Introduction
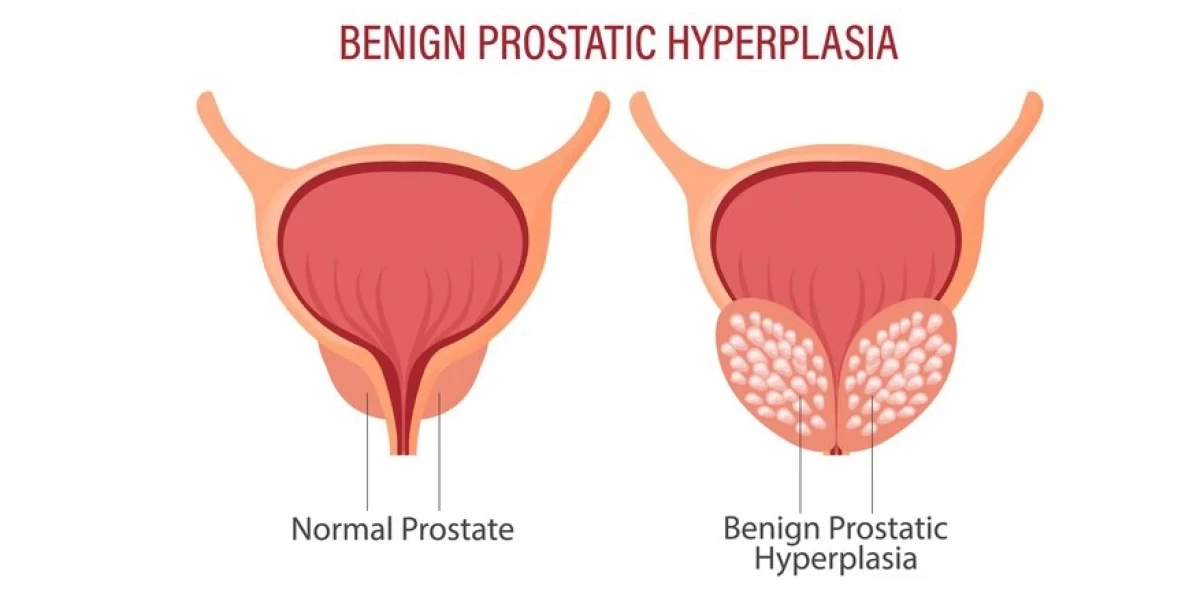
Benign prostatic hyperplasia (BPH) is a common condition affecting men as they age, and it holds significant importance in men's health. Often referred to as an enlarged prostate, BPH is a non-cancerous growth of the prostate gland that can lead to uncomfortable urinary symptoms. As men age, the risk of developing BPH increases, making it a crucial issue in urology and overall well-being. Understanding the prostate gland and its role in the male reproductive system is key to grasping the significance of BPH. In this article, we will explore the function of the prostate, how it changes over time, and what men need to know about BPH and its impact on health.
What Is the Prostate Gland?
The prostate gland is a small, walnut-sized organ situated just beneath the bladder and ahead of the rectum. It surrounds the urethra, the tube responsible for carrying urine from the bladder out of the body. Despite its small size, the prostate plays a vital role in male reproductive health. Its primary function is to produce seminal fluid, which mixes with sperm from the testicles to form semen. This fluid not only nourishes sperm but also aids in its transportation during ejaculation. Without a properly functioning prostate, the reproductive process could be impaired, which emphasizes its importance in sexual health.
As men age, the prostate naturally undergoes changes. Around the age of 40, it starts to grow larger, a process known as prostate enlargement. This growth is normal and is believed to be linked to hormonal changes, particularly involving testosterone and dihydrotestosterone (DHT). However, as the prostate grows, it can begin to press against the urethra, restricting the flow of urine. This pressure can lead to symptoms commonly associated with BPH, such as frequent urination, difficulty starting and stopping urination, weak urine stream, and a feeling of incomplete bladder emptying.
The relevance of these changes to BPH cannot be understated. While prostate enlargement is a natural part of aging, it becomes problematic when it leads to urinary obstruction and discomfort. BPH itself is not life-threatening, but its symptoms can significantly affect a man's quality of life. The condition often requires medical attention to manage symptoms and prevent complications, such as urinary tract infections, bladder stones, or kidney damage.
By understanding the anatomy and function of the prostate gland, as well as the natural changes it undergoes with age, men can better recognize the importance of monitoring their prostate health. Early detection and treatment of BPH can lead to better outcomes and prevent long-term issues related to urinary and sexual health.

What Causes Benign Prostatic Hyperplasia?
Benign Prostatic Hyperplasia (BPH), or an enlarged prostate, is primarily caused by hormonal changes associated with aging. As men age, testosterone levels gradually decline, and the balance between testosterone and estrogen shifts. This hormonal imbalance can lead to the growth of prostate cells, causing the prostate gland to enlarge. The increase in size can press against the urethra, leading to the common urinary symptoms associated with BPH. These age-related hormonal changes are the most common cause of BPH, making it a prevalent condition in older men.
Genetic factors also play a significant role in the development of BPH. Men with a family history of prostate problems are more likely to experience an enlarged prostate themselves. Specific genes that regulate the growth of prostate cells may be passed down through generations, increasing susceptibility to BPH. Additionally, certain genetic predispositions can make the condition develop earlier in life, even in men who might not have other significant risk factors.
Lifestyle influences, such as diet, physical activity, and overall health, can contribute to the onset of BPH. Poor dietary choices, such as a high intake of red meat and fatty foods, can increase the risk of developing an enlarged prostate. Conversely, diets rich in fruits, vegetables, and healthy fats have been linked to a reduced risk. Sedentary lifestyles, obesity, and smoking are also associated with a higher likelihood of BPH. These lifestyle factors, combined with hormonal and genetic influences, create a complex web of causes that lead to the condition.
Benign Prostatic Hyperplasia Prevalence and Risk Factors

BPH is a common condition, especially among older men. Statistics show that around 50% of men aged 50 and older experience symptoms of BPH, and this number rises to about 90% for men in their 80s. The prevalence increases with age, making BPH one of the most common conditions affecting men as they grow older. It’s important to recognize that while BPH is not life-threatening, its symptoms can significantly impact daily life, especially in terms of urinary function.
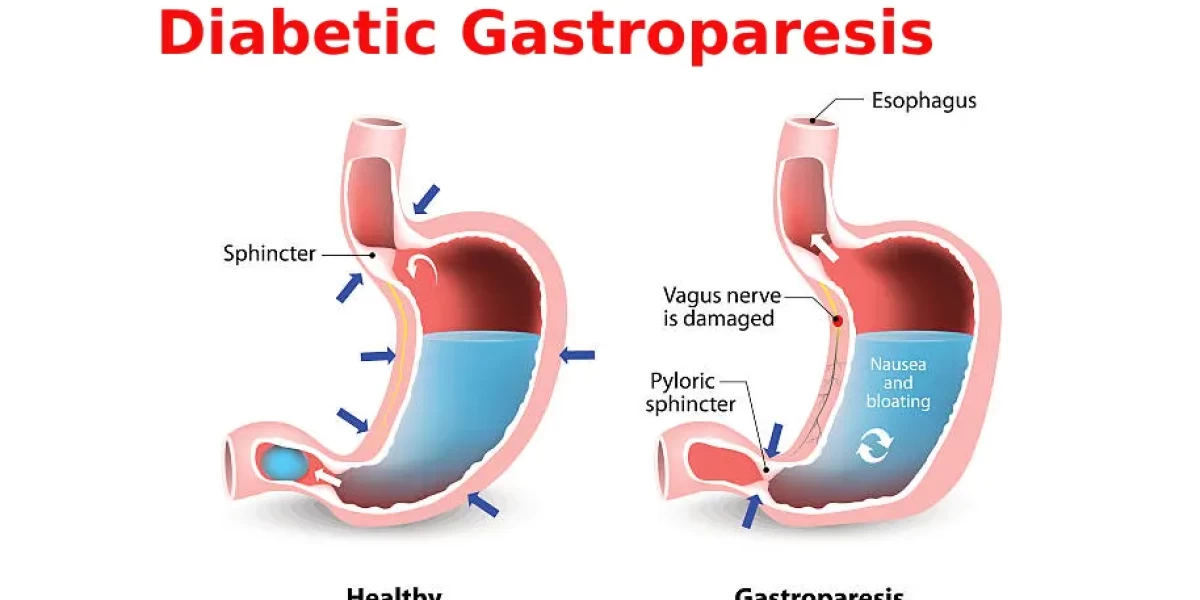
Several risk factors can increase the likelihood of developing BPH. Family history is one of the most significant risk factors, as men with close male relatives who have experienced prostate enlargement are more likely to develop the condition themselves. Obesity is another major risk factor, as excess body weight can contribute to hormonal imbalances that promote prostate growth. Men with diabetes also face an increased risk due to the metabolic changes associated with the disease. Understanding these risk factors can help men assess their own likelihood of developing BPH and encourage early screening and lifestyle adjustments to manage their risk.
Benign Prostatic Hyperplasia Symptoms
The symptoms of BPH revolve around urinary function, with one of the most common complaints being urinary frequency. Men with BPH often feel the need to urinate more frequently, especially at night (a condition known as nocturia). This can disrupt sleep and lead to fatigue and irritability throughout the day. In addition to increased frequency, many men experience a strong sense of urgency, feeling that they must urinate immediately once the urge arises, which can interfere with daily activities.
Another common symptom is difficulty starting or stopping urination. Men with BPH may struggle to initiate a urine stream, and once they do, it can be weak or interrupted. Stopping urination can also be challenging, leading to dribbling or the sensation that the bladder hasn’t fully emptied. These symptoms can lead to frustration and embarrassment, significantly affecting quality of life. Early recognition of these symptoms is crucial, as they can worsen over time and lead to complications if left untreated.
How Is Benign Prostatic Hyperplasia Diagnosed?
Diagnosing BPH typically begins with a review of the patient’s medical history and a physical examination, including a digital rectal exam (DRE). During the DRE, a healthcare professional checks the size and shape of the prostate to detect any abnormalities. While this exam can provide valuable insights, further tests are often needed to confirm the diagnosis and assess the severity of the condition.
One of the most common tests used in diagnosing BPH is the prostate-specific antigen (PSA) test. This blood test evaluates the levels of PSA, a protein generated by the prostate gland. Elevated PSA levels can indicate the presence of BPH, but they can also signal other prostate issues, such as prostatitis or prostate cancer. Therefore, the PSA test is usually used in conjunction with other diagnostic tools to get a clearer picture of prostate health.
In some cases, an ultrasound or imaging test may be performed to evaluate the size of the prostate and assess how much it is affecting the bladder and urethra. Urodynamic tests, which measure bladder function and urine flow, can also help determine the impact of BPH on the urinary system. Consulting a healthcare professional is essential for an accurate diagnosis, as BPH symptoms can mimic those of other serious conditions, such as prostate cancer. Early diagnosis allows for timely treatment and can prevent complications.
Treatment for Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia (BPH) can be treated through a variety of approaches, including lifestyle changes, medications, and surgical interventions. Each treatment option comes with its pros and cons, allowing men to choose the best approach based on the severity of their symptoms and their overall health.
Lifestyle changes are often the first line of treatment for men with mild BPH symptoms. Simple adjustments like reducing fluid intake before bedtime, limiting caffeine and alcohol, and maintaining a healthy weight can help ease symptoms such as frequent urination or a weak urine stream. Although lifestyle changes don’t cure BPH, they can manage symptoms and improve quality of life without side effects. However, they may not be sufficient for men with more severe symptoms.
Medications are another common treatment option for BPH. Alpha-blockers, such as tamsulosin, work by relaxing the muscles in the prostate and bladder neck, making urination easier. 5-alpha reductase inhibitors, like finasteride, reduce the size of the prostate over time by decreasing hormone levels that cause prostate growth. The benefit of medications is that they are non-invasive and can significantly reduce symptoms. However, they can come with side effects like dizziness, headaches, and sexual dysfunction. Some men may also need to take medications long-term to keep their symptoms under control.
For men with more severe BPH or those who don’t respond well to medications, surgical interventions may be necessary. Minimally invasive procedures like transurethral resection of the prostate (TURP) involve removing part of the prostate to relieve pressure on the urethra. Laser therapies are also available, using targeted energy to shrink or remove prostate tissue. Surgery offers more permanent relief of symptoms but comes with risks like infection, incontinence, or sexual dysfunction. It is generally recommended for men whose quality of life is significantly impacted by BPH.
Benign Prostatic Hyperplasia Prevention
Preventing or managing the symptoms of Benign Prostatic Hyperplasia involves adopting a proactive approach to overall health. Maintaining a healthy diet rich in fruits, vegetables, and whole grains is key. Foods high in antioxidants, such as tomatoes (rich in lycopene), and healthy fats like omega-3s from fish, are known to promote prostate health. A balanced diet can help manage weight, which in turn can reduce the risk of developing BPH, as obesity has been linked to an increased risk of prostate enlargement.
Regular exercise is another crucial prevention strategy. Physical activity improves circulation, reduces inflammation, and helps control weight—factors that all play a role in prostate health. Moderate aerobic exercises like walking, swimming, and cycling can be especially beneficial. Staying active not only reduces the risk of BPH but also improves overall health, reducing the likelihood of complications from other chronic conditions.
Routine medical check-ups are also important in the prevention and early detection of BPH. Men over the age of 50 should have regular prostate exams and discuss any urinary changes with their healthcare provider. Early detection allows for more treatment options and can prevent the progression of symptoms. Taking a proactive approach to prostate health can significantly reduce the impact of BPH later in life.
Living with Benign Prostatic Hyperplasia
Living with Benign Prostatic Hyperplasia can affect both the physical and emotional well-being of men. The frequent need to urinate, especially during the night, can disrupt sleep and lead to fatigue, irritability, and anxiety. The embarrassment of needing to use the bathroom frequently, especially in public or social settings, can also contribute to feelings of isolation or frustration. It’s important for men living with BPH to recognize these emotional impacts and seek support when needed.
Coping strategies are essential for managing both the physical and emotional aspects of BPH. One of the best approaches is to maintain open communication with healthcare providers. Discussing symptoms and concerns with a doctor can lead to more effective management of BPH, as well as reassurance about the treatment plan. Joining support groups or online communities can also provide emotional relief by connecting with others who are experiencing similar challenges.
Support from loved ones is equally important. Talking openly with family members about the condition can ease feelings of isolation and foster a more supportive environment. Partners, in particular, can play a vital role in providing emotional encouragement and helping to navigate the challenges of living with BPH.
Conclusion
In conclusion, understanding and managing Benign Prostatic Hyperplasia involves exploring various treatment options, from lifestyle changes and medications to surgical interventions. Preventing BPH or managing its symptoms is possible through healthy eating, regular exercise, and routine medical check-ups. Living with BPH also has emotional and psychological aspects that can be addressed with proper support and communication. Early intervention and ongoing management are essential to minimizing the impact of BPH on daily life. Men experiencing symptoms should seek medical advice and take a proactive approach to maintaining their prostate health.
Frequently Asked Questions(FAQ's)
-
What is the cause of benign prostatic hyperplasia (BPH)?
-
The exact cause of BPH is unclear, but it is believed to be related to aging and changes in male hormones, particularly dihydrotestosterone (DHT), which can cause the prostate gland to enlarge.
-
What is the best treatment for BPH symptoms?
-
Treatment options for BPH include lifestyle changes (such as reducing fluid intake before bed and avoiding caffeine and alcohol), medications (like alpha-blockers and 5-alpha-reductase inhibitors), and minimally invasive procedures or surgery if necessary.
-
What are the causes of BPH?
-
The causes of BPH are not fully understood, but risk factors include aging, family history, obesity, lack of physical activity, and conditions like type 2 diabetes and erectile dysfunction.
-
What is the procedure for treatment of benign prostatic hyperplasia?
-
Treatment procedures for BPH can include medications, minimally invasive therapies (like transurethral resection of the prostate (TURP) or laser therapy), and lifestyle changes.
-
How is BPH permanently treated?
-
There is no permanent cure for BPH, but treatments can effectively manage symptoms and improve quality of life. Surgical options like TURP can provide long-lasting relief.
-
What is the best drink to shrink the prostate?
-
Green tea is often recommended for prostate health due to its potential anti-inflammatory and antioxidant properties. Other beneficial drinks include water, tomato juice, and herbal teas like nettle root and hibiscus.
-
Which fruit is best for the prostate?
-
Fruits high in antioxidants and anti-inflammatory properties, such as berries (blueberries, strawberries), tomatoes, and citrus fruits, are beneficial for prostate healt.
-
How to clean prostate naturally?
-
Natural methods to support prostate health include staying hydrated, eating a balanced diet rich in fruits and vegetables, regular exercise, and avoiding foods and drinks that can irritate the prostate (like caffeine and alcohol).
-
What is the 5-second exercise to shrink the prostate?
-
There isn't a specific 5-second exercise to shrink the prostate. However, regular pelvic floor exercises (Kegels) can help improve urinary symptoms associated with BPH.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.