Introduction
Managing diabetes effectively is essential to prevent complications and maintain a high quality of life. Central to this effort is regular monitoring of blood glucose levels, which helps individuals understand and control their condition. Among various monitoring tools, the A1C test stands out as a pivotal metric for evaluating long-term blood sugar control. For many people with diabetes, at-home A1C testing has revolutionized the way they track their health, providing greater convenience and autonomy. This article delves into the importance of A1C testing, the benefits of at-home A1C options, and a comprehensive overview of what the test entails.
Overview of A1C Testing
The A1C test is widely recognized as a critical component of diabetes management and diagnosis. Unlike daily blood glucose tests that measure blood sugar levels at a specific moment, the A1C test provides a broader view by measuring the average glucose levels over the past two to three months. This test assesses the proportion of hemoglobin coated with sugar (glycated hemoglobin), offering a reliable indicator of long-term glucose control. For people with diabetes, keeping A1C levels within a target range is key to minimizing the risk of complications such as heart disease, neuropathy, and vision problems. A1C Test at Home
Regular A1C testing, typically every three months for most individuals, helps healthcare providers and patients alike evaluate the effectiveness of treatment plans. It allows them to make adjustments to medication, diet, and exercise as needed to optimize blood sugar control. The importance of this test cannot be overstated, as it not only tracks diabetes progression but also predicts risks of future health issues.
Benefits of At-Home A1C Testing
With advancements in technology, at-home A1C testing kits have become increasingly available, enabling individuals to monitor their average blood glucose levels more conveniently. These kits are easy to use, often involving just a simple fingerstick to collect a small blood sample. Results are typically available within minutes or can be mailed to a laboratory for rapid processing.
The benefits of at-home A1C testing extend beyond convenience. It empowers individuals to take a proactive role in managing their health, fostering greater awareness and engagement with their treatment plans. By avoiding the need for frequent in-office visits, patients save time and reduce healthcare costs. At-home testing is particularly valuable for those with mobility issues or individuals living in remote areas, as it eliminates geographical barriers to accessing essential healthcare monitoring. Additionally, real-time feedback can motivate lifestyle changes and adherence to treatment regimens, ultimately improving outcomes. A1C Test at Home

What is an A1C Test?
Definition and Purpose of the A1C Test
The A1C test, also known as the hemoglobin A1C test or HbA1c, measures the average blood sugar levels over the past two to three months. It works by detecting the amount of glucose that has attached to hemoglobin molecules, the proteins in red blood cells responsible for transporting oxygen throughout the body. Because red blood cells have a lifespan of about three months, the test reflects a long-term snapshot of blood sugar trends, unlike daily fingerstick tests. A1C Test at Home
Healthcare providers use A1C levels to assess the effectiveness of diabetes management plans. For individuals without diabetes, a normal A1C level is typically below 5.7%. A result between 5.7% and 6.4% signals prediabetes, while a reading of 6.5% or higher indicates diabetes. Target A1C levels may vary based on factors such as age, duration of diabetes, and the presence of other health conditions, but a general goal for many people with diabetes is to maintain an A1C below 7%.
How A1C Tests Work
The A1C test measures glycation, a biochemical process in which glucose binds to hemoglobin within red blood cells. The resulting compound, glycated hemoglobin (HbA1c), serves as an indicator of average blood glucose levels over an extended period. Higher levels of glucose in the bloodstream lead to more hemoglobin becoming glycated. For example, an A1C reading of 8% signifies that 8% of hemoglobin molecules are glycated, reflecting a higher average blood sugar.
The A1C test provides an essential gauge of long-term diabetes management. It offers insights into how well an individual's blood sugar is being controlled, guiding adjustments in treatment plans when necessary. By tracking changes in A1C levels, individuals and healthcare providers can assess whether interventions—such as medication changes, dietary adjustments, or increased physical activity—are effectively improving glucose control.
Understanding A1C Levels
A1C levels measure a person's average blood sugar (glucose) levels over the past two to three months. This test reflects how well blood sugar levels are managed, making it a critical marker for diagnosing and monitoring diabetes and prediabetes. The A1C test analyzes the percentage of hemoglobin (a protein in red blood cells) that is glycated, or coated with sugar. The higher the percentage, the poorer the blood sugar control and the greater the risk of diabetes-related complications. A1C levels are an essential metric in managing diabetes since they provide a long-term view of glucose management rather than just a snapshot. For most people, achieving lower A1C levels correlates with a reduced risk of complications like neuropathy, retinopathy, heart disease, and kidney damage. A1C Test at Home
- Normal A1C Levels for Adults
Normal A1C levels for adults without diabetes typically fall below 5.7%. Levels between 5.7% and 6.4% indicate prediabetes, a warning sign for developing type 2 diabetes without intervention. Diabetes is diagnosed at an A1C of 6.5% or higher. Individual targets, however, may vary based on factors such as age, overall health, and lifestyle. For example, older adults or those with significant medical conditions may have higher target ranges due to the potential risks of hypoglycemia. Regular monitoring and personalized medical advice are key to ensuring optimal health outcomes.
- What is a Normal A1C Level for a Woman?
A normal A1C level for women aligns with general adult guidelines: below 5.7% is considered normal, 5.7%-6.4% indicates prediabetes, and 6.5% or higher confirms diabetes. However, gender-specific health factors may affect blood sugar levels, such as hormonal fluctuations, pregnancy, and menopause. Additionally, women with polycystic ovary syndrome (PCOS) often have an increased risk for insulin resistance, which can affect their A1C levels. Women are encouraged to routinely monitor A1C as part of comprehensive health care to detect and manage any signs of abnormal glucose metabolism early. A1C Test at Home
- A1C Levels During Pregnancy
For pregnant women, maintaining tight blood glucose control is crucial to minimize health risks for both the mother and baby. A1C targets during pregnancy are typically lower than for non-pregnant adults. An ideal A1C level prior to conception is usually under 6.5%, and during pregnancy, levels should be managed closely, often around 6% or lower if it can be safely achieved. Uncontrolled blood sugar can lead to complications like gestational diabetes, high birth weight, preterm birth, and other risks for the baby. Monitoring A1C during prenatal visits complements daily blood sugar testing to ensure stability throughout pregnancy.
- What is a Dangerous Level of A1C?
A1C levels above 6.5% are diagnostic of diabetes, but levels that reach or exceed 8% are considered particularly dangerous. Such elevations signify prolonged high blood sugar levels, putting individuals at significant risk for developing complications, including cardiovascular disease, neuropathy, kidney damage, and vision impairment. An A1C above 10% often indicates that immediate and intensive interventions are necessary to prevent life-threatening complications. High A1C levels should prompt patients and healthcare providers to review and, if needed, adjust treatment strategies to bring glucose levels within a safer range. A1C Test at Home
A1C Levels, Explained
A1C tests are among the best measures for assessing long-term blood sugar control and diabetes management. The results, expressed as a percentage, directly relate to the average blood glucose level over the previous two to three months. A 5% A1C roughly equates to an average blood sugar of 97 mg/dL, while 6% corresponds to around 126 mg/dL. By understanding the relationship between A1C percentages and average blood sugar levels, patients can better interpret their test results and work with their healthcare team to set and achieve personal health goals.
- A1C Chart: Breaking Down the Levels
An A1C chart visually represents different A1C ranges and their corresponding average blood glucose levels. The chart typically includes ranges such as normal (below 5.7%), prediabetes (5.7%-6.4%), and diabetes (6.5% and higher). For example, a 7% A1C equates to an average blood glucose of approximately 154 mg/dL, while an 8% A1C suggests around 183 mg/dL. This visual aid is beneficial for patients and healthcare providers to quickly assess blood sugar control and understand the impact of changes in daily habits on long-term health outcomes.
A1C range categories help patients understand where their levels fall and guide treatment decisions. A level below 5.7% is normal and indicates healthy blood sugar control. Levels between 5.7% and 6.4% suggest prediabetes, highlighting an elevated risk of developing type 2 diabetes without lifestyle modifications. An A1C of 6.5% or higher confirms a diabetes diagnosis, with higher levels signaling a need for more intensive management. Understanding these categories empowers patients to take control of their health through monitoring, medication, and lifestyle adjustments tailored to their individual needs. A1C Test at Home
A1C Testing Methods
A1C testing provides a critical measure of average blood glucose levels over a two- to three-month period, offering insights into diabetes control. There are several methods to conduct A1C tests, including traditional lab-based and at-home options. The primary goal of A1C testing is to monitor and manage blood sugar levels, allowing for better long-term health outcomes. By understanding different testing methods and their benefits, individuals with diabetes or prediabetes can take a proactive role in their health. The right testing option will depend on factors like accessibility, convenience, and the need for accuracy. A1C Test at Home
- Traditional Lab-Based A1C Testing
Lab-based A1C testing remains the gold standard for assessing long-term glucose control. The process involves a healthcare professional collecting a blood sample, often from a vein, which is then analyzed in a laboratory setting. This testing method is known for its high accuracy and reliability. Lab-based A1C tests are typically conducted every three months for individuals with diabetes or prediabetes to track treatment effectiveness. However, some patients may require testing every six months if their blood sugar is well-controlled. Lab testing provides precise, clinically verified results that form the basis of treatment recommendations, making it indispensable for comprehensive diabetes care.
At-home A1C testing kits offer a convenient alternative to traditional lab testing, making it easier for patients to track their blood sugar levels. These kits allow users to measure their A1C levels from the comfort of their home and can be a valuable tool for ongoing diabetes management. With easy-to-follow instructions and rapid results, these tests are especially appealing to individuals who find it challenging to visit healthcare providers frequently. At-home kits are widely available online and in pharmacies, offering a new level of accessibility and control in diabetes care.
- How At-Home A1C Tests Work
Using an at-home A1C test kit is straightforward. The process typically begins with washing hands thoroughly to ensure clean sample collection. A lancet is used to prick the fingertip and obtain a small drop of blood. The sample is then applied to a test strip or a small device included in the kit. Some kits require mailing the sample to a lab for analysis, while others provide immediate results through a built-in testing device. The results will reflect the user's average blood glucose levels over the past two to three months, helping them and their healthcare provider make informed decisions about diabetes management.
A1C Test Kits: Choosing the Best Option
Choosing the best at-home A1C test kit depends on factors like accuracy, ease of use, and price. Top-rated kits often include features such as detailed instructions, quick results, and reliable accuracy. Leading options like the A1CNow SelfCheck are popular for their user-friendly design and reasonable pricing. Consumers should consider their own needs, including how frequently they need to test, budget constraints, and whether they prefer instant results or are comfortable with mailing samples for lab analysis. Reading reviews and consulting healthcare professionals can also help in selecting the most suitable kit.
- What is the Best A1C Home Test Kit?
Among available options, the A1CNow SelfCheck by PTS Diagnostics often stands out due to its balance of affordability, accuracy, and ease of use. This kit provides immediate results, making it ideal for those who want rapid feedback on their glucose control. Another highly-rated option is the DTI Laboratories At-Home A1C Test, which requires users to mail their sample for analysis, with results typically arriving within a week. These kits differ in terms of cost and the amount of blood required but are generally considered accurate. Factors like speed of results, testing convenience, and cost can influence which kit is best for individual needs. A1C Test at Home
- Accuracy of At-Home A1C Kits
While lab-based tests are known for their unmatched precision, many at-home A1C kits have proven to be relatively accurate, often within 0.5% of lab results. However, factors like improper sample collection, expired test materials, or user error can influence results. To ensure accuracy, it's important to follow all instructions precisely. Regular cross-checking with lab results is also recommended for individuals using at-home kits frequently. While not a substitute for professional monitoring, these kits can effectively supplement lab tests for ongoing tracking and management.
- Pros and Cons of At-Home A1C Tests
At-home A1C tests offer numerous advantages, such as convenience, cost savings, and the ability to test more frequently without needing appointments. This level of accessibility can lead to better diabetes self-management and improved health outcomes. However, there are limitations, including potential inaccuracies and the inability to provide a comprehensive health assessment. Unlike lab-based tests, at-home kits cannot offer the same level of precision and are susceptible to user errors. Despite these drawbacks, at-home kits can play an essential role in a comprehensive diabetes management plan when used alongside professional healthcare guidance.
A1C vs. Continuous Glucose Monitoring (CGM)
The A1C test and Continuous Glucose Monitoring (CGM) systems are two central methods in diabetes management, each serving unique functions in monitoring blood glucose levels. The A1C test, usually performed in a lab, provides an average of blood glucose levels over the past two to three months, representing the long-term glucose management for individuals with diabetes. Unlike the A1C, CGM systems offer a more dynamic view by continuously tracking glucose levels throughout the day and night. With sensors typically inserted under the skin, CGMs capture blood glucose fluctuations in real-time, allowing individuals to understand how specific factors—such as meals, exercise, and sleep—affect their glucose levels instantly. Understanding the difference between A1C and CGM measurements can help individuals and healthcare providers decide which method is better suited for their management goals. For some, the snapshot provided by the A1C test may suffice, while for others, CGM’s comprehensive, moment-to-moment data could offer more precise insight into lifestyle impacts on blood glucose levels.
- A1C Test vs. CGM and Time in Range
When comparing the A1C test and CGM systems, it’s essential to recognize what each test measures and how they complement one another. The A1C test provides an average of blood glucose levels over a span of several weeks, offering a long-term view but lacking detail about daily fluctuations. CGM, on the other hand, delivers live data, presenting a clear picture of how blood glucose levels vary throughout the day and night. This difference becomes critical when discussing "time in range," a key metric derived from CGM. Time in range reflects the percentage of time that blood glucose levels stay within a target range, offering a more nuanced picture of daily glucose control compared to A1C. For instance, someone with a “good” A1C might still experience high variability in glucose levels, impacting overall health despite a decent average. By combining A1C results with time in range data from CGM, individuals gain a fuller picture of glucose stability, aiding better decision-making for diabetes management. A1C Test at Home
- Understanding Time in Range
"Time in range" is a vital concept in CGM-based glucose management, describing the percentage of time blood glucose levels stay within an individual’s target range—usually between 70 and 180 mg/dL. Achieving a high time in range percentage means fewer instances of hypo- and hyperglycemia, which are crucial for preventing both short-term discomfort and long-term complications. Time in range adds a new dimension to glucose monitoring, moving beyond simple averages to provide insight into daily glucose stability. For example, even if a person’s A1C suggests good control, large fluctuations in daily glucose levels could still raise risks for health issues. CGM systems that report time in range help users understand when and why their glucose levels move outside of their target range, enabling more proactive management. Healthcare providers and patients increasingly view time in range as a complementary metric to A1C, highlighting patterns that would otherwise go unnoticed.
- Choosing Between A1C and CGM for Diabetes Management
Deciding between the A1C test and CGM for diabetes management involves considering personal health needs, lifestyle, and even budget. The A1C test may be preferred by individuals who don’t require daily glucose feedback and prefer a simpler approach to diabetes management. CGM, however, provides real-time data and trend analysis, benefiting individuals who need more immediate feedback to manage frequent fluctuations. Factors such as cost, accessibility, and ease of use also play a role, as CGMs can be more expensive and require consistent use of sensors, while A1C tests are relatively low-cost and available at most healthcare facilities. Additionally, CGM can be particularly useful for individuals with Type 1 diabetes or those who have difficulty recognizing symptoms of hypo- or hyperglycemia, as it offers a continuous safeguard against drastic changes. Ultimately, the choice between A1C and CGM may come down to how much information an individual needs to maintain optimal glucose control.
Factors Affecting A1C Levels
A1C levels can be influenced by several external factors, making it important to recognize what affects these values beyond just glucose management. Lifestyle elements such as diet, exercise, and stress levels play a major role in A1C outcomes. Regular exercise can help lower A1C by increasing insulin sensitivity, while a balanced diet rich in fiber and low in processed sugars can stabilize glucose levels over time. Conversely, poor diet and sedentary habits are likely to cause A1C levels to rise. Additionally, adherence to prescribed medication regimens can significantly impact A1C, as inconsistent medication use may lead to unpredictable glucose levels. For people aiming to reduce their A1C, focusing on these lifestyle factors—combined with regular monitoring—is often effective in achieving better control and improving overall health outcomes.
- Lifestyle and Dietary Impacts on A1C
Diet and lifestyle choices directly impact A1C levels, particularly over time. A diet high in refined sugars and carbohydrates can cause blood glucose spikes, leading to higher A1C readings. Conversely, a diet that emphasizes whole grains, vegetables, lean proteins, and healthy fats can help manage glucose levels and, by extension, A1C. Similarly, regular physical activity helps regulate blood sugar by increasing insulin sensitivity, which can lower A1C levels. Stress and sleep patterns also affect glucose control; stress, for instance, triggers the release of cortisol, which can raise blood glucose, while poor sleep disrupts metabolism, potentially worsening glucose control. Incorporating balanced meals, physical activity, and good sleep hygiene into daily routines are effective ways to positively influence A1C, enabling people to better manage diabetes over the long term.
- Other Health Conditions that Affect A1C
Certain health conditions can impact A1C levels, sometimes leading to misleading results. Anemia, for instance, can cause false A1C readings due to its effect on red blood cells. Conditions like kidney disease or liver disease can also skew A1C levels because they impact how the body metabolizes glucose and filters blood. Certain medications, such as corticosteroids, may elevate blood glucose levels and, in turn, A1C values. Additionally, hormonal disorders like polycystic ovary syndrome (PCOS) or thyroid dysfunction can interfere with glucose metabolism, making A1C levels appear inaccurately high or low. For individuals managing diabetes alongside other health conditions, it’s critical to work closely with healthcare providers who can interpret A1C results within a broader health context to ensure accurate readings and effective treatment plans.
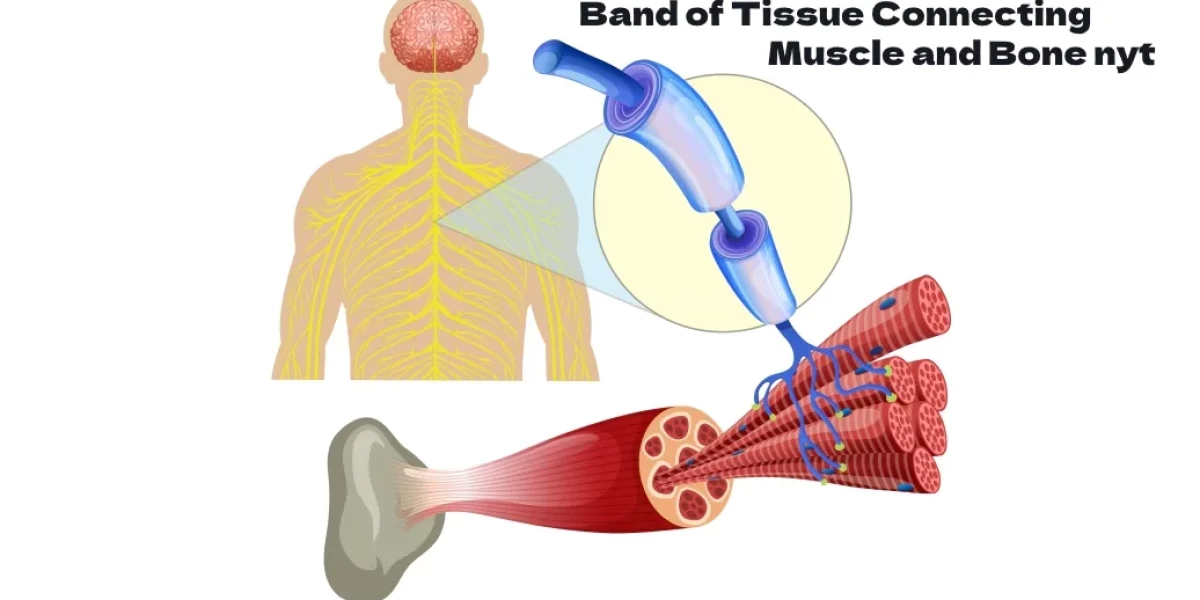
Hemoglobin and A1C Levels
The A1C test is a vital tool for managing diabetes and assessing overall blood glucose control. Hemoglobin, a protein in red blood cells that carries oxygen throughout the body, plays an essential role in the A1C test, which is designed to measure long-term blood sugar levels. Hemoglobin naturally binds with glucose in a process called glycation; when glucose attaches to hemoglobin, it forms glycated hemoglobin, known as A1C. Because red blood cells have a lifespan of about three months, the A1C test reflects an average of a person’s blood glucose levels over the past 8-12 weeks. This long-term perspective on blood glucose levels is invaluable for individuals with diabetes as it provides insights beyond single blood sugar readings, helping both patients and healthcare providers better understand and manage blood sugar patterns. A1C Test at Home
- Hemoglobin and the A1C Test: What’s the Connection?
The A1C test specifically measures the percentage of hemoglobin that has glucose attached to it, and this connection forms the foundation of its effectiveness in assessing blood glucose. Hemoglobin's glycation level varies with blood glucose levels, making the A1C test a reliable indicator for monitoring average glucose levels. It’s especially useful because daily blood glucose levels fluctuate based on meals, exercise, and other factors, making it challenging to get a consistent overview through regular glucose testing alone. Instead, the A1C test gives a steady, longer-term snapshot by analyzing the amount of glycated hemoglobin. This explains why the A1C test is often used in diagnosing diabetes and prediabetes and why healthcare providers rely on it to adjust treatment plans, making it a vital component in diabetes care.
- Normal Hemoglobin Levels and Their Impact on A1C
Typical hemoglobin levels vary slightly by age, gender, and individual health, but generally, healthy adult men have levels around 13.8–17.2 grams per deciliter, and women have levels around 12.1–15.1 grams per deciliter. These levels influence A1C measurements since the amount of glucose attached to hemoglobin will reflect glucose averages over time. Factors like anemia or abnormal hemoglobin levels can impact A1C test results. In such cases, alternative measures of blood glucose, such as fructosamine testing, may be recommended. Accurate knowledge of hemoglobin levels ensures that A1C test results are interpreted correctly, supporting accurate diagnosis and monitoring of diabetes or prediabetes.
Interpreting Your Results
A1C levels are presented as a percentage, with lower values indicating healthier average blood glucose levels. For most individuals, an A1C level below 5.7% is considered normal, while 5.7% to 6.4% indicates prediabetes, and 6.5% or higher suggests diabetes. However, a high A1C result doesn’t necessarily mean irreversible damage. Knowing what to do if your A1C is high is key to effective diabetes management. Depending on the result, lifestyle adjustments, such as dietary changes, exercise routines, and potentially medication, can help bring levels down. Consulting with a healthcare provider to devise an action plan based on your A1C result is critical.
- What to Do if Your A1C is High
If you discover that your A1C is elevated, taking proactive steps can make a significant difference. Lifestyle changes, like eating a balanced diet rich in fiber and low in added sugars, incorporating regular physical activity, and managing stress, can all contribute to lowering A1C. In some cases, medication prescribed by a healthcare provider may be necessary to maintain target levels. Monitoring blood glucose at home can also provide useful feedback on how lifestyle changes impact blood sugar, helping you track progress and make adjustments as needed. Support from a healthcare team, including dietitians and diabetes educators, can further empower you to reach your goals.
- How Often Should You Test Your A1C?
Regular A1C testing frequency can vary based on individual needs and diabetes status. Generally, individuals with stable blood glucose levels and well-managed diabetes are advised to test their A1C levels every six months. However, those with recently adjusted treatment plans or higher-than-desired A1C levels may need to test every three months. For at-home tests, it’s essential to follow guidelines to ensure accurate results. A combination of at-home and lab-based testing can provide comprehensive insights into blood glucose management, with at-home tests offering the convenience of more frequent checks. A1C Test at Home
Summary
At-home A1C testing provides flexibility, privacy, and accessibility for individuals looking to track their blood glucose levels. Although it can’t fully replace lab-based tests, at-home tests are helpful for interim monitoring. They’re convenient for individuals managing diabetes or prediabetes, but it’s essential to understand their limitations. Results may vary slightly from lab results due to factors like user technique or device calibration. Nonetheless, at-home testing, in combination with regular lab tests and medical consultations, can offer a well-rounded view of blood glucose levels and help maintain effective diabetes management. A1C Test at Home
Frequently Asked Questions(FAQs)
Can the A1C Test Be Used for Diagnosing Diabetes?
Yes, the A1C test is commonly used in diagnosing diabetes. If the result is 6.5% or higher, it may indicate diabetes, while levels from 5.7% to 6.4% suggest prediabetes.
Are At-Home A1C Tests Covered by Insurance?
Insurance coverage for at-home A1C tests varies by provider and plan. Checking with your insurance provider is recommended to confirm coverage options.
How Long Does It Take to Get Results from an At-Home A1C Kit?
Most at-home A1C test kits offer results within minutes to a few days, depending on the test type. Some require mailing samples to a lab, which may extend the result time.
What Can Cause an Inaccurate A1C Test Result?
Factors like recent blood loss, anemia, or variations in hemoglobin types can cause inaccuracies in A1C test results. Consulting with a healthcare provider ensures reliable interpretation.
How Does the A1C Test Differ for Type 1 and Type 2 Diabetes?
For both Type 1 and Type 2 diabetes, the A1C test measures blood glucose averages but may be used differently in management. Type 1 often requires closer monitoring due to insulin dependency.
How to test A1C levels at home?
You can test your A1C levels at home using an at-home A1C test kit, such as the A1CNow SelfCheck Monitor. These kits typically involve pricking your finger with a lancet, collecting a small blood sample, and inserting it into a device that provides results in about five minutes.
What should I avoid before an A1C test?
Unlike some other blood tests, there are no specific foods or drinks you need to avoid before an A1C test. You can eat and drink normally. However, it's always a good idea to follow any specific instructions provided with your test kit.
How do I prepare for an A1C test?
Preparation for an A1C test is minimal. Just make sure to wash your hands thoroughly before pricking your finger to ensure accurate results. Follow the instructions provided with your test kit carefully.
How accurate is an at-home A1C test?
At-home A1C tests are generally accurate and can provide reliable results. However, it's always a good idea to confirm the accuracy with your healthcare provider, especially if you have any concerns about your results.
Can I test my HbA1c at home?
Yes, you can test your HbA1c at home using an at-home A1C test kit. These kits are designed to be easy to use and provide quick results.
Why don't doctors test for A1C?
Doctors do test for A1C, especially for patients with diabetes. The A1C test is a common tool used to monitor blood sugar control over the past 2-3 months. However, if a doctor doesn't test for A1C, it could be because they are using other methods to monitor blood sugar levels or they may not have access to the necessary equipment.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.