Ablation is a medical procedure that uses heat, cold, or other forms of energy to destroy abnormal tissue in the body. Ablation can be used to treat various health conditions, especially those that affect the heart rhythm. If you or someone you love has been diagnosed with a heart rhythm disorder, such as atrial fibrillation, atrial flutter, or ventricular tachycardia, you may be wondering what ablation is and how it can help. In this article, we will explain the basics of ablation, the benefits and risks, the preparation and recovery, and some frequently asked questions. By the end of this article, you will have a better understanding of what to expect before, during, and after an ablation procedure.
What is Ablation and Why is it Done?
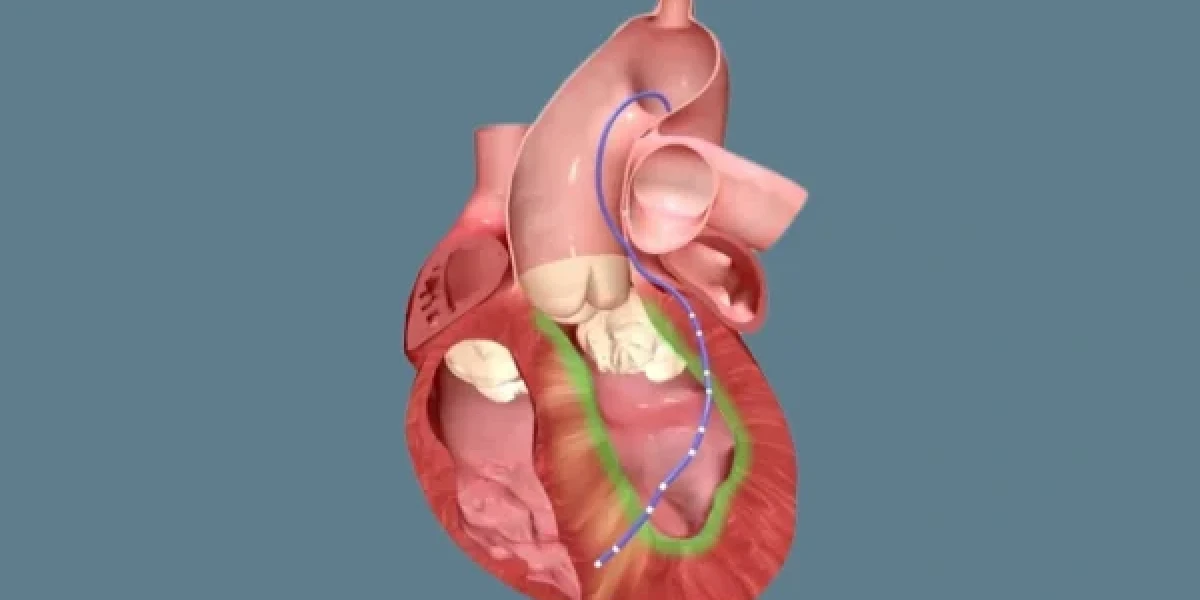
Ablation is a procedure that aims to restore a normal heart rhythm by creating small scars in the heart tissue that are causing abnormal electrical signals. These scars block the pathways of the erratic impulses and prevent them from reaching the rest of the heart. Ablation can be done using different types of energy, such as radiofrequency (heat), cryoablation (cold), or laser (light). The most common type of ablation is catheter ablation, which is a minimally invasive procedure that involves inserting thin, flexible tubes called catheters through the blood vessels and into the heart. The catheters have electrodes at their tips that deliver the energy to the targeted areas. Ablation can also be done surgically, which requires opening the chest and accessing the heart directly. Surgical ablation is usually done in combination with other heart surgeries, such as valve repair or replacement.
Ablation is done to treat various types of heart rhythm disorders, also known as arrhythmias. Arrhythmias occur when the electrical signals that control the heartbeat become irregular, too fast, or too slow. Some of the most common arrhythmias that can be treated with ablation are:
- Atrial fibrillation (AFib): This is the most common type of arrhythmia, affecting about 33 million people worldwide. AFib occurs when the upper chambers of the heart (the atria) quiver instead of contracting normally. This causes the blood to pool and clot in the atria, increasing the risk of stroke and heart failure.
- Atrial flutter: This is a similar condition to AFib, but the atria beat faster and more regularly. Atrial flutter can also lead to blood clots and stroke.
- Supraventricular tachycardia (SVT): This is a condition where the heart beats abnormally fast due to a problem in the electrical system of the upper part of the heart. SVT can cause symptoms such as palpitations, chest pain, shortness of breath, and fainting.
- Ventricular tachycardia (VT): This is a condition where the lower chambers of the heart (the ventricles) beat very fast and out of sync with the atria. VT can be life-threatening, as it can cause the heart to stop pumping blood effectively, leading to cardiac arrest.
Ablation is usually recommended when other treatments, such as medications or pacemakers, have failed to control the arrhythmia or have caused unacceptable side effects. Ablation can also be the first choice of treatment for some types of arrhythmias that respond well to the procedure, such as Wolff-Parkinson-White syndrome and some forms of SVT.
Who is a Candidate for Ablation and How is it Evaluated?
Not everyone with a heart rhythm disorder is a suitable candidate for ablation. Your doctor will evaluate your condition and determine if ablation is right for you based on several factors, such as:
- The type, frequency, and severity of your arrhythmia
- The impact of your arrhythmia on your quality of life and daily activities
- The results of your previous treatments, such as medications or devices
- The presence of any other heart problems, such as coronary artery disease or heart valve disease
- The presence of any other medical conditions, such as kidney disease or bleeding disorders
- Your age and overall health status
Before you undergo ablation, you will need to have some tests and assessments to confirm your diagnosis and plan your procedure. These may include:
- Electrocardiogram (ECG): This is a test that records the electrical activity of your heart using electrodes attached to your chest, arms, and legs. It can show the type and pattern of your arrhythmia and identify any other heart problems.
- Echocardiogram: This is a test that uses sound waves to create a picture of your heart and its structures. It can measure the size, shape, and function of your heart and detect any abnormalities, such as blood clots or valve problems.
- Holter monitor: This is a device that you wear for 24 to 48 hours to record your heart rhythm continuously. It can help to capture any episodes of arrhythmia that may not show up on a regular ECG.
- Event monitor: This is a device that you wear for a longer period, usually a few weeks or months, to record your heart rhythm when you have symptoms. You can activate the device manually or it can be triggered automatically by an abnormal heart rate.
- Electrophysiology study (EPS): This is a test that involves inserting catheters into your heart and stimulating it with electrical impulses to map the source and pathway of your arrhythmia. It can help to pinpoint the exact location and extent of the abnormal tissue that needs to be ablated.
You will also need to discuss your medical history and current medications with your doctor and inform them of any allergies or previous reactions to anesthesia or contrast dye. Your doctor will explain the risks and benefits of ablation and answer any questions you may have. You will need to sign a consent form before the procedure.
What are the Risks and Benefits of Ablation?
Like any medical procedure, ablation has some potential risks and benefits that you should weigh carefully before deciding to have it. The risks and benefits may vary depending on the type and extent of your ablation, your underlying heart condition, and your individual response to the procedure.
Some of the possible risks of ablation are:
- Draining or contamination at the site where the catheter was embedded
- Damage to the blood vessels, heart valves, or heart muscle
- Development of new or worse arrhythmias
- Slow heart rate that may require a pacemaker
- Blood clots that can travel to the lungs or brain and cause pulmonary embolism or stroke
- Narrowing or blockage of the veins that carry blood between the lungs and heart (pulmonary vein stenosis)
- Damage to the kidneys from the contrast dye used during the procedure
- Death in rare cases
Some of the possible benefits of ablation are:
- Restoration of a normal and stable heart rhythm
- Reduction or elimination of the need for medications or devices
- Improvement of the symptoms and quality of life
- Prevention of serious complications, such as stroke or heart failure
- Reduction of the risk of hospitalization or death
Your doctor will discuss with you the likelihood and severity of the risks and benefits of ablation in your specific case and help you make an informed decision. You should also consider the alternative treatment options and their pros and cons. For example, some people may prefer to continue taking medications or using devices to control their arrhythmia, while others may opt for a more invasive surgery or a heart transplant.
How to Prepare for the Procedure?
To prepare for the ablation procedure, you will need to follow some instructions and precautions, such as:
- Stop eating and drinking at least six hours before the procedure
- Stop taking certain medications, such as blood thinners, antiarrhythmics, or diabetes drugs, as instructed by your doctor
- Bring a list of all your medications, including over-the-counter drugs, supplements, and herbal remedies, to the hospital
- Plan for a designated driver to take you home following the procedure.
- Wear agreeable and baggy apparel and leave any gems or resources at home
On the day of the procedure, you will be admitted to the hospital and taken to the electrophysiology (EP) lab, where the ablation will be performed. You will change into a hospital gown and have an intravenous (IV) line inserted into your arm. You will also have electrodes attached to your chest to monitor your heart rhythm and blood pressure.
You will receive either local anesthesia with sedation or general anesthesia, depending on the type and duration of the ablation. Your doctor will then insert one or more catheters through a small incision in your groin, neck, or arm and guide them to your heart using X-ray or ultrasound imaging. Your doctor will then deliver energy through the catheters to create scars in the targeted areas of your heart. You may feel some pressure, discomfort, or warmth during the procedure, but you should not feel any pain.
The ablation procedure usually takes two to four hours, depending on the type and complexity of the arrhythmia. After the procedure, your doctor will remove the catheters and apply pressure or a bandage to the incision site to prevent bleeding. You will then be taken to a recovery room or a hospital ward, where you will be monitored for several hours or overnight.
Recovery and Follow-Up
After the ablation procedure, you will need to follow some guidelines and instructions for your recovery and follow-up, such as:
- Rest in bed for four to six hours and avoid moving your leg or arm where the catheter was inserted
- Drink plenty of fluids to flush out the contrast dye from your kidneys
- Resume your normal diet and medications, unless otherwise instructed by your doctor
- Avoid strenuous activities, such as lifting, driving, or exercising, for a few days or weeks, depending on your doctor’s advice
- Keep the incision site clean and dry and watch for any signs of infection, such as redness, swelling, pain, or fever
- Report any chest pain, shortness of breath, irregular heartbeat, or bleeding to your doctor immediately
You will also need to have regular follow-up appointments with your doctor to check your heart rhythm and function and evaluate the effectiveness of the ablation. You may need to wear a Holter monitor or an event monitor for a few days or weeks after the procedure to record your heart activity. You may also need to take medications, such as blood thinners or antiarrhythmics, for some time after the procedure to prevent blood clots or arrhythmias.
The success rate of ablation varies depending on the type and location of the arrhythmia, but it is generally high, ranging from 70% to 90%. However, some people may need more than one ablation procedure to achieve a lasting effect. Some people may also experience a recurrence of their arrhythmia after a period of time, which may require another ablation or medication.
Conclusion
Ablation is a medical procedure that uses energy to destroy abnormal tissue in the heart that causes arrhythmias. Ablation can restore a normal or near-normal heart rhythm, reduce or eliminate the symptoms of arrhythmia, improve the quality of life and daily activities, and reduce the risk of stroke, heart failure, or sudden cardiac death.
However, ablation is not suitable for everyone who has an arrhythmia, and it has some potential risks and complications, such as bleeding, infection, damage to the heart, blood clots, stroke, or heart attack. Therefore, it is important to understand the key aspects of ablation, such as its purpose, benefits, risks, preparation, and recovery, before undergoing the procedure.
You should also communicate openly with your doctor and healthcare team and ask any questions or concerns you may have. They will provide you with the best information and guidance for your specific case and help you make an informed decision about ablation.
FAQ
Here are some frequently asked questions and answers about ablation:
- Q: How long does it take to recover from ablation?
- A: The recovery time from ablation varies depending on the type and location of the ablation, the individual characteristics and conditions of the patient, and the post-procedure care and guidelines. Generally, most people can resume their normal activities within a few days or weeks after the procedure, but some people may need longer to heal and recover.
- Q: Will I need to take medications after ablation?
- A: Some people may need to take medications, such as blood thinners or antiarrhythmics, for some time after ablation to prevent blood clots or arrhythmias. Your doctor will advise you on the type, dose, and duration of the medications you need to take and monitor your response and side effects.
- Q: Will I need to have a pacemaker or defibrillator after ablation?
- A: Some people may need to have a pacemaker or defibrillator implanted after ablation to regulate their heart rhythm and prevent sudden cardiac arrest. This may be the case if the ablation causes a complete heart block, which is a condition where the electrical signals from the upper to the lower chambers of the heart are interrupted, or if the ablation does not eliminate the risk of life-threatening arrhythmias, such as ventricular fibrillation. Your doctor will assess your need for a pacemaker or defibrillator and explain the benefits and risks of these devices.
- Q: How can I prevent arrhythmias from recurring after ablation?
- A: Ablation can reduce or eliminate the occurrence of arrhythmias, but it does not cure the underlying causes or risk factors of arrhythmias, such as heart disease, high blood pressure, diabetes, obesity, smoking, or stress. Therefore, it is important to adopt a healthy lifestyle and follow your doctor’s recommendations to prevent or manage these conditions and reduce the risk of arrhythmias from recurring after ablation. You can implement alterations to your lifestyle, such as:
- Eating a balanced and nutritious diet that is low in salt, fat, cholesterol, and sugar
- Exercising regularly and moderately, as advised by your doctor
- Maintaining a healthy weight and body mass index (BMI)
- Ceasing tobacco use and steering clear of secondhand smoke
- Limiting or avoiding alcohol and caffeine intake
- Effectively coping with stress and engaging in relaxation practices, such as meditation, yoga, or breathing exercises.
- Getting enough sleep and rest
- Following up with your doctor regularly and taking your medications as prescribed
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.