Introduction
The bubonic plague, often referred to as the "Black Death," is one of the most infamous diseases in history, remembered for its devastating impact on Europe and Asia during the Middle Ages. Responsible for claiming millions of lives, it remains a haunting reminder of the power of infectious diseases. The bubonic plague is caused by the bacterium Yersinia pestis, and although medical advancements have made it treatable today, cases still arise, particularly in certain regions worldwide. Understanding the bubonic plague's causes, symptoms, and transmission methods is essential to protect public health and prevent outbreaks, which, while rare, still pose a threat in various parts of the world.
Causes and Risk Factors of Bubonic Plague
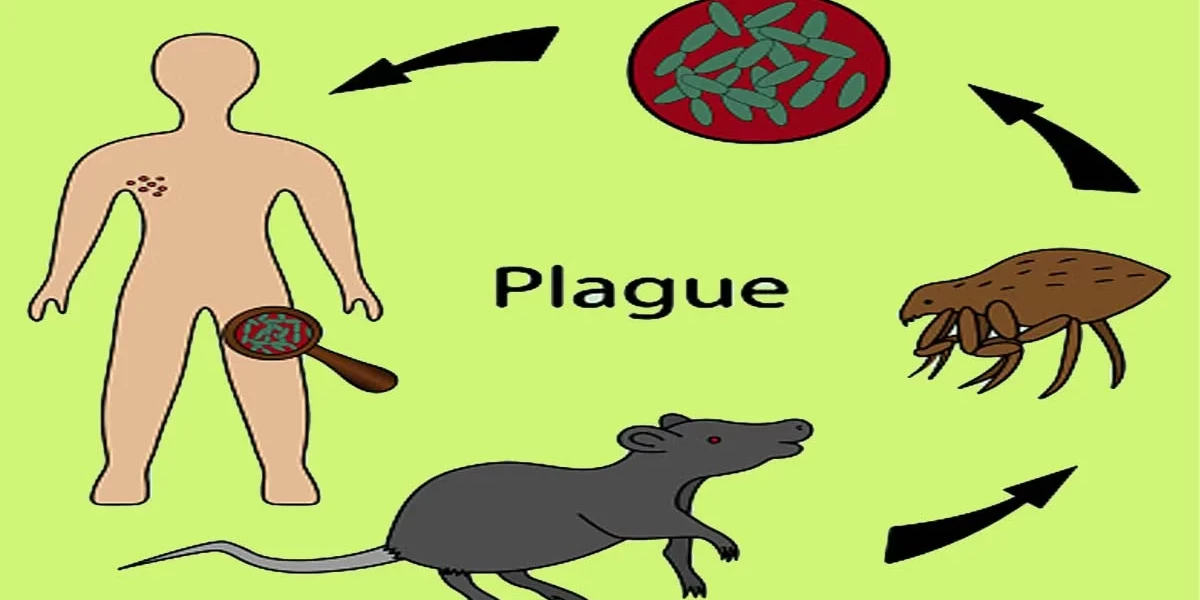
The primary cause of bubonic plague is infection with the bacterium Yersinia pestis. This bacterium is typically found in rodents and other small mammals and spreads to humans through fleas that have fed on infected animals. Fleas serve as vectors for Yersinia pestis, biting both animals and humans, thus transmitting the bacteria from host to host. The bacterium can enter the body through flea bites, where it then travels to the lymphatic system, causing swelling and infection of lymph nodes, a hallmark symptom of the bubonic plague.
In addition to flea bites, other modes of transmission include contact with bodily fluids or tissues of infected animals, which can occur through hunting, handling, or consuming infected animals. In rarer cases, the disease can be transmitted through respiratory droplets from a person or animal with pneumonic plague, another form of plague that affects the lungs. However, person-to-person transmission of bubonic plague is exceedingly rare and usually only happens under specific conditions.
Several risk factors increase susceptibility to bubonic plague. Geographic location is a significant risk factor, as cases of the plague are more prevalent in certain regions, including parts of Africa, Asia, and the western United States, where the bacterium and its vectors are present. Living in rural or semi-rural areas where there is a high population of rodents and fleas can also heighten the risk. Furthermore, socioeconomic conditions play a role, as poverty and limited access to healthcare can increase the likelihood of exposure to infected animals and delay treatment, thus raising the risk of severe outcomes.
Signs and Symptoms of Bubonic Plague
The bubonic plague, one of the most infamous diseases in history, is primarily known for its rapid onset of severe symptoms that, if untreated, can quickly escalate to a life-threatening condition. The initial signs of bubonic plague usually appear within 1 to 7 days of exposure to the bacteria Yersinia pestis, which is transmitted to humans through the bite of an infected flea or through contact with contaminated fluids or tissues. One of the hallmark symptoms of this disease is the sudden onset of high fever, which can range from 100.4°F (38°C) to as high as 104°F (40°C), often accompanied by intense chills. In many cases, this fever is coupled with profound weakness, making the person feel extremely fatigued, even after minimal physical exertion.
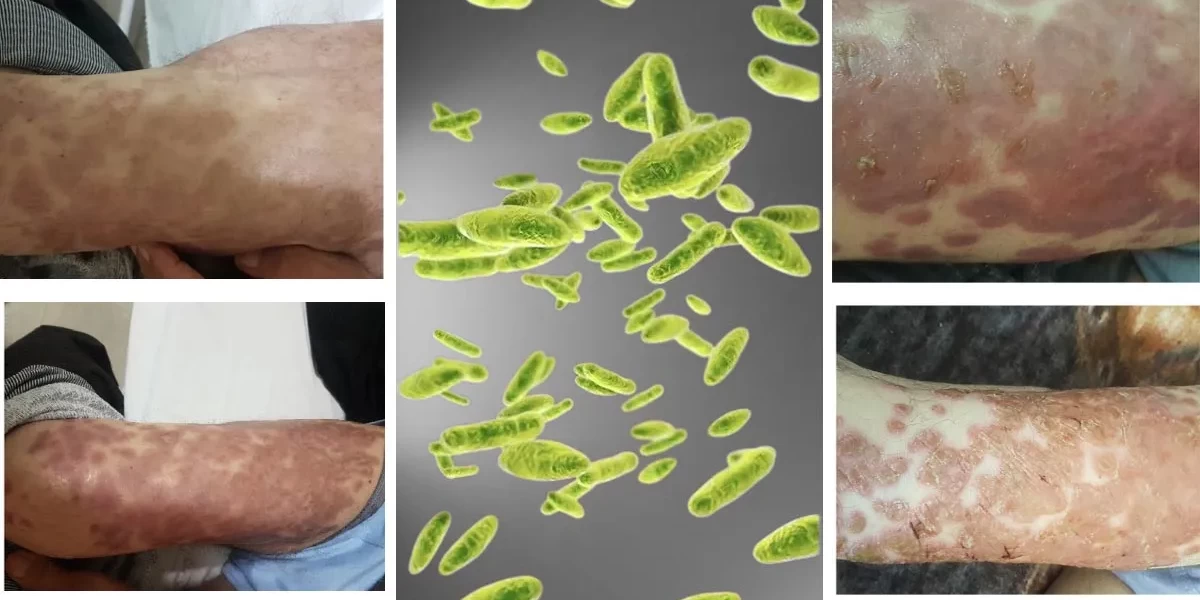
One of the most recognizable signs of bubonic plague is the formation of swollen lymph nodes, commonly known as “buboes.” These swollen lymph nodes are usually painful and appear close to the area where the bacteria entered the body, such as the armpit, groin, or neck. They can grow to be as large as a chicken egg and are often tender to the touch, appearing red and inflamed. The presence of buboes is not only a key indicator for healthcare professionals in diagnosing the disease but also serves as a warning sign for the affected person to seek immediate medical attention. Other accompanying symptoms may include intense headaches, muscle aches, and gastrointestinal distress, such as nausea and vomiting. As the disease progresses, these symptoms can worsen, and without timely treatment, the bacteria may spread to other parts of the body, leading to a more severe form of the disease.
Early recognition of bubonic plague symptoms is essential for effective treatment and containment. Given that this disease can progress rapidly, any delays in seeking medical attention could result in severe complications or even death. Therefore, understanding the symptoms and knowing when to seek medical care is crucial, especially for individuals living in or traveling to areas where the disease is known to be present. Swift identification and response can significantly reduce the mortality rate associated with the bubonic plague, making awareness and early action vital in preventing the spread of this infectious disease.
How Is Bubonic Plague Diagnosed?
Diagnosing bubonic plague accurately and swiftly is critical due to the disease's rapid progression and potential to cause severe complications if left untreated. When a patient presents with symptoms consistent with bubonic plague, healthcare providers typically start with a thorough review of the patient’s medical history and recent activities, as exposure to animals, flea bites, or visits to endemic areas can increase the likelihood of infection. A detailed history can provide crucial context, as the bubonic plague is rare in modern times and often mistaken for other illnesses that share similar symptoms, like influenza or other bacterial infections.
Laboratory tests are essential for confirming a diagnosis of bubonic plague. Blood samples are often collected to detect the presence of Yersinia pestis bacteria, and these samples undergo blood cultures to determine if the bacterium is present in the patient’s bloodstream. In addition to blood cultures, healthcare providers may aspirate fluid from swollen lymph nodes (buboes) to check for the bacteria, as this fluid often provides a more direct sample for testing. Polymerase chain reaction (PCR) testing, which is used to detect the DNA of Yersinia pestis, is another modern diagnostic tool that can provide rapid and reliable results. PCR testing is particularly valuable because it can detect the bacterium even when present in small quantities, allowing for early diagnosis before the infection spreads to other parts of the body.
Prompt diagnosis of bubonic plague is essential to ensure the patient receives appropriate treatment as early as possible. Since the disease can be life-threatening, healthcare providers are trained to recognize the signs quickly and to initiate testing immediately if bubonic plague is suspected. Once diagnosed, treatment with antibiotics, such as streptomycin, doxycycline, or gentamicin, is typically started right away. Without prompt diagnosis and treatment, the disease can progress to more severe forms, such as septicemic or pneumonic plague, which have higher mortality rates and can be more challenging to treat. Therefore, the expertise of healthcare professionals, combined with efficient diagnostic tools, plays a crucial role in containing and managing bubonic plague cases.
Duration of Bubonic Plague
The duration of the bubonic plague, often known as the Black Death due to its historical significance, generally spans from the initial onset of symptoms to either recovery or progression to severe illness, lasting between one to two weeks without intervention. The bubonic plague begins with flu-like symptoms, typically within 2-6 days following exposure to the Yersinia pestis bacteria. These symptoms include fever, chills, headache, and the hallmark swollen and painful lymph nodes, or "buboes," typically located in the groin, armpits, or neck. If left untreated, the disease can progress quickly, worsening in a matter of days and potentially leading to death within a week in severe cases. Early in the infection, fever and fatigue dominate, but within 24-48 hours, the buboes may begin to swell, becoming extremely tender as the infection spreads to the lymphatic system. Over the next few days, untreated cases often see escalating fevers, organ failure, and septic shock as the bacteria spread through the bloodstream, resulting in the most severe form, septicemic plague.
The timeline for recovery largely depends on the speed at which medical intervention is sought. If diagnosed and treated early with appropriate antibiotics, most patients begin to show signs of recovery within 24-72 hours. The recovery period after this stage can vary based on factors such as the patient’s age, immune system strength, and any preexisting health conditions. Generally, younger, healthier individuals experience shorter recovery periods, whereas those with weakened immune systems or existing health issues may require a longer recovery phase and additional supportive care. Environmental factors, such as access to healthcare facilities and the availability of antibiotics, also significantly impact the duration of the disease. In areas with limited healthcare infrastructure, the illness may last longer due to delayed treatment, increasing the risk of severe complications. Consequently, early medical attention is crucial, as it drastically reduces the illness duration and mitigates the risk of complications. Rapid diagnosis and timely intervention not only improve the chances of survival but also play a critical role in preventing the spread of this highly contagious disease, underscoring the necessity of swift medical response to any suspected cases of bubonic plague.
Treatment and Medication Options for Bubonic Plague
Treating the bubonic plague requires swift and aggressive intervention, primarily through the use of antibiotics. The most effective antibiotics include streptomycin, gentamicin, doxycycline, and ciprofloxacin, which are highly effective at eliminating Yersinia pestis bacteria if administered early. When antibiotics are given within the first 24 hours of symptom onset, the chances of recovery improve significantly, often yielding a full recovery within a week of treatment. Streptomycin and gentamicin, in particular, are powerful antibiotics that target the bacterial infection directly, while doxycycline and ciprofloxacin are sometimes preferred due to their effectiveness and wider availability in certain regions.
In addition to antibiotics, supportive care plays a vital role in managing symptoms and enhancing the patient’s chances of survival. Supportive measures may include intravenous fluids to prevent dehydration, oxygen therapy if respiratory distress occurs, and medication to manage fever and pain. In more severe cases where the infection has progressed to septicemic or pneumonic plague, additional intensive care interventions may be required. For instance, mechanical ventilation may be necessary if the infection has caused lung failure. Alongside physical treatments, isolation measures are crucial to prevent the spread, particularly in pneumonic plague cases, which are highly contagious via respiratory droplets. Early treatment is key, as the effectiveness of antibiotics decreases significantly as the disease progresses, especially in cases where it transitions from bubonic to septicemic or pneumonic forms. In such advanced cases, the bacteria can spread to the bloodstream or lungs, leading to severe complications like organ failure, sepsis, and potentially death. Thus, early medical intervention not only shortens the recovery timeline but also significantly reduces the risk of serious, life-threatening complications, making it essential for anyone exhibiting symptoms of the bubonic plague to seek medical attention immediately.
Complications of Bubonic Plague
The bubonic plague, a severe infectious disease caused by the bacterium Yersinia pestis, is infamous for its historical impact and potential complications, which can turn a localized infection into a life-threatening situation. When left untreated, the disease can lead to severe health complications such as septicemia and pneumonia, each associated with high mortality rates and complex medical challenges. Septicemia, or blood infection, is a common complication in which the plague bacterium spreads from the lymphatic system into the bloodstream, causing a rapid inflammatory response that can leading to organ failure, shock, and potentially fatal outcomes if not treated swiftly. Pneumonic plague, another serious complication, occurs when Y. pestis infects the lungs, making it both highly contagious and lethal. Pneumonic plague can spread through respiratory droplets, raising the risk of widespread outbreaks, especially in densely populated areas. For patients, these complications can escalate quickly, leading to death within 24 hours in severe cases. Recognizing early symptoms such as high fever, severe headache, chills, muscle pain, and general malaise is crucial for timely intervention, as these can signal the transition of a localized infection into a systemic one. Advanced medical care, including intravenous antibiotics, fluids, and supportive care, becomes essential once the disease has progressed to these stages. However, awareness of these complications remains key for both medical professionals and the public, as timely intervention and proper treatment are critical to improving survival rates and preventing further transmission.
Prevention of Bubonic Plague
Preventing the spread of the bubonic plague requires a multifaceted approach that includes public health initiatives, personal hygiene practices, and strategies for reducing contact with potentially infected animals. Public health agencies, especially in areas where the plague is known to circulate, play an essential role in disease prevention by monitoring rodent populations, implementing pest control measures, and educating the public about risk factors. These agencies also help control outbreaks by informing healthcare providers of early signs to watch for, thus facilitating rapid response to prevent widespread transmission. On an individual level, personal hygiene and protective practices are crucial in reducing exposure risks. People are advised to avoid handling rodents and use insect repellents in areas where flea populations, the primary vectors for Y. pestis, are high. Proper disposal of garbage, maintaining a clean environment, and managing food sources that may attract rodents can further reduce exposure to plague-carrying animals. For those in high-risk areas or working closely with animals, using protective gear such as gloves and avoiding direct contact with wild animals or their carcasses is essential. In areas where the plague is endemic, vaccination is sometimes recommended for high-risk individuals, though it is not widely available. Through these preventive measures, both individuals and communities can lower their risk of exposure to the bubonic plague, thereby helping to control and prevent potential outbreaks.
The Bubonic Plague: Current Research and Statistics
The bubonic plague, infamous for the devastation it caused during historical outbreaks such as the Black Death in the 14th century, remains a subject of significant concern and research today. Despite being commonly associated with historical pandemics, the plague has persisted as a threat in various regions around the world. Modern research and advanced epidemiological tracking methods have shed new light on the disease, leading to more effective control and treatment strategies. Current statistics underscore its impact, with the World Health Organization (WHO) reporting around 1,000 to 2,000 cases annually, primarily in regions like Africa, Asia, and South America. Countries such as the Democratic Republic of Congo, Madagascar, and Peru have seen recurrent outbreaks, drawing attention from international health organizations and prompting a concerted effort to address and contain the disease.
New research also highlights that the disease, caused by the bacterium Yersinia pestis, primarily spreads through flea bites, particularly those from fleas that infest rodents, which remain the main reservoirs. Studies have shown that increased human contact with rodent populations and other environmental changes may contribute to the disease's persistence and potential resurgence. Research efforts have also pinpointed regions in the United States, particularly in the Southwest, where local outbreaks have occurred, albeit rarely, with a handful of cases reported each year.
When it comes to advancements in treatment and prevention, significant progress has been made. Medical research has improved our understanding of effective antibiotics like streptomycin, doxycycline, and ciprofloxacin, which, when administered promptly, can drastically improve survival rates. Furthermore, recent studies have explored potential vaccine development, though no fully approved and widely available plague vaccine currently exists. The ongoing research, however, is promising and could pave the way for preemptive measures in high-risk regions.
Globally, efforts to control the plague have also expanded beyond treatment to prevention. WHO and other health bodies work alongside local authorities to educate communities on proper sanitation practices, ways to avoid rodent exposure, and the importance of seeking medical help at the first signs of infection. With modern technology, genetic studies of Y. pestis have even allowed researchers to trace the evolution and transmission patterns of the bacterium, offering insights into how outbreaks might be mitigated in the future. By investing in continued research, enhancing treatment options, and promoting global collaboration, experts remain optimistic about reducing the bubonic plague’s threat and improving prevention methods.
Conclusion
In summary, understanding the history, nature, and ongoing research surrounding the bubonic plague highlights the importance of awareness, early diagnosis, and effective treatment. While global cases remain low, the potential for outbreaks reminds us of the need for vigilance, particularly in high-risk areas. Efforts by health organizations and advancements in medical research continue to pave the way for better prevention and treatment options, empowering communities to take proactive steps against this ancient disease. Staying informed, maintaining proper sanitation, and recognizing early symptoms are essential steps in safeguarding oneself and helping to prevent further transmission.
Frequently Asked Questions(FAQs)
01. What is the diagnosis of bubonic plague?
- The diagnosis of bubonic plague involves clinical evaluation and laboratory tests, including blood cultures, lymph node aspirates, and polymerase chain reaction (PCR) tests to identify the presence of Yersinia pestis.
2. What is the prevention and treatment of plague?
- Prevention: Reducing exposure to rodents and fleas, using insect repellent, keeping pets free of fleas, and avoiding contact with potentially infected animals. There is no plague vaccine available currently.
- Treatment: Antibiotics such as streptomycin and gentamicin are effective in treating plague. Early diagnosis and treatment are crucia.
3. What causes bubonic plague?
- Bubonic plague is caused by the bacterium Yersinia pestis, which is transmitted to humans by the bite of infected fleas that have fed on rodents.
4. What are the symptoms and causes of plague?
- Symptoms: Sudden onset of fever, chills, headache, muscle pain, weakness, and painful, swollen lymph nodes (buboes).
- Causes: The bacterium Yersinia pestis, transmitted by flea bites, direct contact with infected tissues, or inhalation of respiratory droplets from infected individuals.
5. How to prevent bubonic plague?
- Prevent bubonic plague by reducing rodent habitats, using insect repellent, keeping pets free of fleas, and avoiding contact with potentially infected animals.
6. How is bubonic plague treated today?
- Bubonic plague is treated with antibiotics such as streptomycin and gentamicin. Timely diagnosis and swift treatment are crucial for recovery.
7. What is the best treatment for plague?
- The best treatment for plague is the use of antibiotics, particularly streptomycin and gentamicin, administered early in the course of the disease.
8. What are the 5 symptoms of the Black Death in order?
- The five symptoms of the Black Death (bubonic plague) in order are: sudden high fever, chills, headache, muscle pain, and painful, swollen lymph nodes (buboes).
9. Which organ is affected by plague?
The organ primarily affected by bubonic plague is the lymphatic system, specifically the lymph nodes, which become swollen and painful (buboes).
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.