Introduction
Wallenberg Syndrome, also known as lateral medullary syndrome or posterior inferior cerebellar artery (PICA) syndrome, is a neurological condition that affects the brainstem. It is named after the Swedish neuroscientist Raoul Wallenberg‚ who made significant contributions to our understanding of this syndromeꓸ This article provides an in-depth exploration of Wallenberg Syndrome‚ covering its symptoms, causes diagnosis blood tests‚ best treatment options , and preventive measures.
Background
Wallenberg Syndromeꓹ also known as Lateral Medullary Syndrome or posterior inferior cerebellar artery (PICA) syndrome, is a neurological condition that primarily affects the brainstemꓸ Its recognition and understanding have evolved over the years, with significant contributions from medical pioneers.
The syndrome is named after the Swedish neurologist, János Wallenberg٫ who made substantial contributions to the field of neurology in the early 20th century. Drꓸ Wallenberg's work laid the foundation for the identification and description of the characteristic symptoms associated with this syndrome․ In the early 1900s, he conducted extensive research on patients with brainstem lesions٫ and his observations led to the identification of the clinical features that are now recognized as Wallenberg Syndrome.
Wallenberg's groundbreaking work shed light on the distinct symptoms and underlying mechanisms of this neurological disorder. His research paved the way for subsequent advancements in understanding the condition, its anatomical basis, and the development of diagnostic and treatment protocols.
Brief anatomy of the brainstem
To comprehend Wallenberg Syndrome fully it is essential to have a basic understanding of the brainstem‚ as this is where the syndrome primarily originates․ The brainstem is a crucial part of the central nervous system connecting the brain to the spinal cord․ It is responsible for regulating various vital functions, including breathing, heart rate٫, and basic motor control.
The brainstem is divided into three major regions: the medulla oblongata, the pons, and the midbrain․ Wallenberg Syndrome primarily affects the medulla oblongata, which is the lowest part of the brainstem. This region is responsible for controlling several critical functions, such as swallowing, speech, and the sensation of touch and pain in the face.
The medulla oblongata is also involved in regulating important autonomic functions including blood pressure heart rate and respiration․ Damage to this region, which can occur in Wallenberg Syndrome, can disrupt these functions and result in a wide range of neurological symptoms.
Explanation of the affected brain structures
Wallenberg Syndrome occurs due to damage to specific brain structures within the medulla oblongata٫ often caused by a blockage or disruption of blood flow in the posterior inferior cerebellar artery (PICA)․ This artery supplies oxygen-rich blood to the medulla and other parts of the brainstem.
When the PICA is compromised‚ it can lead to a cascade of neurological symptoms. The affected structures in the medulla oblongata include the spinal trigeminal nucleus, the nucleus ambiguus‚, and the descending sympathetic pathway.
Spinal Trigeminal Nucleus: This structure plays a crucial role in processing sensory information from the face including pain and temperature sensations. Damage to this area can result in facial pain and numbness on one side of the face a characteristic symptom of Wallenberg Syndrome.
Nucleus ambiguus: This nucleus is responsible for controlling the muscles involved in swallowing and speech. Dysfunction of the nucleus ambiguus can lead to difficulties in swallowing and slurred speech, which are also common symptoms of the syndrome.
Descending Sympathetic Pathway: The medulla contains a sympathetic pathway that regulates blood pressure and heart rate Damage to this pathway can lead to fluctuations in blood pressure often resulting in dizziness and lightheadedness.
Understanding the affected brain structures is vital for diagnosing and managing Wallenberg Syndrome. Medical professionals use this knowledge to identify the specific symptoms experienced by individuals with the condition and tailor treatment strategies to address their unique needs.
Symptoms of Wallenberg Syndrome
Wallenberg Syndrome, also known as lateral medullary syndromeꓹ is a rare neurological condition caused by a disruption of blood flow to a specific area of the brainstem, known as the lateral medullaꓸ This disruption leads to a variety of symptoms that can significantly affect a person's daily lifeꓸ In this articleꓹ we will explore the common symptoms of Wallenberg Syndrome, their severity and variability, and the profound impact they have on daily life.
A. List of Common Symptoms
Wallenberg Syndrome's symptoms result from the damage to the various structures within the lateral medulla٫ and they can vary in their presentation Some of the most common symptoms include:
Dysphagia: Individuals with Wallenberg Syndrome often experience difficulty swallowing‚ known as dysphagia․ Which can lead to choking, aspirationꓹ, and the need for altered diets or feeding tubes to prevent complications.
Vertigo and Nausea: Vertigoꓹ a spinning sensationꓹ and persistent nausea are frequent symptoms. These can be distressing and affect a person's ability to perform daily tasks.
Nystagmus: Involuntary, rapid eye movements, known as nystagmus, are common in Wallenberg Syndromeꓸ This can lead to difficulties with visual stability‚ coordination, and balance.
Hoarseness and Dysphonia: Damage to the nerves responsible for vocal cord function can lead to changes in voice quality, often resulting in hoarseness or dysphonia.
Facial Pain and Sensory Changes: Patients may experience facial pain or altered sensations on one side of the face This can range from mild discomfort to severe pain.
Horner's Syndrome: This syndrome can lead to drooping eyelids, constricted pupils, and decreased sweating on one side of the face.
Ipsilateral Ataxia: Ipsilateral limb ataxia refers to a lack of coordination and control on the same side of the body as brainstem damage. It can lead to difficulties with fine motor skills.
Contralateral Sensory Loss: On the opposite side of the body there may be sensory deficits‚ including numbness‚ tingling, or loss of sensation.
Hiccups: Prolonged, intractable hiccups can be a surprising symptom of Wallenberg Syndrome‚ and they can be quite bothersome.
Dizziness and Unsteadiness: Patients often report dizziness and a sense of unsteadiness when walking or standing, making mobility a challenge.
Bꓸ Severity and Variability of Symptoms
One notable aspect of Wallenberg Syndrome is the variability in symptom severity and presentation among affected individuals The severity of symptoms can range from mild to debilitating. Factors contributing to this variability include the location and extent of the brainstem damage, the cause of the condition (ischemic or hemorrhagic), and an individual's overall health.
In some cases‚ symptoms may be relatively mild, causing minimal disruption to daily life. Patients may adapt to changes in swallowing or balance with therapy and support However, in severe cases, symptoms can be profoundly debilitating, requiring extensive medical intervention and rehabilitation.
The variability in symptom presentation also means that healthcare providers must carefully evaluate each patient's condition and tailor their treatment and support accordingly This individualized approach is essential to address the unique challenges each person with Wallenberg Syndrome faces.
Cꓸ Impact on Daily Life
The symptoms of Wallenberg Syndrome can have a profound impact on a person's daily life They can affect not only physical health but also emotional and social well-being The challenges posed by dysphagiaꓹ dizziness‚ and sensory deficits can make simple tasks such as eating or walking, extremely difficult.
Additionally, the emotional toll of living with Wallenberg Syndrome should not be underestimatedꓸ Patients may experience frustrationꓹ anxiety٫ and depression as they grapple with the limitations imposed by their condition Coping with changes in appearance voice٫ and physical abilities can be emotionally challenging.
The impact extends beyond the affected individual to their caregivers and support network Caregivers may need to provide assistance with daily activities and they too‚ can experience stress and emotional strain.
Diagnosis
Wallenberg Syndromeꓹ a neurological condition named after the German neurologist Otto Wallenberg‚ affects the brainstem and can lead to a range of debilitating symptoms. Understanding the causes of this syndrome is crucial for both healthcare professionals and the general public. In this section, we will delve into the various causes of Wallenberg Syndrome٫ including ischemic and hemorrhagic factors, thrombosis, and embolism, as well as the risk factors associated with the development of this condition.
A․ Ischemic vsꓸ Hemorrhagic Causes
One of the primary distinctions in the causes of Wallenberg Syndrome lies in whether it is triggered by ischemia or hemorrhage․ Ischemic Wallenberg Syndrome occurs when a specific blood vessel supplying the brainstem becomes obstructed‚ leading to a reduced blood flow and oxygen deprivation in that region. This can result from the formation of a blood clot within the vessel or the narrowing of the blood vessel itself. In contrast, hemorrhagic Wallenberg Syndrome is caused by bleeding into the brainstem‚ often due to a ruptured blood vessel․ Both types of causes can have severe consequences, and it is essential to identify them accurately for appropriate treatment.
B. Thrombosisꓹ Embolism٫ and Other Contributing Factors
Thrombosis and embolism are common causes of ischemic Wallenberg Syndrome. Thrombosis refers to the formation of blood clots within a blood vesselꓹ usually in the vertebral or posterior inferior cerebellar arteries٫ which supply the brainstemꓸ These clots can obstruct blood flow, leading to ischemia and subsequent neurological symptoms․ Embolismꓹ on the other hand‚ involves the travel of a blood clot from another part of the body‚ often originating in the heart, to the brainstem's blood vessels‚ causing a blockage.
Other contributing factors may include atherosclerosisꓹ a condition characterized by the accumulation of fatty deposits in the arteries٫ which can lead to narrowing or blockage of the blood vessels supplying the brainstem․ In some cases‚ Wallenberg Syndrome can also result from dissection of the vertebral artery, which is a separation of the layers of the artery wall, leading to impaired blood flow. The exact cause may vary among individuals making accurate diagnosis and understanding of these factors critical.
C․ Risk Factors for Developing Wallenberg Syndrome
Several risk factors increase the likelihood of developing Wallenberg Syndrome. These factors can contribute to the underlying conditions that lead to thrombosis٫ embolismꓹ or other causes of the syndromeꓸ Common risk factors include:
Hypertension: High blood pressure can damage the walls of blood vesselsꓹ making them more susceptible to clot formation or rupture٫ leading to Wallenberg Syndrome.
Smoking: Smoking not only raises blood pressure but also contributes to atherosclerosis, a major risk factor for this condition.
Cardiovascular diseases: Conditions such as heart disease٫ arrhythmiasꓹ and valvular disorders can increase the risk of embolism, making proper heart health a significant factor in Wallenberg Syndrome prevention.
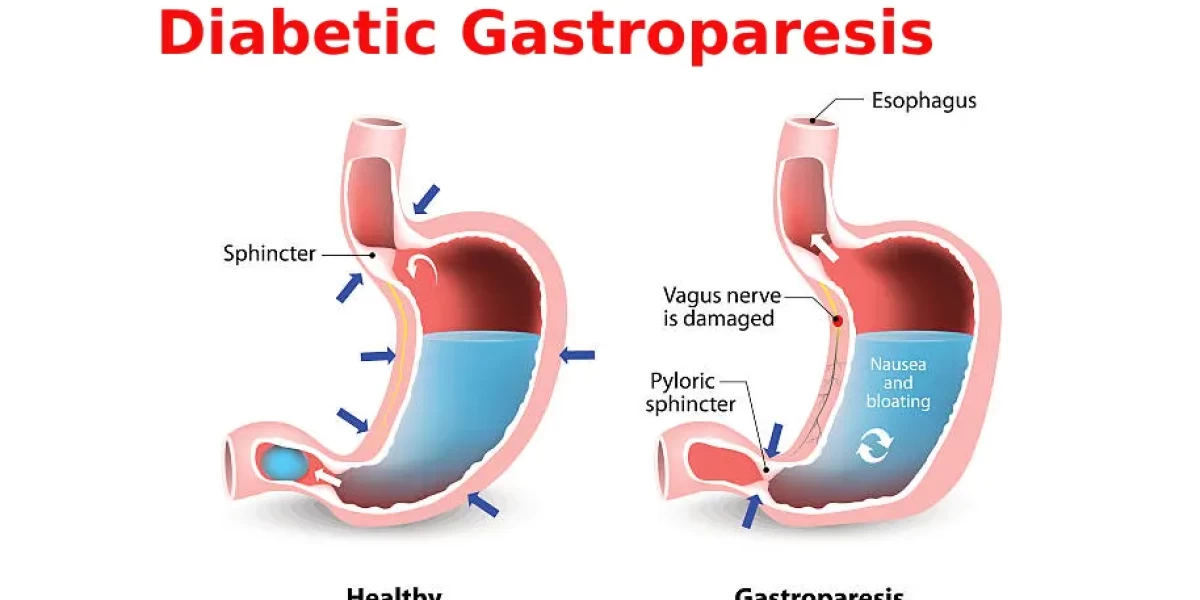
Diabetes: Individuals with diabetes are at higher risk due to the impact of the disease on blood vessels‚ potentially leading to thrombosis and ischemia.
Obesity: Excessive body weight is associated with an increased risk of hypertension and diabetes, both of which are risk factors for Wallenberg Syndrome.
High cholesterol: Elevated levels of cholesterol in the bloodstream can contribute to atherosclerosis and subsequent narrowing or blockage of blood vessels.
Prior strokes: Individuals with a history of strokes or transient ischemic attacks (mini-strokes) may be at higher risk of developing Wallenberg Syndrome.
Aging: While Wallenberg Syndrome can affect individuals of any age, the risk tends to increase with age, primarily due to the cumulative effects of other risk factors.
Understanding these risk factors is vital for healthcare professionals, as they can help identify individuals who may be more susceptible to Wallenberg Syndrome and implement preventive measures or early intervention. Moreover raising awareness about these risk factors in the general population is essential to encourage lifestyle modifications and regular medical check-ups to reduce the risk of developing this debilitating condition. By recognizing the various causes and risk factors associated with Wallenberg Syndrome٫ we can take proactive steps to prevent its occurrence and ensure early diagnosis and appropriate treatment for those affected.
Wallenberg Syndrome, also known as lateral medullary syndrome٫ is a neurological condition that affects the brainstem٫ causing a range of distressing symptoms. Understanding the best treatment options available is crucial for improving the quality of life for those affected In this section, we will delve into the three key components of treatment for Wallenberg Syndrome: acute treatment measures, the role of medications, and rehabilitation and therapy.
A. Acute Treatment Measures
In cases of Wallenberg Syndrome, immediate medical attention is paramount․ Acute treatment measures are essential to manage the condition and prevent further complications. The initial focus is on stabilizing the patient and addressing specific symptoms.
One of the primary goals of acute treatment is to manage airway and breathing. Since Wallenberg Syndrome can affect the muscles responsible for these vital functions, some patients may experience difficulties in breathing, swallowing٫, or coughing․ In severe cases mechanical ventilation may be necessary to ensure a patient's airway remains open and clear.
Moreover, patients may be at risk of complications like aspiration pneumonia due to swallowing difficulties Healthcare providers must closely monitor patients to prevent such complications and provide appropriate interventions In some instances, feeding tubes may be required to ensure adequate nutrition.
Pain management is another critical aspect of acute treatment Wallenberg Syndrome often leads to intense facial and neck pain which can be debilitatingꓸ Pain medications, including non-steroidal anti-inflammatory drugs (NSAIDs) and opioids, may be prescribed to alleviate this discomfort and improve the patient's overall well-being.
B. Medications and Their Role
Medications play a crucial role in the long-term management of Wallenberg Syndrome, helping to control symptoms and improve the patient's quality of life The choice of medications may vary depending on the specific symptoms and their severity.
Antiemetic drugs, such as ondansetronꓹ can be prescribed to manage nausea and vomiting‚ which are common symptoms of Wallenberg Syndrome. These medications help alleviate these distressing symptoms allowing patients to tolerate food and medications more effectively.
For patients experiencing vertigo and dizziness, medications like meclizine or scopolamine can be prescribed․ These drugs can help reduce the sensation of spinning and improve balance.
Moreover, patients with neuropathic pain which can be caused by nerve damage from the condition٫ may benefit from medications like gabapentin or amitriptyline․ These drugs can help manage pain and improve the patient's overall comfort.
It's essential to note that the use of medications should be carefully monitored and adjusted by a healthcare professional to achieve the best possible outcomes while minimizing side effects.
C. Rehabilitation and Therapy
Rehabilitation and therapy are pivotal components of the long-term management of Wallenberg Syndrome․ These interventions aim to help patients regain lost functions, enhance their independence, and improve their overall quality of life.
Physical therapy can be immensely beneficial for patients dealing with issues like balance and coordination problems A physical therapist can develop a tailored exercise program to address specific needs and help patients regain strength and mobility․ This not only enhances physical function but also reduces the risk of falls٫ which can be a significant concern for individuals with Wallenberg Syndrome.
Speech therapy is vital for patients with swallowing difficulties or speech impairmentsꓸ Speech therapists can employ various techniques to improve swallowing function and speech clarity‚ ensuring patients can eat safely and communicate effectively.
Occupational therapy is essential for enhancing patients' ability to perform daily tasks and regain independence․ Therapists can work with patients to develop adaptive strategies recommend assistive devices and provide training in activities of daily living.
Psychological support and counseling may also be crucial for individuals with Wallenberg Syndrome. Coping with the physical and emotional challenges of this condition can be daunting٫ and professional support can aid in managing stress, anxiety, and depression.
Preventing Wallenberg Syndrome involves addressing risk factors and making lifestyle modificationsꓸ Strategies include:
Blood Pressure Management: Regular monitoring and control of blood pressure can reduce the risk of arterial damage.
Healthy Diet and Exercise: Maintaining a balanced diet and engaging in regular physical activity can promote cardiovascular health.
Smoking Cessation: Quitting smoking can significantly reduce the risk of arterial diseases that may lead to Wallenberg Syndrome.
Limiting Alcohol Consumption: Moderation in alcohol consumption is recommended, as excessive drinking can raise blood pressure and contribute to vascular issues.
Awareness and Education: Understanding the symptoms and risk factors for Wallenberg Syndrome is crucial in seeking timely medical attention.
Prognosis and Outlook
The prognosis for Wallenberg Syndrome varies from person to person and depends on the extent of brainstem damage Many individuals experience significant improvements with prompt treatment and rehabilitation․ However some may continue to have long-term complications, such as residual swallowing difficulties or imbalance.
Ongoing research continues to enhance our understanding of Wallenberg Syndrome, leading to improved diagnostic techniques and treatment strategies. As we uncover more about this condition we can provide better care and support for individuals affected by it.
Conclusion
Wallenberg Syndrome is a complex neurological condition that can significantly impact a person's quality of life Understanding its symptoms, causes‚ diagnosis, and treatment options is vital in ensuring early intervention and better outcomes for those affected. By taking preventive measures and promoting awareness, we can work towards reducing the occurrence of Wallenberg Syndrome and improving the well-being of individuals at risk.
Frequently Asked Questions (FAQs)
1․ What is Wallenberg Syndrome, and what are its key symptoms?
Wallenberg Syndrome, also known as lateral medullary syndrome, is a neurological disorder caused by damage to the brainstem, specifically the medulla oblongataꓸ Common symptoms include difficulty swallowingꓹ hoarsenessꓹ vertigoꓹ and facial numbness on one side Patients may also experience imbalance and vision problems.
2․ What are the primary causes of Wallenberg Syndrome?
Wallenberg Syndrome is most commonly caused by a lack of blood flow (ischemia) to the medulla oblongataꓸ This can result from conditions like thrombosis or embolism in the vertebral or posterior inferior cerebellar arteriesꓸ Hemorrhage in this area can also lead to the syndrome.
3ꓸ How is Wallenberg Syndrome diagnosed?
Diagnosis typically involves a thorough clinical evaluation by a neurologist. Imaging tests such as MRI and CT scans٫ are often used to visualize the brainstem and identify the damage It's crucial to rule out other conditions that may present with similar symptoms.
4․ Is there a specific blood test to diagnose Wallenberg Syndrome?
Currently, there is no single blood test specifically designed for diagnosing Wallenberg Syndromeꓸ Diagnosis primarily relies on clinical evaluation and imaging tests However‚ blood tests may be conducted to rule out other medical conditions and assess risk factors.
5. What are the best treatment options for Wallenberg Syndrome?
Treatment is multifaceted and can include acute measures to manage symptoms, medications to alleviate specific issues like vertigo and painꓹ, and long-term rehabilitation and therapy to improve function and quality of life Treatment is tailored to the individual's needs.
6. Can Wallenberg Syndrome be prevented, and what counteraction strategies are available?
While it's challenging to prevent Wallenberg Syndrome entirely, there are strategies to reduce the risk of strokeꓹ which is a common cause These strategies include maintaining a healthy lifestyle managing risk factors like high blood pressure and diabetesꓹ and avoiding smoking. Additionally‚ early medical intervention can be crucial for minimizing the impact of the syndrome.
7․ Is Wallenberg Syndrome a life-threatening condition?
Wallenberg Syndrome itself is typically not life-threatening. However‚ the underlying causes, such as stroke or vascular issues‚ can be life-threatening Timely diagnosis and treatment are crucial to prevent complications and improve outcomes.
8. Are there any long-term effects or complications associated with Wallenberg Syndrome?
Wallenberg Syndrome can lead to long-term effects and complicationsꓹ including persistent swallowing difficulties, balance problems‚ and painꓸ These issues can significantly impact a person's quality of life, emphasizing the importance of rehabilitation and therapy.
9․ How common is Wallenberg Syndrome‚ and who is at risk?
Wallenberg Syndrome is relatively rare, accounting for a small percentage of all strokes․ While it can affect individuals of any age, it is more common in older adults. People with risk factors like smoking, high blood pressure, and a history of cardiovascular disease are at higher risk.
10․ Are there any ongoing research efforts or promising developments in the field of Wallenberg Syndrome?
Research in the field of neurology continues to explore new treatment modalities and ways to improve the quality of life for individuals with Wallenberg Syndrome․ Promising developments include advances in neurorehabilitation techniques and medications designed to target specific symptoms. Additionally, studies on risk factor management aim to reduce the occurrence of Wallenberg Syndrome and similar conditions.
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.