1. Introduction
Blood sugar, also known as blood glucose, is an essential element that our body relies on for energy. It is derived from the foods we eat and is carried through the bloodstream to be used for energy or stored for future use. Maintaining the proper blood sugar level is crucial because it directly affects our overall health and bodily functions. When blood sugar levels are too high or too low, it can lead to severe health issues.
Hyperglycemia and hypoglycemia are two primary conditions related to blood sugar imbalances. High blood sugar levels are termed hyperglycemia, while low blood sugar levels are called hypoglycemia. Both conditions can be dangerous if not managed properly. Understanding these imbalances is vital for maintaining overall health, preventing potential complications, and ensuring that the body's processes run smoothly. Awareness and education about blood sugar imbalances are key to preventing long-term health issues and improving quality of life. Hyperglycemia vs. Hypoglycemia
2. Defining Hyperglycemia and Hypoglycemia
What Is Hyperglycemia?
Hyperglycemia, a condition characterized by elevated blood sugar levels, occurs when there is too much glucose circulating in the bloodstream. This can happen for several reasons, such as insufficient insulin production, insulin resistance, or dietary factors that lead to excessive carbohydrate intake. Hyperglycemia is a hallmark of diabetes and may lead to serious complications if left unmanaged. Symptoms of hyperglycemia can include frequent urination, increased thirst, blurred vision, fatigue, and headaches. Prolonged high blood sugar levels can damage organs and tissues over time, leading to kidney disease, nerve damage, cardiovascular problems, and eye complications. Effective management of hyperglycemia typically involves careful monitoring of blood glucose levels, adhering to a balanced diet, regular exercise, and medication or insulin therapy when needed.
What Is Hypoglycemia?
Hypoglycemia, on the other hand, is a condition where blood sugar levels drop too low, typically below 70 mg/dL (3.9 mmol/L). This can occur in people with diabetes who take too much insulin or certain medications, skip meals, or engage in strenuous exercise without adequate food intake. Symptoms of hypoglycemia can range from mild to severe and may include shakiness, dizziness, sweating, confusion, irritability, blurred vision, and even loss of consciousness if left untreated. Immediate treatment, such as consuming quick sources of glucose like fruit juice, candy, or glucose tablets, is necessary to raise blood sugar levels quickly. Chronic or severe hypoglycemia requires medical attention to determine underlying causes and to adjust treatment plans accordingly. Hyperglycemia vs. Hypoglycemia

Key Differences Between Hyperglycemia and Hypoglycemia
While hyperglycemia and hypoglycemia both relate to abnormal blood sugar levels, they present opposite issues and demand different interventions. Hyperglycemia is marked by high blood sugar and requires interventions to lower glucose levels, whereas hypoglycemia signifies low blood sugar and calls for quick elevation of glucose. The symptoms and potential complications also vary, with hyperglycemia causing long-term damage if left unmanaged and hypoglycemia posing immediate, sometimes life-threatening risks. Understanding these differences is crucial for individuals managing diabetes and for healthcare providers to ensure proper treatment strategies are employed. Hyperglycemia vs. Hypoglycemia
3. The Role of Glucose and Insulin
How Glucose Fuels the Body
Glucose serves as the primary energy source for the body's cells and is especially vital for the brain's function. When we eat carbohydrates, they are converted into glucose, which is subsequently absorbed into the blood. Cells utilize this glucose for energy to perform various functions, including muscle contractions, brain activity, and cellular repair. In the absence of adequate glucose, the body’s energy reserves deplete quickly, leading to fatigue, dizziness, and impaired cognitive functions. Proper glucose levels are essential for optimal physical and mental performance, as the body constantly works to maintain a balance between intake and expenditure of energy.
The Role of Insulin in Blood Sugar Regulation
Insulin, a hormone secreted by the pancreas, is crucial in managing blood glucose levels. It allows glucose to enter the body's cells to be used as energy or stored as glycogen in the liver and muscles for future use. When we eat and glucose levels rise, the pancreas releases insulin to help move glucose out of the bloodstream and into cells. Without sufficient insulin or if the body becomes resistant to it, glucose remains in the blood, leading to hyperglycemia. Conversely, too much insulin can result in hypoglycemia as blood sugar levels drop too low. The balance between insulin production and utilization is crucial for metabolic health and overall well-being. Hyperglycemia vs. Hypoglycemia
Imbalances in Glucose and Insulin Levels
An imbalance between glucose and insulin can lead to significant health issues. If the body produces too little insulin or the cells become resistant to it, hyperglycemia can develop, increasing the risk of diabetes and related complications. On the flip side, excessive insulin can cause hypoglycemia, depriving the body’s cells of necessary energy. Effective blood sugar management hinges on understanding and addressing these imbalances. This may involve lifestyle changes, dietary adjustments, physical activity, and, in some cases, medication to ensure optimal glucose and insulin balance for sustained health and prevention of complications.
4. Hyperglycemia: Causes and Risk Factors
Primary Causes of Hyperglycemia
Hyperglycemia, characterized by elevated blood sugar levels, arises when the body struggles to produce or effectively use insulin. For those with diabetes, the primary causes include inadequate insulin production, insulin resistance, or the omission of diabetes medications. In type 1 diabetes, the autoimmune destruction of insulin-producing beta cells leads to insulin deficiency. Conversely, in type 2 diabetes, insulin resistance—a state where cells fail to respond properly to insulin—prevails. Factors such as consuming high-carbohydrate meals, prolonged stress, infections, or corticosteroid medications can also exacerbate hyperglycemia by promoting glucose release into the bloodstream or reducing insulin effectiveness.
Common Risk Factors for Hyperglycemia
Several lifestyle and health factors increase the risk of hyperglycemia. These include obesity, sedentary behavior, poor dietary choices, chronic stress, and inadequate diabetes management. Stress triggers the release of hormones such as cortisol and adrenaline, which raise blood sugar. Sleep disturbances, such as insomnia or sleep apnea, also worsen insulin resistance and elevate glucose levels. Genetics play a role too—individuals with a family history of diabetes have a higher predisposition. Moreover, certain medications, including steroids and some diuretics, can interfere with glucose metabolism, raising the risk of hyperglycemia. Hyperglycemia vs. Hypoglycemia
Hyperglycemia in Diabetics vs. Non-Diabetics
Hyperglycemia commonly affects diabetics, resulting from insufficient insulin management, dietary indiscretions, or skipped medication doses. However, non-diabetics can also experience hyperglycemia due to acute illness, chronic stress, or medication side effects. Non-diabetic hyperglycemia often reflects underlying insulin resistance and may signal prediabetes or metabolic syndrome, necessitating lifestyle interventions. Diabetics face more severe consequences of hyperglycemia, including potential diabetic ketoacidosis (DKA) in type 1 diabetes or hyperosmolar hyperglycemic state (HHS) in type 2, which can become life-threatening if untreated. Hyperglycemia vs. Hypoglycemia
5. Hypoglycemia: Causes and Risk Factors
Primary Causes of Hypoglycemia
Hypoglycemia is characterized by blood sugar levels dropping below the normal threshold. Among diabetics, the most common causes are excessive doses of insulin or other glucose-lowering medications, skipped meals, prolonged physical activity, or excessive alcohol consumption without adequate food intake. In non-diabetics, hypoglycemia may stem from conditions such as adrenal insufficiency, severe infections, liver disease, or excessive alcohol intake. Certain medications, including beta-blockers and quinine, can also induce low blood sugar levels.
Common Risk Factors for Hypoglycemia
The risk of hypoglycemia increases due to various factors. For diabetics, frequent changes in daily routines, inconsistent meal timing, and unmonitored physical activities pose significant risks. Overmedication with insulin or sulfonylureas, combined with skipped meals, heightens vulnerability. Non-diabetic hypoglycemia is more common among people with gastrointestinal disorders, hormonal imbalances, or excessive alcohol consumption. Additionally, weight loss surgery can sometimes cause a condition called reactive hypoglycemia, characterized by blood sugar dips following meals. Hyperglycemia vs. Hypoglycemia
Hypoglycemia in Diabetics vs. Non-Diabetics
Hypoglycemia in diabetics often results from overmanagement of glucose control. Insulin-dependent diabetics, especially, are susceptible due to incorrect dosing or meal-planning challenges. Non-diabetic hypoglycemia may arise without a clear cause but often signals hormonal imbalances, critical illness, or reactive drops following meals. Unlike diabetic hypoglycemia, which demands constant vigilance to maintain blood sugar balance, non-diabetic hypoglycemia may require targeted evaluation to identify its cause and prevent recurrent episodes.

6. Symptoms of Hyperglycemia
Early Signs of High Blood Sugar
The initial signs of hyperglycemia often include excessive thirst (polydipsia), frequent urination (polyuria), blurred vision, and fatigue. These symptoms occur because excess glucose in the blood pulls water from body tissues, leading to dehydration and increased thirst. Blurred vision stems from glucose-related changes in the eye's shape, while fatigue results from the body's inability to efficiently use glucose for energy.
Progressive Symptoms of Hyperglycemia
If untreated, hyperglycemia can progress, leading to additional symptoms like headaches, difficulty concentrating, weight loss, and persistent infections such as urinary tract or yeast infections. Prolonged high blood sugar weakens the immune system, making it harder for the body to fight infections. This state also often exacerbates fatigue, disrupts sleep, and heightens hunger (polyphagia) as cells struggle for energy despite high blood glucose levels. Hyperglycemia vs. Hypoglycemia
Severe Symptoms and When to Seek Help
Severe hyperglycemia may present with symptoms like nausea, vomiting, shortness of breath, rapid heartbeat, and confusion. In diabetics, this can lead to emergencies like diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS). Immediate medical attention is vital if blood sugar levels exceed 240 mg/dL despite treatment or if symptoms worsen. Timely intervention prevents complications, such as nerve damage, cardiovascular events, or coma, highlighting the importance of effective glucose management.
7. Symptoms of Hypoglycemia
Early Signs of Low Blood Sugar
Hypoglycemia, or low blood sugar, can present early signs that are critical to recognize for timely intervention. Common symptoms include sudden hunger, shakiness, and sweating, often accompanied by a rapid heartbeat. Feeling anxious or irritable is another common response as glucose levels drop, signaling the body’s need for an energy boost. Other indications include dizziness, lightheadedness, or difficulty focusing on tasks. Recognizing these symptoms early allows individuals to consume a small snack rich in carbohydrates to stabilize blood sugar levels before symptoms worsen. This preventive approach can mitigate more serious health repercussions.
Progressive Symptoms of Hypoglycemia
If early signs of hypoglycemia are not promptly addressed, symptoms can become progressively worse. Individuals may experience confusion, slurred speech, and difficulty walking or maintaining balance. Fatigue and extreme lethargy can take over, making even simple tasks challenging. Some people might experience headaches or blurred vision as glucose levels continue to drop, impairing their mental and physical faculties. As symptoms escalate, it becomes more challenging to self-correct, emphasizing the importance of addressing mild symptoms quickly to prevent more serious outcomes. Hyperglycemia vs. Hypoglycemia
Severe Symptoms and When to Seek Help
Severe hypoglycemia is a medical emergency that can have life-threatening consequences. Symptoms may include loss of consciousness, seizures, or an inability to eat or drink. In such cases, immediate medical intervention is essential to prevent permanent damage. Family members or bystanders should know how to administer glucagon or contact emergency services for assistance. People who frequently experience severe episodes should work closely with a healthcare provider to manage blood sugar levels effectively, minimizing the risk of recurrence. Hyperglycemia vs. Hypoglycemia
8. Long-Term Health Risks
Long-Term Risks of Untreated Hyperglycemia
Chronic untreated hyperglycemia can lead to serious health complications, such as cardiovascular disease, nerve damage, and kidney problems. Over time, elevated blood sugar levels cause persistent inflammation and damage to blood vessels and organs. This can result in diabetic neuropathy, impairing sensation in the limbs, and nephropathy, potentially leading to kidney failure. The heart and eyes are also vulnerable, increasing the risk of heart attacks, strokes, and diabetic retinopathy. Managing blood sugar levels through lifestyle and medication is crucial for reducing long-term health risks.
Long-Term Risks of Untreated Hypoglycemia
Untreated hypoglycemia poses its own unique set of risks, especially when episodes occur frequently. Chronic low blood sugar can lead to cognitive impairment, including memory problems and difficulties concentrating. The brain depends heavily on glucose for energy, so frequent dips can cause long-term damage. Over time, untreated hypoglycemia may also increase the risk of cardiovascular events due to the stress it places on the body. It’s essential for individuals with recurring low blood sugar to work closely with a healthcare provider to identify underlying causes and establish preventive measures. Hyperglycemia vs. Hypoglycemia
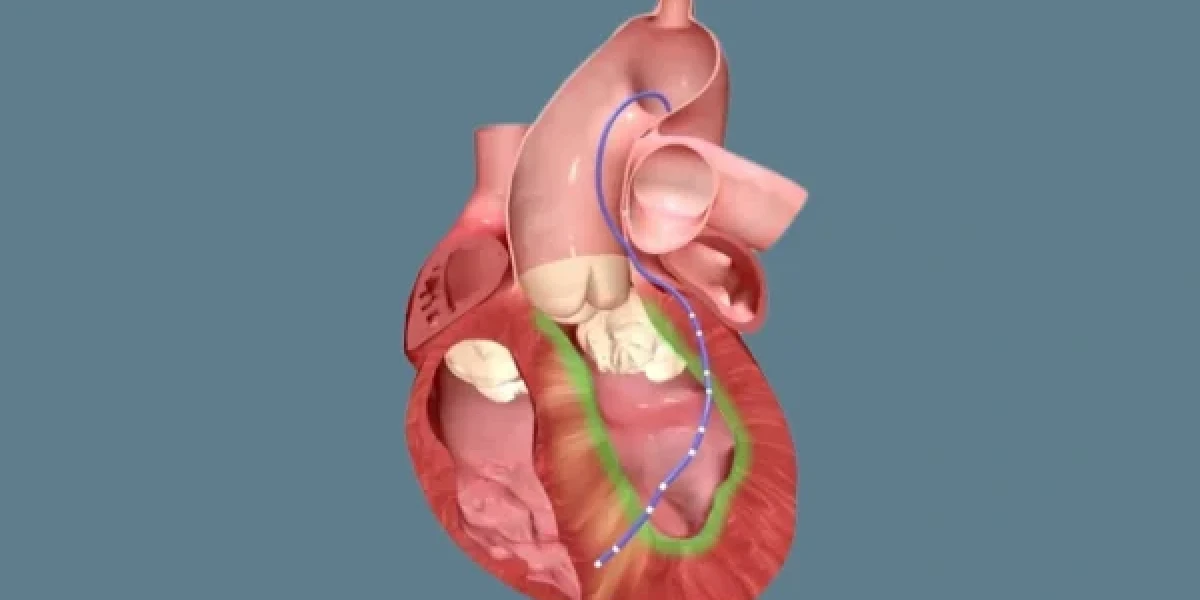
Potential Complications of Recurrent Episodes
Recurrent episodes of hypoglycemia or hyperglycemia significantly heighten the risk of complications. Persistent fluctuations in blood sugar levels can strain cardiovascular health, potentially leading to arrhythmias, heart attacks, or strokes. For people with diabetes, recurrent hypoglycemia may lead to a phenomenon known as "hypoglycemia unawareness," making it harder to recognize symptoms until blood sugar drops to dangerous levels. Preventive strategies, including monitoring blood sugar, managing medications, and maintaining a consistent eating schedule, are vital for reducing these risks.
9. Diagnosis of Blood Sugar Imbalances
Blood Sugar Testing Methods
Several methods are available for testing blood sugar levels, including fasting blood sugar tests, oral glucose tolerance tests, and continuous glucose monitors (CGMs). Fasting blood sugar tests measure glucose levels after an overnight fast, providing baseline data for assessment. Oral glucose tolerance tests evaluate the body's response to a glucose load, often used for diagnosing diabetes. CGMs continuously monitor glucose throughout the day, providing real-time data and trends. Effective blood sugar management starts with accurate testing, allowing for precise interventions.
Interpreting Results for Hyperglycemia
Interpreting test results for hyperglycemia involves understanding thresholds for high blood sugar. A fasting blood sugar level above 126 mg/dL or a random blood sugar reading above 200 mg/dL typically indicates diabetes. Higher levels can suggest poorly controlled diabetes or other health concerns. Consistently elevated readings require lifestyle changes and, often, medical intervention to reduce the risk of complications. Tracking blood sugar fluctuations over time is key to tailoring an effective treatment plan.
Interpreting Results for Hypoglycemia
Hypoglycemia is diagnosed when blood sugar levels drop below 70 mg/dL, though individual thresholds may vary. Symptoms like shakiness, confusion, or fatigue often accompany low readings. Identifying patterns in blood sugar changes can help uncover potential causes, such as medication dosing errors, poor dietary intake, or physical activity imbalances. Addressing these causes and educating patients on recognizing early signs is essential for minimizing health risks associated with low blood sugar levels.
10. Treatment Options for Hyperglycemia
Lifestyle Modifications and Diet
One of the most effective ways to manage hyperglycemia is through lifestyle changes, particularly diet and exercise. A diet rich in whole grains, lean proteins, fruits, and vegetables, while limiting simple sugars and processed foods, can help stabilize blood sugar levels. Portion control and regular meal timing are equally crucial. Physical activity also plays a major role; even moderate exercise like walking can lower glucose levels and improve insulin sensitivity. Stress reduction techniques, such as yoga or meditation, can also contribute by reducing stress hormones that elevate blood sugar. Combined, these strategies empower individuals to achieve healthier glucose control naturally.
Medications and Insulin Adjustments
When lifestyle modifications alone do not suffice, medications may be necessary. Oral antidiabetic medications, such as metformin, can enhance insulin sensitivity or reduce glucose production. Insulin therapy is critical for those with type 1 diabetes and may be necessary for some with type 2 diabetes as well. Adjusting the type, dosage, or timing of insulin is vital for those facing persistent hyperglycemia. Regular consultations with healthcare providers ensure that medications are optimized to balance glucose levels effectively, reducing the risk of complications.
Emergency Treatments for Severe Cases
Severe hyperglycemia, known as diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), demands immediate medical attention. Emergency treatments include intravenous (IV) fluids to rehydrate and insulin therapy to lower blood glucose quickly. Electrolyte imbalances, such as potassium deficiencies, are corrected as part of comprehensive care. Seeking prompt medical help can prevent organ damage and life-threatening complications. Emergency treatment serves as a wake-up call to reassess diabetes management and prevent recurrence through tighter glucose control and regular follow-ups.
11. Treatment Options for Hypoglycemia
Dietary Adjustments and Timing of Meals
Managing hypoglycemia often starts with dietary changes, including consuming regular, balanced meals to maintain stable glucose levels. Small, frequent meals that combine complex carbohydrates, protein, and healthy fats can prevent rapid drops in blood sugar. Avoiding excessive alcohol intake and consuming snacks before bedtime or during intense exercise can further stabilize glucose levels. Collaborating with a registered dietitian can ensure dietary adjustments are personalized to suit individual needs and health goals.
Glucose Supplements and Medications
Glucose supplements, such as tablets or gels, provide a quick source of sugar to rapidly increase blood glucose levels during mild hypoglycemia. For individuals taking insulin or other diabetes medications, adjusting dosages may help prevent frequent episodes. Glucagon injections, administered by a trained family member or friend, are lifesaving for severe hypoglycemia when the individual is unable to consume food or drink. It’s crucial to work with a healthcare provider to fine-tune medication regimens and minimize risks.
Emergency Treatments for Severe Cases
In cases of severe hypoglycemia that lead to unconsciousness or seizures, immediate intervention is necessary. Administering glucagon injections can rapidly raise blood sugar. Emergency responders may provide intravenous glucose. After emergency stabilization, revisiting the underlying causes, such as medication dosing or meal timing, is essential to prevent future occurrences. Loved ones and caregivers should be trained in emergency protocols to ensure timely response and reduce complications. Hyperglycemia vs. Hypoglycemia
12. Preventing Hyperglycemia
Daily Lifestyle Habits for Prevention
Daily habits are key to preventing hyperglycemia. Regular meal timing and portion control help maintain stable blood sugar. Engaging in at least 150 minutes of moderate physical activity weekly can improve insulin sensitivity. Stress management through mindfulness, breathing exercises, or hobbies can reduce spikes in blood sugar levels. Avoiding tobacco and limiting alcohol also contribute to better glucose control. Simple, consistent habits lay the foundation for long-term health and minimize hyperglycemia episodes.
The Role of Diet and Exercise
Diet and exercise are cornerstones of preventing hyperglycemia. A balanced diet low in processed sugars and high in fiber slows glucose absorption, keeping levels steady. Regular exercise helps muscles utilize glucose for energy, reducing circulating levels. Combining aerobic activity, like walking or cycling, with resistance training maximizes insulin sensitivity. It's crucial to find enjoyable activities and dietary patterns to sustain long-term changes and optimize health outcomes.
Monitoring Blood Sugar Levels
Regular monitoring is essential for preventing hyperglycemia. Blood glucose meters and continuous glucose monitors (CGMs) provide real-time insights into glucose fluctuations, allowing for quick corrections through diet or medications. Keeping a log of readings helps identify patterns and triggers, guiding lifestyle adjustments or treatment changes. Effective monitoring is a proactive approach, empowering individuals to maintain control and minimize the risk of prolonged high blood sugar levels.
13. Preventing Hypoglycemia
Strategies for Balanced Blood Sugar Levels
Consistently balancing blood sugar is crucial for hypoglycemia prevention. Strategies include eating balanced meals with a focus on slow-digesting carbohydrates and protein, avoiding skipping meals, and incorporating frequent snacks if necessary. Adjusting insulin or other diabetes medications in consultation with a healthcare provider helps maintain equilibrium. Regular exercise should be paired with pre- and post-workout snacks to avoid drops. These steps build a solid foundation for long-term blood sugar control.
Recognizing Early Warning Signs
Learning to recognize early signs of hypoglycemia, such as shakiness, sweating, or sudden hunger, allows for immediate intervention. Consuming a quick-acting carbohydrate source can prevent symptoms from worsening. Education is key, ensuring individuals understand their personal thresholds and triggers for low blood sugar. Sharing this knowledge with family members and coworkers ensures a supportive environment, minimizing the risk of severe episodes. Hyperglycemia vs. Hypoglycemia
Tips for Reducing Risk in Diabetics
Reducing hypoglycemia risk in diabetics involves proactive measures such as regularly scheduled meals and routine monitoring. Adjusting insulin or other medications based on activity levels and stressors is essential. Carrying fast-acting carbohydrates at all times provides a safety net. Open communication with healthcare providers enables quick adaptation to changing needs, reducing the likelihood of dangerous lows and fostering more stable blood sugar control. Hyperglycemia vs. Hypoglycemia
14. Dietary Considerations
Foods to Avoid for Hyperglycemia
For individuals managing hyperglycemia, avoiding certain foods is crucial to maintaining stable blood sugar levels. Foods high in refined carbohydrates and sugars, such as white bread, pastries, sugary beverages, and processed snacks, can lead to spikes in blood glucose. These foods have a high glycemic index, causing rapid absorption of glucose into the bloodstream. Saturated and trans fats found in fried foods and fatty cuts of meat should also be minimized, as they contribute to insulin resistance. Instead, focus on nutrient-dense whole foods that stabilize blood sugar, support weight management, and reduce the risk of chronic complications.
Foods to Include for Hypoglycemia
For those managing hypoglycemia, consuming foods that provide a steady release of glucose is key. Incorporating complex carbohydrates, such as whole grains, fruits, and vegetables, ensures sustained energy. Pairing carbs with protein and healthy fats, like nuts or lean meats, slows digestion and prevents rapid drops in blood sugar. Snacks such as Greek yogurt, fruit with nut butter, or whole-grain toast can help maintain stable glucose levels. Quick-acting carbs, such as glucose tablets or juice, can be used in cases of acute hypoglycemia to quickly raise blood sugar.
Creating a Balanced Diet for Stable Blood Sugar
Creating a balanced diet for stable blood sugar revolves around the consumption of whole foods, mindful carbohydrate intake, and portion control. Meals should include a balance of protein, healthy fats, and complex carbohydrates to prevent glucose spikes and crashes. Eating at regular intervals and avoiding large gaps between meals helps stabilize blood sugar. Fiber-rich foods, such as legumes, leafy greens, and whole grains, can slow glucose absorption. Staying hydrated and limiting alcohol intake further supports blood sugar management. Personalized nutrition plans can be guided by healthcare professionals to optimize outcomes.
15. Managing Blood Sugar in Daily Life
Monitoring Techniques for Consistent Management
Consistent blood sugar management relies on effective monitoring techniques, such as self-monitoring blood glucose (SMBG) with a glucometer or using a continuous glucose monitor (CGM). SMBG provides snapshots of blood sugar at specific times, while CGMs track levels continuously, offering insights into trends and patterns. Both methods help individuals tailor diet, exercise, and medication for optimal blood sugar control. Maintaining a daily log of glucose readings alongside meals and physical activity offers a comprehensive view of factors influencing blood sugar fluctuations.
Planning Meals and Snacks Effectively
Effective meal and snack planning helps maintain stable blood sugar levels. Individuals should aim for meals balanced in macronutrients and low in refined sugars. Smaller, frequent meals and snacks with a focus on whole grains, lean proteins, and healthy fats can prevent spikes and dips in blood glucose. Pre-planning meals and keeping healthy snacks on hand can minimize reliance on high-sugar options during hunger pangs. Tools like carb counting and understanding the glycemic index can further aid in making informed choices.
When to Seek Help from a Healthcare Professional
There are times when professional guidance is necessary to manage blood sugar effectively. If blood sugar remains consistently high or low despite lifestyle adjustments, or if symptoms become severe or unmanageable, seeking help from a healthcare professional is critical. Medical experts can offer tailored treatment plans, review medication regimens, and provide nutrition and lifestyle guidance. Regular check-ins ensure adjustments are made as needed to maintain optimal blood sugar levels.
16. Hyperglycemia and Hypoglycemia in Different Populations
Blood Sugar Imbalances in Children
Children can experience blood sugar imbalances due to various factors, including diet, activity levels, and underlying conditions like type 1 diabetes. Symptoms may be less obvious than in adults, making regular monitoring essential. For children with diabetes, maintaining a structured meal and activity schedule can prevent fluctuations. In school settings, communication with teachers and caregivers about blood sugar management is crucial for their safety and well-being.
Blood Sugar Imbalances in the Elderly
The elderly may face unique challenges in managing blood sugar imbalances due to age-related changes in metabolism, medication interactions, and comorbidities. Regular monitoring, medication adjustments, and tailored dietary plans can help maintain stable glucose levels. Cognitive impairment and physical limitations may also complicate management, making support from caregivers or healthcare professionals important.
Managing Blood Sugar During Pregnancy
Managing blood sugar during pregnancy is critical for both maternal and fetal health. Gestational diabetes, characterized by high blood sugar levels, requires dietary adjustments, regular exercise, and sometimes medication to ensure stable glucose levels. Women with preexisting diabetes need to work closely with healthcare providers to avoid complications. Monitoring blood sugar levels consistently and attending prenatal appointments ensures a healthy pregnancy outcome. Hyperglycemia vs. Hypoglycemia
17. The Impact of Exercise on Blood Sugar Levels
Exercise Recommendations for Hyperglycemia
Exercise plays a vital role in managing hyperglycemia by enhancing insulin sensitivity and lowering blood sugar. Aerobic activities like walking, swimming, or cycling can help reduce glucose levels. Strength training exercises also improve glucose uptake in muscle cells. It's important to monitor blood sugar before, during, and after exercise, as excessive drops may require adjustments in food intake or medications.
Exercise Recommendations for Hypoglycemia
For individuals prone to hypoglycemia, planning is crucial before engaging in physical activity. Light to moderate-intensity exercise, paired with carbohydrate-rich snacks, can help maintain stable blood sugar levels. It is essential to carry quick-acting carbs, such as glucose tablets, to treat potential low blood sugar episodes during exercise. Consultation with a healthcare provider can help design an exercise routine that minimizes risk.
Safety Tips for Exercise and Blood Sugar Management
Staying safe while exercising involves consistent monitoring of blood sugar levels and listening to the body’s cues. Hydration is key, as dehydration can affect glucose levels. Proper footwear and gradual increases in exercise intensity reduce the risk of injury. Individuals taking insulin or diabetes medications should be aware of exercise-induced hypoglycemia and have a management plan in place. Regular communication with healthcare providers ensures a balanced approach to fitness and blood sugar stability.
18. The Role of Stress in Blood Sugar Fluctuations
How Stress Can Trigger Hyperglycemia
Stress activates the body's "fight-or-flight" response, causing a cascade of hormonal changes, including the release of cortisol and adrenaline. These hormones trigger the liver to release stored glucose into the bloodstream, leading to elevated blood sugar levels, a condition known as hyperglycemia. Chronic stress can exacerbate this effect, increasing insulin resistance over time and making it harder for cells to absorb glucose. For people with diabetes, stress-induced hyperglycemia can complicate blood sugar management, emphasizing the need for stress reduction strategies like mindfulness, physical activity, and adequate sleep.
How Stress Can Lead to Hypoglycemia
In contrast, stress can also lead to hypoglycemia, particularly for people who are on medications such as insulin or sulfonylureas. The stress response can cause erratic eating habits, skipped meals, or excessive physical exertion, which may result in low blood sugar levels. Additionally, stress-related behaviors like consuming alcohol or caffeine can further destabilize blood sugar control. Recognizing these risks is vital for individuals managing blood sugar levels, as effective stress management, balanced nutrition, and consistent monitoring can prevent sudden drops in glucose. Hyperglycemia vs. Hypoglycemia
Effective Stress Management for Blood Sugar Control
Managing stress effectively is a cornerstone of blood sugar control. Techniques such as meditation, yoga, deep breathing exercises, and regular physical activity can reduce the body's stress response. Developing a consistent sleep routine and maintaining a balanced diet are additional ways to lower stress and stabilize glucose levels. Behavioral therapy or stress counseling may also help individuals identify and address their specific stress triggers. Ultimately, a holistic approach to stress management can lead to better overall health and more consistent blood sugar levels. Hyperglycemia vs. Hypoglycemia
19. When to Seek Medical Assistance
Recognizing Emergency Situations
Recognizing emergency situations related to blood sugar fluctuations is critical. Severe hyperglycemia can manifest as extreme thirst, frequent urination, confusion, or even diabetic ketoacidosis (DKA), which requires immediate medical attention. Similarly, severe hypoglycemia symptoms like seizures, unconsciousness, or an inability to speak clearly demand urgent intervention, such as the administration of glucagon or contacting emergency services. Knowing these warning signs can prevent life-threatening complications and ensure timely care.
Regular Check-Ups and Monitoring
Regular check-ups are essential for managing blood sugar levels effectively. Routine visits with healthcare providers help track changes in blood sugar, assess treatment efficacy, and make necessary adjustments to medication or lifestyle. Blood tests, such as HbA1c, provide an overview of average glucose levels over time, helping to gauge long-term control. Consistent monitoring empowers individuals to catch trends early, preventing serious complications and optimizing health outcomes.
Tips for Communicating with Healthcare Providers
Effective communication with healthcare providers is vital for successful blood sugar management. Patients should come prepared with a log of blood sugar readings, medication lists, and questions or concerns. Clearly articulating symptoms, lifestyle changes, and any challenges faced in managing blood sugar can guide healthcare providers in making tailored recommendations. Building a collaborative relationship fosters trust and ensures a personalized approach to diabetes care, enhancing outcomes.
20. Conclusion
Effective management of blood sugar involves understanding the distinct challenges posed by hyperglycemia and hypoglycemia. While hyperglycemia results from excess glucose in the bloodstream, hypoglycemia is characterized by dangerously low levels. Recognizing the symptoms, triggers, and long-term risks of both conditions is crucial for prevention and treatment. Regular monitoring, healthy lifestyle choices, and prompt intervention can significantly improve health outcomes.
Maintaining balanced blood sugar requires a proactive approach. Regular monitoring provides real-time data to adjust diet, medication, and exercise. Healthy eating habits, physical activity, stress reduction, and adherence to prescribed therapies create a solid foundation for long-term health. The key is consistency and awareness, empowering individuals to make informed decisions about their well-being. Hyperglycemia vs. Hypoglycemia
Consulting a healthcare provider is an essential component of effective blood sugar management. Medical professionals can offer expert guidance, adjust treatments, and address concerns. Seeking support fosters a collaborative approach that aligns with individual needs and improves overall quality of life.
21. Frequently Asked Questions(FAQs)
1. What is the normal range for blood sugar levels?
Normal fasting blood sugar levels range from 70 to 99 mg/dL, while post-meal levels should be below 140 mg/dL in non-diabetics.
2. Can someone have both hyperglycemia and hypoglycemia?
Yes, people with diabetes, particularly those using insulin, may experience episodes of both hyperglycemia and hypoglycemia due to fluctuations in diet, activity, and medication.
3. What are the best foods to manage blood sugar levels?
Foods rich in fiber, lean proteins, healthy fats, and low-glycemic carbohydrates like whole grains, vegetables, and legumes help stabilize blood sugar levels.
4. How often should blood sugar be monitored?
Monitoring frequency depends on individual treatment plans. People with diabetes often check daily, but recommendations vary based on condition severity and management goals.
5. What are the immediate steps to take for severe hypoglycemia?
Immediate steps include consuming a fast-acting carbohydrate source, such as glucose tablets or juice. If symptoms persist or worsen, seek emergency medical attention.
6. Is it safe to exercise with hyperglycemia or hypoglycemia?
Exercise has its advantages, yet it should be engaged in cautiously. Individuals should monitor blood sugar before, during, and after exercise to avoid spikes or drops, and consult a healthcare provider for personalized advice.
7. What is the difference between the symptoms of hyperglycemia and hypoglycemia?
Hyperglycemia (high blood sugar) symptoms include frequent urination, increased thirst, blurred vision, fatigue, and headaches. Severe cases may cause nausea, confusion, and even diabetic ketoacidosis in people with diabetes. Hypoglycemia (low blood sugar), on the other hand, often presents with shakiness, sweating, hunger, irritability, confusion, dizziness, and in severe cases, loss of consciousness or seizures. Understanding these contrasting symptoms helps distinguish between high and low blood sugar episodes and take appropriate action.
8. What is hypoglycemia and management?
Hypoglycemia happens when blood glucose levels fall below the normal range, generally under 70 mg/dL. This condition can be caused by factors such as excessive insulin, skipping meals, intense exercise, or alcohol consumption. Management includes consuming fast-acting carbohydrates, like glucose tablets, fruit juice, or candy, to quickly raise blood sugar levels. Long-term management involves identifying triggers, eating balanced meals with complex carbohydrates, and working closely with a healthcare provider to adjust medication or insulin dosages.
9. What are the signs and symptoms of hyperglycemia?
Hyperglycemia manifests with symptoms such as increased thirst, frequent urination, exhaustion, blurred vision, and headaches. As blood sugar levels rise, individuals may also experience difficulty concentrating, dry skin, and slow-healing wounds. In people with diabetes, prolonged hyperglycemia can lead to more serious complications, including ketoacidosis, which manifests with nausea, vomiting, abdominal pain, and a fruity odor on the breath. Quick detection and management are vital to prevent further issues.
10. How do you remember hypoglycemia and hyperglycemia symptoms?
To remember the symptoms of hypoglycemia and hyperglycemia, use the following mnemonics:
- Hypoglycemia: "TIRED" - Tremors, Irritability, Restlessness, Excessive hunger, Dizziness.
- Hyperglycemia: "Hot and Dry, Sugar’s High" - Refers to feeling overheated, having dry skin, and experiencing increased thirst and urination.
11. How do you detect and manage hypoglycemia?
Hypoglycemia can be detected through symptoms like shakiness, sweating, hunger, confusion, and anxiety or by checking blood glucose levels with a glucometer. Immediate management involves consuming 15-20 grams of fast-acting carbohydrates (e.g., glucose tablets or juice). Recheck blood sugar after 15 minutes, and if still low, repeat the process. For severe cases, glucagon injections may be necessary. Preventing hypoglycemia involves consistent meal timing, monitoring blood sugar, and adjusting medications as needed.
12. How to remember hyper and hypo?
To distinguish between hyper and hypo, think of “hyper” as “high” and “hypo” as “low”. Hyperglycemia refers to high blood sugar, while hypoglycemia means low blood sugar.
13. How to remember the difference between hyper and hypo?
Associate hyper with "high" and hypo with "low":
14. How to remember glucose levels?
A common guideline for remembering normal glucose levels is: “70-100 mg/dL” for fasting blood sugar, and less than 140 mg/dL two hours after eating for non-diabetics. Using these benchmarks as a reference can aid in quick recall.
15. How to remember hypokalemia symptoms?
To remember symptoms of hypokalemia (low potassium), use the mnemonic “6 L's”:
- Lethargy
- Leg cramps
- Limp muscles
- Low, shallow respirations
- Lethal cardiac dysrhythmias
- Lots of urine (polyuria)
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.