Introduction
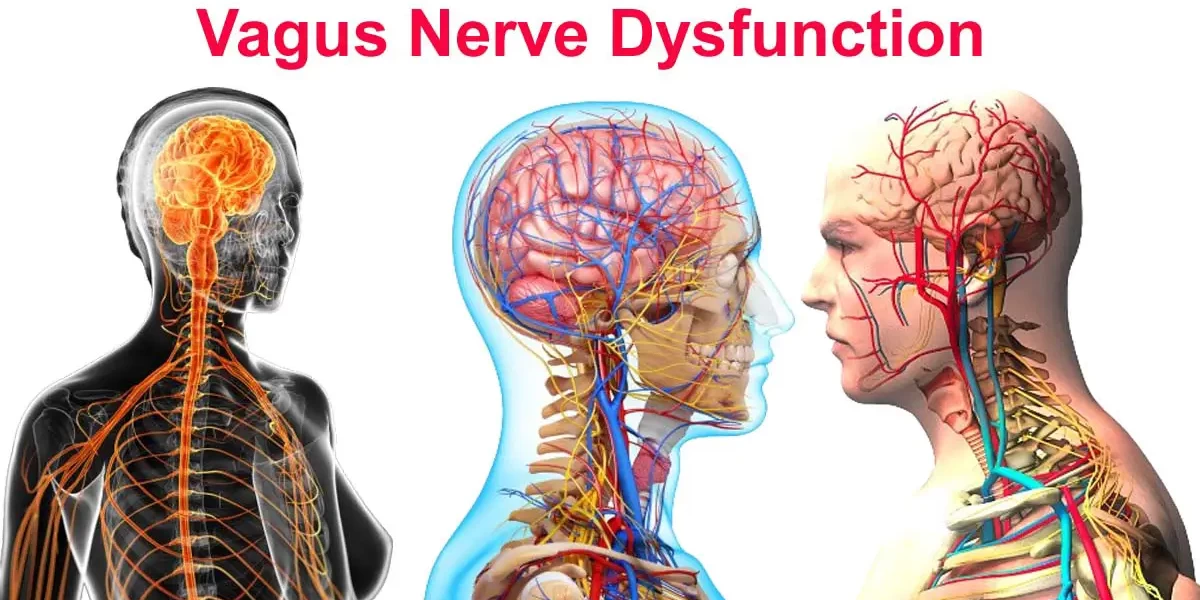
The vagus nerve, often called the body's "superhighway," plays a critical role in our overall health, regulating essential body functions and keeping our systems balanced. From controlling inflammation to supporting mood, this nerve is a central player in physical and mental wellness. Yet, despite its vital role, the vagus nerve often remains overlooked in mainstream health discussions. By gaining insight into this critical nerve and its wide-ranging influence, we can better understand how to manage stress, improve immune function, and optimize health. This article explores the vagus nerve's importance, function, and its relationship with the parasympathetic nervous system. Vagus Nerve Dysfunction
The vagus nerve is pivotal for physical and emotional health, acting as a bridge between the brain and most of our body's organs. It plays a crucial role in calming the body after stress, reducing inflammation, and supporting healthy digestion. Research reveals that a well-functioning vagus nerve can lower anxiety, depression, and even chronic diseases by promoting a "rest and digest" state rather than a "fight or flight" response. By stimulating the vagus nerve, we can tap into better digestion, mood regulation, and even heart rate control, enhancing the quality of our daily lives. Thus, understanding and improving vagus nerve function is paramount to achieving overall well-being. Vagus Nerve Dysfunction
Vagus nerve dysfunction can manifest as a host of physical and psychological issues, such as digestive disorders, anxiety, depression, and chronic inflammation. When the nerve is unable to send accurate signals to organs and tissues, the body cannot appropriately enter a restful state or fight disease effectively. This dysfunction can contribute to common health issues like irritable bowel syndrome (IBS), autoimmune conditions, and mood imbalances. By recognizing symptoms and causes of vagus nerve dysfunction, we empower ourselves to address them with targeted interventions like deep breathing exercises, cold therapy, and mindfulness practices, offering profound benefits to physical and mental health.
What Is the Vagus Nerve?
The vagus nerve is the longest cranial nerve, extending from the brainstem through the neck and chest to the abdomen. As part of the autonomic nervous system, it helps regulate heart rate, digestion, and respiratory rate, among many other functions. "Vagus" means "wandering" in Latin, which accurately describes its far-reaching connections throughout the body. This nerve forms an essential component of the parasympathetic nervous system, responsible for promoting rest, recovery, and balanced body functions. It acts like a communication network, sending signals between the brain and various organs to maintain homeostasis.
- An Overview of the Vagus Nerve:
- Originating in the medulla oblongata of the brainstem, the vagus nerve branches out to touch nearly every major organ in the body. It forms intricate networks with organs in the digestive, respiratory, and cardiovascular systems. This extensive reach makes it critical for sending sensory information to the brain, controlling involuntary processes like heart rate and breathing patterns. When the vagus nerve works optimally, it fosters an internal environment that encourages healing, efficient energy usage, and emotional resilience. However, when impaired, its effects can cascade across multiple systems, leaving health vulnerable.
- Functions of the Vagus Nerve in the Body:
- The vagus nerve’s core functions include slowing the heart rate, facilitating digestion, and modulating immune responses. By releasing acetylcholine, it reduces inflammation, playing a significant role in the immune system's function. It also controls the release of digestive enzymes, ensuring nutrient absorption and gastrointestinal motility. Beyond its physical duties, the vagus nerve contributes to emotional regulation, social connection, and stress reduction by influencing neurotransmitters like serotonin and dopamine. Optimal vagus nerve function is linked to better stress adaptation, clearer thinking, and improved heart health. Vagus Nerve Dysfunction
- Connection Between the Vagus Nerve and the Parasympathetic Nervous System:
- As a key component of the parasympathetic nervous system, the vagus nerve facilitates the "rest and digest" response, counteracting the sympathetic "fight or flight" state. When activated, the parasympathetic system promotes relaxation, energy conservation, and physiological recovery. The vagus nerve triggers a calming response throughout the body, lowering heart rate, relaxing muscles, and enhancing digestion. Techniques that stimulate vagal tone, such as deep diaphragmatic breathing and meditation, help maintain this balance, enhancing resilience against stressors. Strengthening vagus nerve function allows us to shift easily from stress to relaxation, fostering both physical healing and mental clarity.

What Causes Vagus Nerve Dysfunction?
Vagus nerve dysfunction arises when this critical nerve cannot effectively transmit signals between the brain and organs. This dysfunction disrupts the body's ability to regulate essential functions like heart rate, digestion, and immune response. While a range of factors can impair the vagus nerve, understanding the causes is crucial for prevention and treatment. Causes of vagus nerve dysfunction include infections, chronic inflammation, physical trauma, and lifestyle-related stressors. Addressing these underlying triggers and taking steps to strengthen vagal tone can reduce dysfunction, improve overall health, and enhance the body’s natural healing capacity.
Common Causes of Vagus Nerve Dysfunction
Vagus nerve dysfunction can be triggered by multiple factors, each contributing to impaired nerve signaling. Chronic infections, like viral or bacterial infections, can inflame the nerve and surrounding tissues, causing dysfunction. Physical trauma to the neck, head, or spine can compress or damage the nerve, leading to disrupted communication. Chronic stress and anxiety also over-activate the sympathetic nervous system, reducing vagal tone and affecting overall health. Neurological disorders, such as multiple sclerosis and Parkinson's disease, can further impair vagus nerve function, exacerbating symptoms and complicating treatment options. Identifying and addressing these root causes is essential for effective management.
- Infections and Inflammation:
- Infections and inflammation are major contributors to vagus nerve dysfunction. Chronic or acute infections, such as Lyme disease, Epstein-Barr virus, or respiratory illnesses, can inflame and damage the nerve, leading to a wide range of symptoms. Inflammatory conditions, such as autoimmune diseases, trigger the immune system to overreact, leading to chronic inflammation that affects vagal activity. The vagus nerve plays a key role in modulating the body's inflammatory response, but when impaired, inflammation can spiral out of control, causing systemic symptoms like fatigue, brain fog, and digestive issues. Treating infections and reducing inflammation is critical for restoring vagal function.
- Physical Trauma or Injury:
- Physical trauma to the head, neck, or spine can lead to vagus nerve dysfunction by directly injuring or compressing the nerve. Whiplash injuries, concussions, and neck surgeries may all contribute to nerve impairment, disrupting its ability to regulate key bodily functions. This type of dysfunction may manifest as heart rate irregularities, digestive disturbances, or chronic pain. Physical rehabilitation, nerve stimulation therapies, and mindfulness-based practices can often help to restore vagal tone following trauma. Protecting the spine and managing recovery after injury are key to preventing long-term nerve damage and dysfunction.
- Chronic Stress and Anxiety:
- Chronic stress and anxiety are powerful disruptors of vagus nerve function. When we experience prolonged stress, the body remains in a heightened state of fight-or-flight, reducing vagal activity and impairing the nerve’s ability to calm the system. This imbalance can lead to persistent inflammation, digestive issues, and mood disorders. Stress reduction techniques, such as deep breathing exercises, meditation, and cold exposure therapy, can help activate the vagus nerve and bring the body back to a state of balance. Cultivating relaxation and stress management habits is vital for supporting healthy vagal tone. Vagus Nerve Dysfunction
- Neurological Disorders:
- Neurological conditions such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis often involve vagus nerve dysfunction. These conditions can impact the nervous system’s ability to communicate with the body, causing a cascade of symptoms, from impaired digestion to mood disorders. Because the vagus nerve helps regulate neurotransmitter production, its dysfunction may also contribute to cognitive symptoms, such as brain fog and memory impairment. While these disorders present complex challenges, stimulating vagal activity through targeted therapies, nutrition, and exercise may improve quality of life and reduce symptom severity.
Risk Factors Associated with Vagus Nerve Dysfunction
Several risk factors can increase susceptibility to vagus nerve dysfunction. These include genetic predispositions, chronic inflammation, autoimmune disorders, and lifestyle habits such as poor diet, physical inactivity, and high stress levels. Advanced age, chronic illness, and exposure to toxins also elevate the risk of nerve impairment. Recognizing and minimizing these risks is key to maintaining a healthy vagus nerve. Lifestyle interventions, including a balanced diet, stress management, and regular exercise, can lower inflammation and strengthen the vagus nerve’s ability to regulate essential body functions.
What Are the Symptoms of Vagus Nerve Dysfunction?
Vagus nerve dysfunction presents a broad spectrum of symptoms, affecting both the body and the mind. Physical symptoms include digestive disturbances, heart rate irregularities, and chronic pain or fatigue, while neurological and psychological symptoms can manifest as anxiety, depression, or cognitive impairment. Because the vagus nerve touches so many systems, its dysfunction can mimic other conditions, making diagnosis challenging. Understanding the diverse symptoms of vagus nerve dysfunction empowers individuals to seek appropriate care and address root causes, ultimately improving their overall health.
Physical Symptoms
Physical symptoms of vagus nerve dysfunction can vary widely but often include heart rate irregularities, digestive problems, and chronic pain or fatigue. The nerve’s role in regulating the cardiovascular system means dysfunction may present as tachycardia or arrhythmias. Similarly, its influence on digestive processes often leads to conditions like bloating, nausea, or difficulty swallowing. Chronic fatigue syndrome and pain disorders like fibromyalgia may also be linked to impaired vagal activity. Strengthening the vagus nerve through lifestyle changes, therapy, and stress management can help alleviate these physical symptoms.
- Digestive Issues (Gastroparesis, IBS):
- The vagus nerve plays a central role in digestive function, controlling peristalsis, gastric emptying, and the secretion of digestive enzymes. Dysfunction can lead to gastroparesis, where the stomach fails to empty properly, causing nausea, bloating, and abdominal pain. Irritable bowel syndrome (IBS) is another common manifestation, characterized by alternating diarrhea and constipation. By stimulating vagal activity with dietary adjustments, exercise, and stress reduction techniques, individuals may see significant improvement in digestive health.
- Heart Rate Irregularities:
- Vagus nerve dysfunction can cause irregularities in heart rate, ranging from tachycardia (fast heartbeat) to bradycardia (slow heartbeat). Because the nerve plays a key role in regulating cardiovascular function, impaired activity can lead to symptoms like palpitations, dizziness, or fainting. Techniques such as vagus nerve stimulation and biofeedback can be effective tools for restoring balance and stabilizing heart rhythms.
- Fatigue and Chronic Pain:
- Chronic fatigue and widespread pain are often linked to impaired vagus nerve function. By modulating inflammation and pain perception, the vagus nerve helps maintain energy levels and reduce chronic pain conditions like fibromyalgia. When the nerve becomes dysfunctional, it can lead to persistent fatigue, muscle pain, and other inflammatory symptoms. Interventions like vagus nerve stimulation therapy, anti-inflammatory diets, and stress reduction strategies may offer relief and restore vitality.
Neurological and Psychological Symptoms
The vagus nerve's influence on neurotransmitter production and regulation directly impacts mental health and cognitive function. Dysfunction can contribute to anxiety, depression, and mood disorders due to imbalances in serotonin, dopamine, and cortisol. Neurological symptoms may also include brain fog, memory impairment, and difficulty concentrating. By strengthening vagal tone through practices like meditation, breathing exercises, and nutritional support, it is possible to enhance emotional well-being and cognitive clarity.
- Anxiety, Depression, and Mood Disorders:
- Vagus nerve dysfunction often correlates with mental health issues such as anxiety, depression, and mood swings. This is due to its regulation of key neurotransmitters like serotonin and its role in reducing inflammation and cortisol levels. Therapeutic approaches to stimulate the vagus nerve, including mindfulness practices, exercise, and even vagus nerve stimulation devices, may reduce symptoms and improve mental health outcomes.
- Brain Fog and Memory Issues:
- Brain fog and memory issues are common symptoms of vagus nerve dysfunction. The nerve's influence on blood flow and neurotransmitter balance can directly impact cognitive processes, leading to forgetfulness, confusion, or difficulty concentrating. Targeting vagal tone through brain-boosting nutrition, stress reduction, and neuroplasticity exercises can sharpen mental clarity and alleviate cognitive issues associated with nerve dysfunction.
Is There a Test for Vagus Nerve Dysfunction?
Testing for vagus nerve dysfunction involves evaluating the nerve’s ability to communicate with various body systems, providing crucial insight into its health and functioning. While no single definitive test for vagus nerve dysfunction exists, healthcare professionals use a combination of diagnostic tools to assess its role in health conditions. This multi-faceted approach may include heart rate variability (HRV) testing, electrodiagnostic studies, and physical assessments of nerve function. Identifying and diagnosing vagus nerve issues is essential for developing effective treatment plans that address root causes, improve symptoms, and restore vagal tone for optimal wellness. Vagus Nerve Dysfunction
Diagnostic Tools and Methods
Diagnosing vagus nerve dysfunction requires a careful review of symptoms, medical history, and targeted testing. Physicians often perform comprehensive evaluations that include assessing heart rate variability (HRV), a measure of autonomic nervous system function and vagal activity. Electrodiagnostic studies, such as electromyography (EMG) and nerve conduction tests, can also help pinpoint nerve dysfunction by evaluating electrical activity and signal transmission. In some cases, imaging tests like MRI or CT scans may be used to rule out structural issues affecting the nerve. This multifaceted approach ensures a thorough understanding of vagus nerve health, guiding effective treatment strategies.
- Heart Rate Variability (HRV) Testing:
- Heart rate variability (HRV) testing is one of the most common methods for assessing vagus nerve function. HRV measures the variation in time intervals between heartbeats, reflecting the balance between the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous systems. A high HRV generally indicates a well-functioning vagus nerve and strong adaptability to stress, while a low HRV may signal impaired vagal activity and autonomic imbalance. HRV testing is non-invasive and can be performed using specialized devices, making it a useful tool for monitoring vagal health and guiding therapeutic interventions to improve autonomic function.
- Electrodiagnostic Studies:
- Electrodiagnostic studies, including electromyography (EMG) and nerve conduction tests, help evaluate the electrical activity of the vagus nerve and its ability to transmit signals. By placing electrodes on the skin and stimulating the nerve, these tests measure how well signals travel along the nerve pathways. Impaired signal transmission may indicate nerve damage, dysfunction, or other issues affecting the vagus nerve’s communication with the brain and organs. Electrodiagnostic studies are particularly useful for diagnosing conditions like neuropathy and other disorders involving nerve impairment, providing valuable insight into the extent of dysfunction.
When to Seek Professional Help
If you experience persistent symptoms such as digestive issues, chronic fatigue, heart rate irregularities, or mood disturbances, it may be time to seek professional help for potential vagus nerve dysfunction. Early diagnosis is crucial, as untreated vagus nerve issues can lead to worsening health problems. Consulting a healthcare provider familiar with vagal function can provide clarity and guide an effective treatment plan. Professionals may recommend lifestyle modifications, stress management techniques, or specialized therapies to improve vagal tone, reduce symptoms, and support overall health and well-being.
Treatments for Vagus Nerve Dysfunction
Treating vagus nerve dysfunction involves a combination of lifestyle changes, medical interventions, and targeted therapies to restore vagal tone and improve function. Lifestyle approaches, such as stress reduction, exercise, and dietary changes, can strengthen the nerve and promote better health. Medical treatments may include vagus nerve stimulation therapy, medications to address underlying conditions, and, in severe cases, surgical interventions. Each treatment plan is individualized based on the severity of dysfunction, underlying causes, and patient needs, aiming to optimize vagal health and enhance overall well-being. Vagus Nerve Dysfunction
Medical Treatments and Interventions
Medical treatments for vagus nerve dysfunction focus on reducing symptoms and addressing underlying conditions that contribute to nerve impairment. Physicians may prescribe anti-inflammatory medications, antidepressants, or other drugs to target the root causes of vagal dysfunction. Vagus nerve stimulation therapy, a non-invasive treatment, involves using electrical impulses to stimulate the nerve and improve its function. For more severe cases, interventions such as physical therapy, nerve blocks, or specialized neuromodulation techniques may be used. Collaborating with healthcare professionals ensures the most effective approach for improving vagal tone and managing symptoms.
- Vagus Nerve Stimulation Therapy:
- Vagus nerve stimulation (VNS) therapy is a groundbreaking treatment for vagus nerve dysfunction that uses electrical impulses to stimulate the nerve, enhancing its activity and function. This therapy involves implanting a small device near the collarbone that sends regular electrical pulses to the vagus nerve. VNS has been shown to be effective in managing epilepsy, depression, and inflammatory conditions, making it a promising option for patients with vagal dysfunction. Non-invasive options, such as transcutaneous vagus nerve stimulation (tVNS), are also available, offering a convenient way to improve vagal tone and support overall health.
- Medications to Address Underlying Issues:
- Medications can be an essential part of treating vagus nerve dysfunction, particularly when underlying conditions contribute to nerve impairment. Anti-inflammatory drugs, antianxiety medications, and antidepressants can help reduce inflammation, stress, and mood disorders that impact the vagus nerve. In some cases, medications targeting gastrointestinal motility may be prescribed to address digestive issues linked to vagal dysfunction. Collaborating with a healthcare provider to determine the appropriate medication regimen ensures that treatment is tailored to individual needs, promoting better nerve function and symptom relief.
Surgical Options in Severe Cases
For severe cases of vagus nerve dysfunction that do not respond to conservative treatments, surgical interventions may be considered. Vagus nerve stimulation (VNS) implant surgery involves placing a small device under the skin that sends electrical pulses to the nerve, improving its function. In rare situations, other surgical approaches may be used to alleviate nerve compression or repair damage. Surgery is typically reserved for cases where other treatments have failed, offering relief to patients with significant symptoms and limited options. Careful evaluation by a specialist ensures the best outcomes for surgical interventions targeting vagal dysfunction.
Home Remedies for Vagus Nerve Dysfunction
Home remedies for vagus nerve dysfunction offer natural and holistic approaches to improving vagal tone and enhancing overall health. Lifestyle changes, dietary adjustments, and relaxation practices can support vagal function, reducing symptoms and promoting balance in the nervous system. Key home-based strategies include breathing exercises, cold therapy, and consistent physical activity, all of which stimulate the vagus nerve to encourage better communication between the brain and body. These methods empower individuals to take control of their health, alleviating symptoms of dysfunction while supporting the body's natural healing processes.
Lifestyle Changes to Support Vagus Nerve Health
Adopting lifestyle changes is a foundational step in supporting vagus nerve health. Simple modifications, such as prioritizing regular sleep, practicing stress management, and maintaining consistent mealtimes, can significantly enhance vagal function. Building habits like mindful eating, reducing screen time, and practicing gratitude encourages a calm, balanced state, activating the parasympathetic nervous system. Avoiding excessive caffeine, alcohol, and processed foods also helps minimize vagal strain. Making these lifestyle changes not only strengthens vagal tone but also creates a holistic environment where the body can thrive, leading to improved mental clarity, digestion, and emotional resilience.
- Diet and Nutrition Tips:
- Diet and nutrition play a pivotal role in supporting vagus nerve health. Anti-inflammatory foods such as leafy greens, nuts, seeds, berries, and fatty fish rich in omega-3s can reduce systemic inflammation, which supports optimal vagal function. Probiotic-rich foods, like yogurt, kimchi, and sauerkraut, promote gut health and have been shown to enhance communication between the gut and the brain, benefiting the vagus nerve. Avoiding inflammatory foods, such as refined sugars and processed carbohydrates, reduces stress on the nerve. Staying hydrated and consuming a balanced, nutrient-dense diet provides the building blocks necessary for maintaining a healthy nervous system.
- Exercise and Movement Routines:
- Regular exercise and movement can significantly enhance vagus nerve health by increasing blood flow, reducing inflammation, and lowering stress levels. Aerobic exercises, such as walking, jogging, and swimming, have been shown to boost vagal tone by stimulating parasympathetic activity. Yoga and tai chi, which combine movement with mindfulness, are especially beneficial for calming the nervous system and enhancing vagal function. Incorporating strength training, stretching, and moderate-intensity exercises into your routine can support a balanced nervous system, helping to regulate heart rate, improve digestion, and reduce anxiety symptoms associated with vagus nerve dysfunction.
Breathing Exercises and Relaxation Techniques
Breathing exercises and relaxation techniques are effective methods for stimulating the vagus nerve. Diaphragmatic breathing, also known as deep belly breathing, activates the parasympathetic response, reducing heart rate and promoting relaxation. Techniques like alternate nostril breathing, box breathing, and progressive muscle relaxation can further enhance vagal tone, leading to improved stress management and emotional resilience. Meditation, mindfulness practices, and guided imagery are also beneficial for calming the nervous system and enhancing vagus nerve activity. These simple, daily practices offer a powerful way to manage symptoms of dysfunction naturally.
Cold Therapy and Its Benefits
Cold therapy is an effective way to stimulate the vagus nerve and enhance its function. Techniques such as cold showers, ice baths, and splashing cold water on the face activate the nerve’s parasympathetic response, reducing inflammation and promoting a calm state. Research shows that cold exposure can increase vagal tone, lowering stress levels and enhancing resilience to external stressors. Regular use of cold therapy not only improves vagal function but also supports immune health, heart rate variability, and overall well-being. Gradual adaptation to cold exposure allows individuals to safely harness its powerful benefits.
How Effective Are Vagus Nerve Stimulators?
Vagus nerve stimulators (VNS) are devices designed to stimulate the vagus nerve using electrical impulses, offering a treatment option for various conditions linked to vagal dysfunction. VNS is particularly effective in managing epilepsy, depression, and other neurological disorders. By improving vagal tone, stimulators help regulate neurotransmitter release, reduce inflammation, and promote a state of calm. While VNS therapy offers benefits, its effectiveness depends on individual factors and the underlying condition being treated. Many patients report significant improvements in symptoms, highlighting its potential as a therapeutic tool when combined with lifestyle and medical approaches.
Overview of Vagus Nerve Stimulators
Vagus nerve stimulators are devices that deliver electrical impulses to the vagus nerve, typically through a small implant placed near the collarbone. This stimulation can influence autonomic nervous system function, enhancing communication between the brain and the body. VNS devices are used primarily to treat conditions like epilepsy, depression, and anxiety disorders by modulating neural activity. Non-invasive options, such as transcutaneous vagus nerve stimulation (tVNS), are also available, offering accessible ways to stimulate the nerve without surgery. VNS therapy has opened new doors in the treatment of neurological and psychiatric conditions, providing hope for those with chronic symptoms.
Clinical Studies and Success Rates
Clinical studies on vagus nerve stimulation (VNS) therapy reveal promising results in improving health conditions linked to vagal dysfunction. For epilepsy patients, VNS has been shown to reduce seizure frequency by up to 50% in many cases. In individuals with treatment-resistant depression, VNS can lead to significant improvements in mood and a reduction in depressive episodes. Clinical trials also demonstrate its effectiveness in reducing inflammation, anxiety, and heart rate variability issues. However, success rates can vary depending on individual factors and the severity of the condition. Further research continues to explore the full therapeutic potential of VNS therapy.
Potential Risks and Side Effects
While vagus nerve stimulators offer numerous benefits, they come with potential risks and side effects that should be carefully considered. Common side effects of VNS therapy include hoarseness, throat pain, cough, and voice changes due to nerve stimulation. Surgical implantation of VNS devices carries risks such as infection, scarring, and complications from anesthesia. Non-invasive tVNS typically has fewer risks but may cause skin irritation or discomfort at the site of stimulation. Careful monitoring by healthcare professionals and a thorough evaluation of potential risks ensure that patients receive the most appropriate and effective treatment for their condition.
How to Heal the Vagus Nerve Naturally
Healing the vagus nerve naturally centers on practices that enhance vagal tone, which strengthens the connection between the brain and the body. Techniques such as deep breathing exercises, cold exposure therapy, yoga, and singing can stimulate the nerve, improving its function. Regular exercise, proper sleep hygiene, and a diet rich in anti-inflammatory foods also support vagal health. Engaging in social connections, laughter, and meaningful relationships further promotes vagal tone. By incorporating these habits into daily life, individuals can activate the parasympathetic nervous system, reduce inflammation, and restore balance, leading to enhanced physical and emotional well-being.
Daily Habits to Enhance Vagal Tone
Simple daily habits can greatly enhance vagal tone, benefiting both physical and mental health. Deep belly breathing or diaphragmatic breathing helps stimulate the vagus nerve by slowing the heart rate and calming the nervous system. Singing, chanting, or humming can activate the nerve through vocal cord vibration, while regular cold exposure—like splashing cold water on the face or taking cold showers—triggers the nerve’s calming response. Practicing gratitude, maintaining social connections, and consuming a nutrient-rich diet filled with omega-3 fatty acids, probiotics, and antioxidants are also key strategies to naturally enhance vagal function.
The Role of Mindfulness and Meditation
Mindfulness and meditation play a powerful role in healing the vagus nerve by reducing stress, calming the mind, and enhancing vagal tone. Practices such as mindful breathing, guided imagery, and body scanning encourage the body to shift into a relaxed state, activating the parasympathetic nervous system. Meditation has been shown to reduce inflammation, improve heart rate variability, and support emotional resilience. Regular practice can lead to long-term benefits, improving the body's stress response and bolstering vagus nerve health. Even a few minutes of daily mindfulness practice can significantly impact physical, mental, and emotional well-being.
Building Resilience Against Stress
Building resilience against stress is essential for supporting vagus nerve health. Chronic stress weakens the vagus nerve and disrupts the balance between the sympathetic and parasympathetic systems, leading to inflammation, anxiety, and other health issues. To counteract this, focus on stress-reducing activities like deep breathing, yoga, and exercise. Social support, spending time in nature, and practicing positive self-talk also help buffer against stress. Cultivating resilience allows the body to better adapt to life’s challenges, keeping the nervous system balanced and promoting healthy vagal tone for overall well-being.
Conclusion
The vagus nerve plays a critical role in regulating essential bodily functions, including digestion, heart rate, and mood. Healing and enhancing the vagus nerve naturally involves daily practices that promote relaxation, improve vagal tone, and build resilience against stress. By understanding and addressing vagus nerve dysfunction, individuals can improve their quality of life and reduce symptoms related to various health conditions. Investing in habits that nurture the vagus nerve leads to better health outcomes, creating a foundation for lasting wellness.
Vagus nerve dysfunction impacts multiple systems within the body, leading to symptoms ranging from digestive disturbances to anxiety and heart rate irregularities. Key takeaways include recognizing early signs of dysfunction, adopting lifestyle changes to enhance vagal tone, and using therapies that stimulate the nerve. Early detection and management of vagus nerve issues can prevent long-term complications and improve quality of life. Understanding the critical role of the vagus nerve empowers individuals to take proactive steps for better health.
Early detection of vagus nerve dysfunction is crucial for effective management and symptom relief. Identifying early warning signs, such as digestive issues, fatigue, anxiety, or heart rate changes, allows individuals to seek intervention before symptoms worsen. Working with healthcare professionals to develop a personalized treatment plan, which may include natural therapies, medication, or vagus nerve stimulation, ensures the best outcomes. Proactive management of vagal dysfunction is key to maintaining a balanced nervous system and reducing the impact on physical and mental health.
For individuals affected by vagus nerve dysfunction, there is hope and a wide range of options for managing and improving symptoms. From natural approaches like diet, exercise, and stress reduction to advanced therapies such as vagus nerve stimulation, personalized care can make a significant difference. Advances in research continue to shed light on new ways to enhance vagal function, providing patients with a diverse toolbox of strategies. With the right combination of interventions, individuals can reclaim their health and improve their overall quality of life.
Frequently Asked Questions(FAQs)
What are the first signs of vagus nerve dysfunction?
Early signs of vagus nerve dysfunction often include digestive issues like bloating, heartburn, or gastroparesis, along with symptoms such as chronic fatigue, anxiety, difficulty swallowing, or heart rate irregularities.
Can vagus nerve dysfunction be reversed naturally?
Yes, vagus nerve dysfunction can often be improved naturally through lifestyle changes, including deep breathing exercises, meditation, regular physical activity, proper diet, and cold exposure therapy.
How does the vagus nerve impact digestion?
The vagus nerve controls the movement of food through the digestive tract by stimulating muscle contractions (peristalsis). Dysfunction can lead to issues like gastroparesis, bloating, constipation, or irritable bowel syndrome (IBS).
What is the connection between the vagus nerve and mental health?
The vagus nerve influences the production of neurotransmitters that regulate mood, such as serotonin. Dysfunction is linked to anxiety, depression, and other mood disorders, highlighting its critical role in mental health.
Are vagus nerve stimulators covered by insurance?
Coverage for vagus nerve stimulators varies depending on insurance providers and the specific condition being treated. It is often covered for conditions like epilepsy or depression when traditional treatments have failed.
How long does it take to heal the vagus nerve?
The time it takes to heal the vagus nerve varies based on the severity of dysfunction and the interventions used. Lifestyle changes may take weeks to months to improve symptoms, while therapies like VNS may show effects sooner.
Can vagus nerve dysfunction cause chronic pain?
Yes, vagus nerve dysfunction can contribute to chronic pain conditions by affecting inflammation regulation and pain perception pathways, potentially exacerbating issues like fibromyalgia or chronic fatigue syndrome.
How to treat vagus nerve dysfunction?
Treating vagus nerve dysfunction involves a combination of lifestyle changes, therapies, and sometimes medical interventions. Natural approaches include deep breathing exercises, meditation, yoga, and cold exposure therapy, which can enhance vagal tone. Eating an anti-inflammatory diet rich in omega-3 fatty acids and probiotics also supports vagus nerve health. For more severe cases, vagus nerve stimulation (VNS) therapy, medication to treat underlying conditions, or even surgical intervention may be recommended. Working with a healthcare provider to create a personalized treatment plan is often the most effective approach.
How do you know if your vagus nerve is damaged?
Damage to the vagus nerve may manifest through various symptoms, including difficulty swallowing, loss of gag reflex, changes in voice, heart rate irregularities, digestive issues such as bloating or gastroparesis, and frequent fainting spells. Psychological symptoms like anxiety, depression, and brain fog may also indicate vagal dysfunction. Diagnosis typically involves medical history review, physical exams, and diagnostic tests like heart rate variability (HRV) analysis or electrodiagnostic studies. Consulting a doctor for a comprehensive evaluation is crucial to confirm any suspected damage.
What type of doctor treats vagus nerve problems?
Doctors who treat vagus nerve problems include neurologists, who specialize in nervous system disorders, and sometimes gastroenterologists or cardiologists if the symptoms primarily involve digestion or heart function. For complex or chronic cases, a specialist in autonomic disorders or an otolaryngologist (ear, nose, and throat doctor) may be involved. Some patients may benefit from consulting integrative medicine practitioners who use holistic approaches to support vagus nerve health.
Can stress damage the vagus nerve?
Chronic stress can negatively affect the function of the vagus nerve by impairing its ability to regulate the parasympathetic (rest-and-digest) response, which can lead to imbalances in heart rate, digestion, and emotional regulation. While stress may not cause direct physical damage to the nerve, it can weaken vagal tone and exacerbate dysfunction, increasing inflammation and making it harder for the body to recover from stress. Managing stress through relaxation techniques, mindfulness, and other interventions is important for protecting vagal health.
Can the vagus nerve repair itself?
The vagus nerve can often repair itself over time, particularly when supported by lifestyle changes and targeted therapies. Enhancing vagal tone through practices such as deep breathing, meditation, cold exposure, and exercise can promote healing. Consistent stress management and proper nutrition also play key roles in supporting nerve health and regeneration. For severe dysfunction, medical interventions like vagus nerve stimulation therapy may be necessary to aid recovery and improve function.
How to stop anxiety nerve pain?
To stop anxiety-related nerve pain, it’s essential to address both the physical and emotional components. Practicing deep breathing and progressive muscle relaxation can calm the nervous system and reduce pain signals. Mindfulness meditation and yoga can help reduce stress and anxiety, improving overall nerve function. Physical activity and a balanced diet rich in omega-3 fatty acids can also have a positive impact. For persistent pain, consulting a healthcare provider for additional therapies, medications, or counseling to manage anxiety may be beneficial.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.