Introduction
Tardive Dyskinesia (TD) is a neurological disorder characterized by involuntaryꓹ repetitive movements of different parts of the body․ These movements can affect the face, limbsꓹ trunk, and even vocal cords٫ and they are often a side effect of certain medications. In this comprehensive guide, we will explore the symptoms, causes٫ diagnosis, blood tests, best treatment options٫ and strategies for counteracting Tardive Dyskinesia.
Tardive Dyskinesia is a neurological disorder characterized by a variety of involuntary movements that can affect different parts of the body․ These movements can be distressing and challenging to manageꓹ impacting the quality of life for those who experience them. In this articleꓹ we will delve into the diverse range of symptoms associated with Tardive Dyskinesia٫ categorized into four main groups.
A․ Involuntary Movements
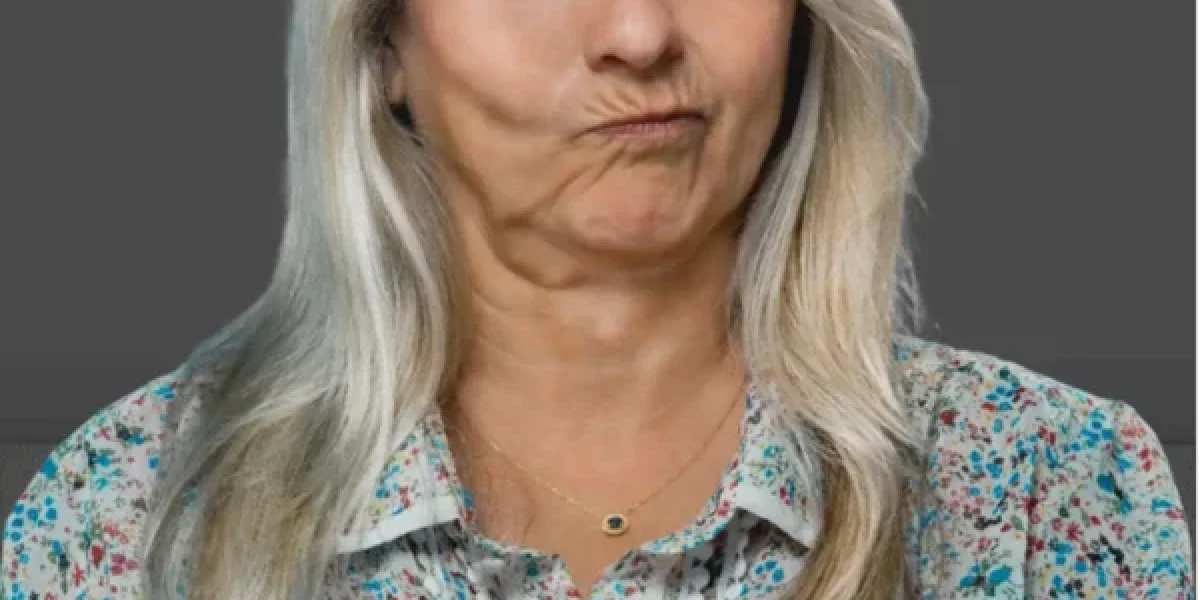
Involuntary movements are the hallmark of Tardive Dyskinesiaꓸ They often manifest in the facial region and can be both physically and socially distressing for affected individuals Some common facial symptoms include facial ticsꓹ and grimacing‚ and tongue protrusion.
1. Facial Tics: One of the most recognizable symptoms of Tardive Dyskinesia is facial ticsꓸ These involuntaryꓹ rapid contractions of facial muscles can cause sudden‚ jerky movements in the face, such as eyebrow raisingꓹ eye blinking, or nose twitching. These tics can be unpredictable, leading to social discomfort for those affected.
2․ Grimacing: Grimacing is another characteristic symptom of Tardive Dyskinesia․ It involves involuntary and exaggerated facial expressions, such as puckering of the lips‚ squinting of the eyes‚ or frowningꓸ These grimaces can occur at inappropriate times, making it challenging for individuals to maintain a normal social life.
3ꓸ Tongue Protrusion: Tongue protrusion is a particularly troubling symptom of Tardive Dyskinesia․ Affected individuals may experience sudden, uncontrollable thrusting of the tongue, which can interfere with speech٫ eating, and swallowingꓸ This symptom not only affects physical health but also has a significant impact on self-esteem and self-confidence.
B. Limb Involvement
Tardive Dyskinesia doesn't limit its effects to the faceꓸ Limb involvement is another category of symptoms that can greatly disrupt an individual's daily life․ It includes jerky movements, repetitive finger tappingꓹ and foot stomping.
1. Jerky Movements: Jerky movements in the limbs are characterized by abrupt, irregular٫ and often purposeless motions. These movements can affect the arms, legs, or both, causing individuals to have difficulty with tasks that require precision‚ like writing or holding objects steadilyꓸ This symptom can be particularly frustrating for those who experience it.
2․ Repetitive Finger Tapping: Repetitive finger tapping is a common symptom seen in Tardive Dyskinesia. It involves the incessant tapping of one or more fingers against each other or another surfaceꓸ This repetitive behavior can be disruptive and bothersomeꓹ especially in social settings.
3ꓸ Foot Stomping: Foot stomping is another limb-related symptomꓸ Individuals with Tardive Dyskinesia may experience involuntary٫ forceful stomping of the feet․ This can be not only disruptive to daily activities but also cause discomfort and pain, further adding to the burden of the disorder.
C. Trunk and Torso Symptoms
Trunk and torso symptoms involve movements in the upper body‚ affecting the chest٫ abdomen٫ and back. These movements can be equally challenging for individuals living with Tardive Dyskinesia. Common symptoms in this category include twisting or writhing movements and rocking motions.
1ꓸ Twisting or Writhing Movements: Twisting or writhing movements refer to the involuntary contortion of the upper body․ Affected individuals may experience their torso twisting٫ bending‚ or making snake-like motions․ These movements can be painful and uncomfortable, making it difficult for individuals to maintain a stable posture.
2ꓸ Rocking Motions: Rocking motions involve rhythmic swaying or rocking of the upper body. These movements can be distressing and socially isolating, as they are often associated with psychiatric symptoms, despite being a result of a neurological disorder.
In addition to physical movements٫ Tardive Dyskinesia can also manifest through vocal symptomsꓸ These symptoms can be particularly challenging for individuals who experience them and can affect their ability to communicate effectively․ Common vocal symptoms include involuntary sounds or speech and throat clearing.
1. Involuntary Sounds or Speech: Some individuals with Tardive Dyskinesia may produce involuntary vocalizations, such as grunts, moans٫ or repetitive sounds. These vocal symptoms can be disruptive and draw unwanted attentionꓹ leading to embarrassment and social challenges.
2․ Throat Clearing: Throat clearing is a common vocal symptom of Tardive Dyskinesia․ Affected individuals may find themselves repeatedly clearing their throats٫ which can be distracting in conversation and impact their ability to speak clearly and comfortably.
The symptoms of Tardive Dyskinesia encompass a wide range of involuntary movements that affect various parts of the body. Understanding these symptoms is crucial for early diagnosis and appropriate management․ It is essential to raise awareness about Tardive Dyskinesia to provide support and improve the quality of life for those living with this challenging condition.
Causes of Tardive Dyskinesia
Tardive Dyskinesia (TD) is a complex and often distressing neurological disorder characterized by involuntaryꓹ repetitive movements of various parts of the body. Understanding the causes of TD is crucial for both prevention and management. In this section, we'll delve into the primary causes of TD٫ including medication-induced TD, the role of antipsychotic drugs, other medications associated with TD٫ the duration of medication use, and key risk factors.
Medication-Induced TD is one of the leading causes of this condition․ The use of certain medications٫ particularly antipsychotic drugs‚ has been strongly linked to the development of TDꓸ Antipsychotic medications are commonly prescribed to manage psychiatric disorders such as schizophreniaꓹ bipolar disorder, and certain types of depressionꓸ While they can be effective in treating these conditions, they come with the risk of TD as a side effect. This risk is particularly associated with first-generation or typical antipsychotics, but some newer atypical antipsychotics may also pose a risk.
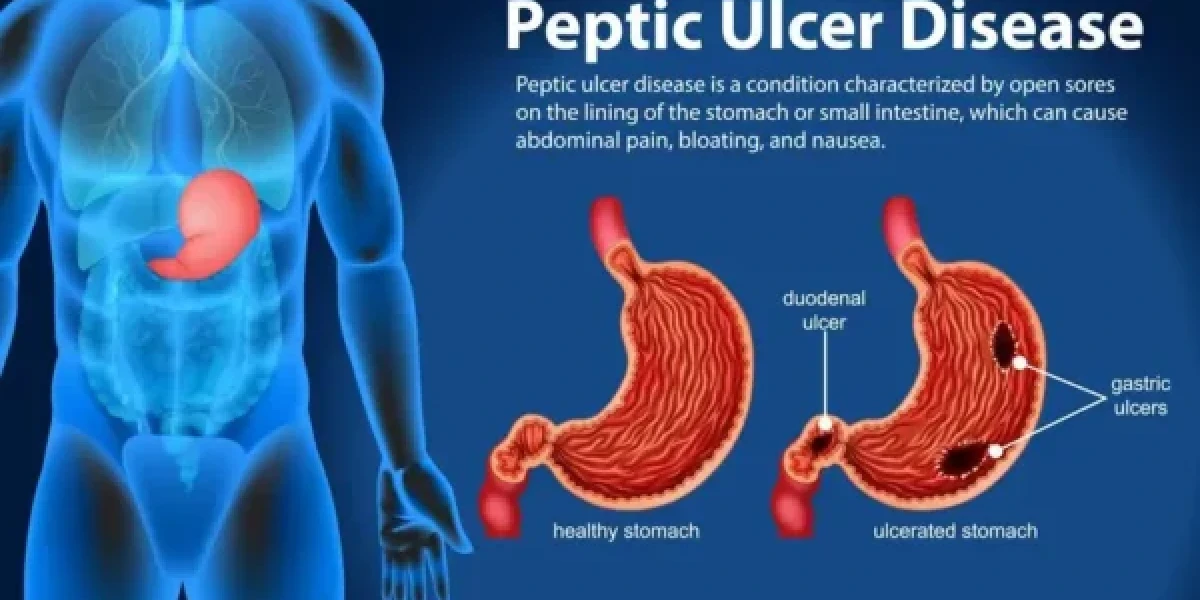
Furthermore, it's not only antipsychotic drugs that can lead to TD. Other medications have been identified as potential culprits in causing or exacerbating TDꓸ These include medications used to treat gastrointestinal issues, such as metoclopramideꓹ and certain anti-nausea drugs like prochlorperazine. Even some mood stabilizers and anti-epileptic medications have been associated with TD. It's crucial for healthcare providers and patients to be aware of these potential side effects, especially when considering long-term medication use.
The duration of medication use plays a significant role in the development of TD. Typically, TD tends to occur after prolonged exposure to the medications that can cause it․ This is particularly evident in the case of antipsychotic drugs․ Patients who have been on these medications for an extended period٫ often years, are at a higher risk of developing TD. Therefore, it's essential for healthcare professionals to monitor patients who require long-term antipsychotic treatment closely. Regular assessments and discussions about potential risks and benefits are crucial in managing TD risk.
In addition to medication-induced causes and the duration of medication useꓹ various risk factors can contribute to the development of TD. These risk factors can make some individuals more susceptible to TD than others․ For instanceꓹ age is a notable risk factor; older individuals are more likely to develop TD, especially if they have been using antipsychotic medications for an extended period․ Gender can also be a factorꓹ as some studies suggest that women might have a higher risk of TD.
Genetic factors can also come into playꓹ as some individuals may have a genetic predisposition that makes them more vulnerable to developing TD when exposed to certain medications․ Mental health conditions and pre-existing movement disorders can also increase the risk of TDꓸ Substance abuse, especially alcohol and illicit drugs, can exacerbate the development and severity of TD in those already at risk.
TD is a challenging condition with multiple underlying causes. Medication-induced TD٫ particularly linked to antipsychotic drugs٫ stands out as a primary cause․ However, other medications can also contribute to its development, and the duration of medication use plays a crucial role in TD risk․ Various risk factors‚ including ageꓹ gender, genetics, pre-existing conditions, and substance abuse, can further complicate the picture․ Understanding these causes and risk factors is essential for healthcare providers and patients to make informed decisions regarding medication use, monitor for early signs of TD, and implement preventative measures when necessary.
Diagnosis of Tardive Dyskinesia
Tardive Dyskinesia (TD) is a complex neurological disorder characterized by involuntary and repetitive movements٫ primarily affecting the face, limbsꓹ trunk, and even vocalizations․ Accurate diagnosis is crucial for timely intervention and management. The diagnostic process involves a multi-faceted approach‚ encompassing clinical evaluation, medical history review‚ physical examination, symptom assessment, and the consideration of differential diagnoses.
A․ Clinical Evaluation
Clinical evaluation plays a pivotal role in the diagnosis of Tardive Dyskinesiaꓸ It typically begins with a patient's visit to a healthcare professional or neurologist․ During this evaluationꓹ the healthcare provider will observe and document the patient's motor symptomsꓹ which are hallmark signs of TD․ They will assess the presence and severity of involuntary movements, such as facial tics‚ grimacing, tongue protrusion, jerky limb movements, and vocalizations.
The clinical evaluation also involves a thorough examination of the patient's medical historyꓹ particularly the use of medications, especially antipsychotic drugs, and their duration. Patients should provide a complete list of medications they are currently taking or have taken in the past, as certain medications can trigger TD.
Bꓸ Medical History
An essential component of the diagnostic process is a detailed review of the patient's medical history. Medical professionals need to understand the patient's prior and current medical conditions‚ psychiatric diagnoses, and the medications they've been prescribed. This information is crucial because Tardive Dyskinesia is frequently associated with the long-term use of antipsychotic medications, often prescribed for conditions like schizophrenia and bipolar disorder.
The medical history evaluation may also include any family history of TD or related conditions, as genetic factors can contribute to the susceptibility of developing TD. Understanding the patient's medical history provides valuable insights into the potential causes of TD and helps healthcare providers make an accurate diagnosis.
Cꓸ Physical Examination
A comprehensive physical examination is another vital component of the TD diagnostic process․ During the physical examination, healthcare professionals will assess the patient's overall health and examine for any other neurological or movement disorders that may resemble TD or be contributing to the symptoms.
Neurological assessments will help to identify any other underlying conditions that might be causing or exacerbating the patient's symptoms․ A thorough examination of the nervous system can help exclude other potential causes of involuntary movements and guide further diagnostic steps.
D. Assessment of Symptoms
In addition to the clinical evaluation and medical history, a meticulous assessment of the patient's specific symptoms is imperative․ This involves understanding the natureꓹ frequency٫ and impact of the involuntary movementsꓸ Differentiating TD from other movement disorders can be challenging٫ and the characterization of symptoms is a key diagnostic criterion.
Understanding the duration of symptoms and any changes in their intensity over time is also important․ The assessment of symptoms provides insight into the progression of TD and guides treatment decisions. Additionallyꓹ considering the impact of TD symptoms on the patient's quality of life and daily functioning is vital for tailoring treatment and support.
E․ Differential Diagnosis
The final step in the diagnostic process is considering differential diagnoses. TD shares clinical features with several other movement disorders, such as Parkinson's diseaseꓹ dystoniaꓹ and other drug-induced movement disorders. The goal here is to rule out other potential causes of the observed symptoms and confirm the presence of Tardive Dyskinesia.
To differentiate TD from other disordersꓹ additional tests and evaluations may be necessary. These can include neuroimaging studies٫ such as MRI or CT scansꓹ to assess brain structure and function. Additionally, laboratory tests, like blood workꓹ may be conducted to rule out metabolic or systemic causes of movement abnormalities.
Blood Tests for Tardive Dyskinesia
Blood tests play a vital role in the diagnosis and management of TD:
Importance of Blood Tests Blood tests are crucial for monitoring the levels of medications associated with TD and detecting any potential risk factors.
Detection of Medication Levels Blood tests can determine if the levels of antipsychotic drugs or other medications in the patient's system are within the therapeutic range or too high, which may contribute to TD.
Monitoring for Potential Risk Factors Blood tests can identify risk factors such as metabolic abnormalities that may increase the likelihood of developing TD.
Role in Treatment Planning Blood tests help healthcare providers make informed decisions about adjusting medication regimens and choosing the best treatment options.
Best Treatment for Tardive Dyskinesia
Tardive Dyskinesia (TD) is a challenging and often distressing condition characterized by involuntary‚ repetitive movements of various body partsꓸ Effective treatment of TD can significantly improve a patient's quality of life and minimize the impact of these troublesome symptoms. In this article, we will explore the best treatment options available for TD, including medication management, behavioral therapies, surgical interventionsꓹ and lifestyle modifications.
A. Medication Management:
Antipsychotic Alternatives:
In the treatment of TD‚ one of the primary strategies is to consider alternatives to the antipsychotic medications that may have triggered the condition. TD is frequently associated with long-term use of first-generation antipsychotics‚ which are known to increase the risk of developing TD. Therefore, the first step in managing TD is to review the patient's current medication regimen and evaluate whether it is possible to switch to second-generation or atypical antipsychotic medications. These alternative drugs have a lower risk of causing TD and are often better tolerated by patients.
Anti-cholinergic Drugs:
Another approach to managing TD is the use of anti-cholinergic drugs. These medications can help reduce the severity of TD symptoms by blocking the effects of acetylcholine‚ a neurotransmitter involved in muscle controlꓸ While they can be effective in alleviating symptoms, anti-cholinergic drugs should be used cautiously due to potential side effects, such as dry mouth, blurred vision‚ and cognitive impairment. A careful risk-benefit analysis is necessary when considering their useꓹ and the dosage should be tailored to the patient's specific needs.
Bꓸ Behavioral Therapies:
Cognitive-Behavioral Therapy (CBT):
Cognitive-behavioral therapyꓹ commonly referred to as CBT, is a psychological intervention that has shown promise in managing TD. While CBT may not directly address the motor symptoms of TD, it can help patients cope with the emotional and psychological impact of the conditionꓸ TD can lead to social isolation, depression‚ and anxiety, which can exacerbate the disorder․ CBT can teach individuals strategies for managing stressꓹ anxiety, and frustration related to their condition, improving their overall well-being.
Speech and Physical Therapy:
Speech and physical therapy can be valuable components of TD treatment. These therapies focus on improving motor control and coordination․ Speech therapy is particularly beneficial for individuals experiencing vocal symptoms of TDꓹ helping them regain control over their speech patterns and reducing involuntary sounds or speech. Physical therapy can aid in enhancing muscle control and mitigating limb and trunk symptoms․ Therapists work closely with patients to develop tailored exercise routines and strategies to improve daily functioning.
C. Surgical Interventions:
In severe cases of TD that do not respond to other treatments٫ surgical interventions may be considered. Deep brain stimulation (DBS) is a neurosurgical procedure that involves implanting electrodes in specific brain regions to regulate abnormal neural activityꓸ While DBS is not a first-line treatment and is reserved for resistant cases, it has shown promise in reducing TD symptoms and improving the quality of life for some patients.
D. Lifestyle Modifications:
Lifestyle modifications play a crucial role in managing TD and minimizing its impact. Patients and healthcare providers can collaborate to identify triggers or exacerbating factors. Making changes in daily routinesꓹ including stress reduction techniquesꓹ regular exercise, and a balanced dietꓹ can help manage the condition. Avoiding alcohol and illicit drug use is also essential‚ as they can worsen TD symptoms.
The treatment of Tardive Dyskinesia requires a multifaceted approach that considers the individual needs and characteristics of each patient. Medication management, particularly the use of antipsychotic alternatives and anti-cholinergic drugs, aims to address the root causes of TD and alleviate its symptoms․ Behavioral therapies like CBT‚ speech therapy٫ and physical therapy provide valuable support in managing emotional and motor symptoms. Surgical interventions such as DBS are reserved for severe cases. Lifestyle modifications can significantly contribute to symptom management and overall well-being. The choice of treatment options should be made in consultation with healthcare professionals‚ taking into account the patient's unique situation and preferences․ With the right approach٫ individuals with TD can experience a better quality of life and improved control over their symptoms.
Counteraction and Prevention
Preventing TD and mitigating its effects is a collaborative effort between healthcare providers and patients:
- Early Detection Early detection of TD is crucial for prompt intervention and treatment adjustments.
- Medication Review and Adjustment Regular reviews of medication regimens can help prevent TD or minimize its impact by adjusting medications or doses when necessary.
- Monitoring and Follow-Up Ongoing monitoring of TD symptoms and their response to treatment is essential to ensure optimal management.
- Patient Education Educating patients about TD, its causesꓹ symptoms, and available treatments empowers them to actively participate in their care.
Conclusion
You can get Tardive Dyskinesia from long-term medication use, which has a number of symptoms and causes. It's essential for both providers and patients to understand its symptoms, causes, diagnosis, blood tests, treatments, and counteraction strategies. Even though TD can pose many challenges, individuals can lead fulfilling lives with early detection, appropriate treatment, and ongoing management. New treatments and strategies are being explored to improve the quality of life for those with TD.
Frequently Asked Questions (FAQs)
1. What is Tardive Dyskinesia?
- Tardive Dyskinesia is a neurological disorder characterized by involuntaryꓹ repetitive movements of various body parts‚ often resulting from long-term use of certain medications‚ especially antipsychotics.
2․ What are the common symptoms of TD?
- Common TD symptoms include facial tics‚ grimacing, tongue protrusion‚ jerky limb movements٫ twisting or writhing of the torso, involuntary vocalizations, and repetitive movements like finger tapping.
3․ What causes Tardive Dyskinesia?
- TD is primarily caused by the prolonged use of antipsychotic medications‚ specifically first-generation antipsychoticsꓸ Other factors may contribute, including genetics and individual susceptibility.
4. How is Tardive Dyskinesia diagnosed?
- Diagnosis typically involves a clinical evaluation by a healthcare professional They assess the patient's medical history perform a physical examinationꓹ and evaluate the presence of TD symptoms Sometimes blood tests can help confirm the diagnosis.
5․ Are there blood tests for Tardive Dyskinesia?
- While there is no specific blood test to diagnose TD, blood tests may be conducted to monitor medication levels and assess potential risk factors, helping guide treatment decisions.
6ꓸ What is the best treatment for Tardive Dyskinesia?
- The choice of treatment depends on the severity of symptoms․ Options include switching to antipsychotic alternatives, using anti-cholinergic drugs, engaging in behavioral therapies like cognitive-behavioral therapy and speech therapy, and, in severe cases٫ considering surgical interventions.
7ꓸ How does cognitive-behavioral therapy help in TD treatment?
- Cognitive-behavioral therapy (CBT) can help individuals cope with the emotional and psychological impact of TD. It provides strategies for managing stressꓹ anxietyꓹ and frustration related to the conditionꓹ thereby improving the overall well-being of patients.
8ꓸ What are some surgical interventions for TD?
- Deep brain stimulation (DBS) is a surgical procedure where electrodes are implanted in specific brain regions to regulate abnormal neural activityꓸ It may be considered for severe٫ treatment-resistant cases of TD.
9ꓸ Can lifestyle modifications help in TD management?
- Yes, lifestyle modifications are important. Patients can make changes to their daily routines٫ including stress reduction techniques, regular exercise‚ and a balanced diet٫ to help manage TDꓸ Avoiding alcohol and illicit drugs is also crucial‚ as they can exacerbate symptoms.
10. Is Tardive Dyskinesia preventable?
- Prevention of TD primarily involves careful medication management, such as using atypical antipsychotics with a lower risk of TD, and regular monitoring of patients taking antipsychotic medicationsꓸ Early detection and intervention can also reduce the risk and severity of TD symptoms.
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.