such as medical bills, equipment, medications, and home modifications.
- Q: What are the resources and support available for people with ALS and their families?
- A: There are many resources and support available for people with ALS and their families, such as health care providers, organizations, websites, books, and magazines, that provide information, education, advice, guidance, or tools for diagnosis, treatment, management, and coping with ALS. Some of the examples are:
- The ALS Association, which is a national nonprofit organization that funds research, provides care and services, and advocates for people with ALS and their families.
- The Muscular Dystrophy Association, which is a voluntary health agency that supports research, care, and education for people with neuromuscular diseases, including ALS.
- The National Institute of Neurological Disorders and Stroke, which is a federal agency that conducts and supports research, education, and training on neurological disorders, including ALS.
- The ALS Therapy Development Institute, which is a nonprofit biotechnology organization that is dedicated to finding effective treatments and cures for ALS.
- The ALS Untangled, which is a research network that reviews alternative and off-label treatments for ALS.
- The ALS Forum, which is an online platform that connects researchers, clinicians, patients, and caregivers, and provides news, resources, and discussions on ALS.
- The ALS Ice Bucket Challenge, which is a viral social media campaign that raises awareness and funds for ALS research.
- The Living with ALS Resource Guides, which are a series of publications that provide practical information and strategies for people with ALS and their families.
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.