Understanding Bladder Cancer: A Comprehensive Overview
Bladder cancer is a significant health concern, ranking as one of the most common forms of cancer in the world. This disease originates in the tissues of the bladder, an essential organ in the urinary system that stores urine before it is excreted. Bladder cancer can affect individuals of all genders, but it is notably more prevalent in men and those over the age of 55. The increasing incidence of this cancer necessitates heightened awareness about its types, symptoms, causes, and available treatment options. Early detection and understanding of bladder cancer can lead to more effective management and better outcomes for patients. Therefore, it is crucial for individuals to familiarize themselves with the complexities of this disease to recognize potential warning signs and seek timely medical advice. This article delves into the different types of bladder cancer, their symptoms, risk factors, and the latest treatment modalities to provide a well-rounded understanding of this serious condition.
Types of Bladder Cancer
Bladder cancer primarily manifests in three main types: transitional cell carcinoma, squamous cell carcinoma, and adenocarcinoma. Each type is distinct, not only in its cellular origin but also in its growth patterns and prevalence within the population.
Transitional Cell Carcinoma (TCC) is the most common form of bladder cancer, accounting for approximately 90% of all cases. TCC arises from the transitional cells lining the bladder, which are specialized cells capable of stretching as the bladder fills. This type often presents as a superficial tumor that may recur after treatment, making regular monitoring essential. TCC can also be classified further into low-grade and high-grade tumors, which differ in their likelihood to invade deeper layers of the bladder and metastasize to other organs.
Squamous Cell Carcinoma (SCC) is less common, representing about 4% of bladder cancer cases. This type develops from squamous cells, which can form in the bladder lining due to chronic irritation or inflammation, often caused by conditions such as urinary tract infections or the presence of certain risk factors like smoking or exposure to industrial chemicals. SCC tends to be more aggressive than TCC and is more likely to invade deeper tissues.
Adenocarcinoma, the least common type, accounts for about 2% of bladder cancer cases. This cancer originates from glandular cells that produce mucus within the bladder. Adenocarcinoma is often associated with chronic irritation or infection and may present a more aggressive course than the other types. The rarity of this form can lead to challenges in diagnosis and treatment, as it may not respond well to standard therapies used for TCC.
Understanding these types of bladder cancer is crucial for recognizing their symptoms, which may include blood in the urine, frequent urination, pain during urination, or back pain. Awareness of these signs, along with knowledge of the types of bladder cancer, can empower individuals to seek prompt medical attention, improving their chances of early diagnosis and successful treatment. As research continues to evolve, staying informed about the latest treatment options is essential for those diagnosed and for healthcare providers aiming to provide optimal care.

Bladder Cancer Symptoms
Recognizing the symptoms of bladder cancer early can make a significant difference in treatment outcomes. Here are some of the most common warning signs:
Hematuria (Blood in Urine)
One of the earliest and most common signs of bladder cancer is hematuria, or blood in the urine. The blood may be visible (turning the urine pink, red, or brown) or only detectable under a microscope during a urine test. Even a small amount of blood in the urine should not be ignored, as it could be a sign of bladder cancer.
Frequent Urination and Urgency
Bladder cancer can cause changes in urination patterns. Patients may experience an increased need to urinate, even when the bladder isn’t full. Urgency, or a strong and sudden need to urinate, is also common. These symptoms may overlap with conditions like urinary tract infections, which makes early diagnosis crucial.
Pelvic and Abdominal Pain
As bladder cancer progresses, it can cause pain in the pelvic region and lower abdomen. Some patients also report pain during urination, which may be a sign that the cancer has begun to spread beyond the bladder.
Bladder Cancer Causes
The exact cause of bladder cancer isn’t always clear, but several risk factors can increase the likelihood of developing the disease.
Smoking
Smoking is a major cause of bladder cancer, with smokers being up to three times more likely to develop the disease than non-smokers. Harmful chemicals in tobacco smoke enter the bloodstream and are filtered by the kidneys, eventually collecting in the bladder, where they can damage the bladder’s lining.
Chemical Exposure
People who work in industries that involve exposure to certain chemicals, such as dyes, rubber, leather, and textiles, have a higher risk of developing bladder cancer. These chemicals, known as aromatic amines, can cause mutations in bladder cells that lead to cancer.
Chronic Bladder Infections
Frequent bladder infections or inflammation, often linked to long-term catheter use, can increase the risk of bladder cancer. Chronic irritation can cause changes in the bladder cells, which may lead to cancer over time.
Genetics and Family History
While lifestyle factors like smoking and chemical exposure play a significant role, genetics also contribute to bladder cancer risk. People with a family history of bladder cancer are more likely to develop the disease.
Diagnosing Bladder Cancer
Early and accurate diagnosis of bladder cancer is crucial for determining the best treatment options. Here are the most common methods used to diagnose the disease:
Urine Tests
A urine test can detect abnormal cells or blood in the urine, which may be an early sign of bladder cancer. Tests like urine cytology examine urine under a microscope to identify cancer cells.
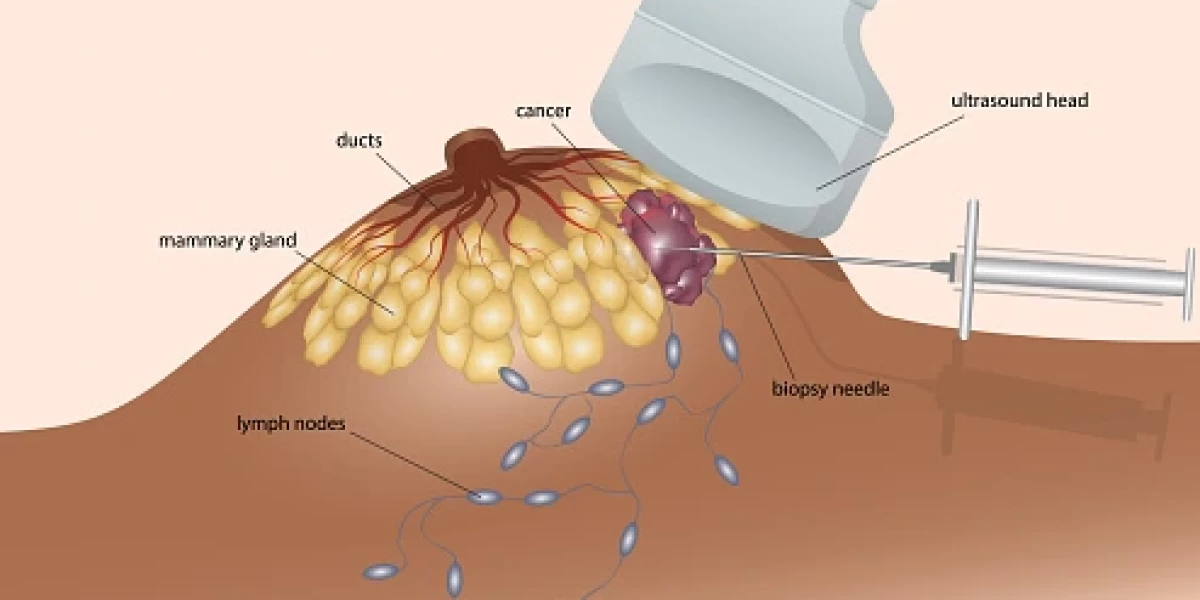
Imaging Studies
Imaging techniques, such as CT scans or ultrasounds, can provide a detailed view of the bladder and surrounding tissues. These scans help identify tumors and assess whether the cancer has spread to other parts of the body.
Cystoscopy
The most definitive method for diagnosing bladder cancer is cystoscopy, in which a thin, flexible tube with a camera (cystoscope) is inserted through the urethra to examine the inside of the bladder. If abnormal tissue is found, a biopsy may be performed to confirm the presence of cancer.
Stages of Bladder Cancer

Bladder cancer is classified into stages based on how far it has spread.
Stage 0
This is the earliest stage, where cancer cells are found only on the surface of the bladder lining and haven’t invaded deeper tissues. It’s often referred to as non-invasive bladder cancer.
Stage I
In stage I, the cancer has grown into the bladder wall but hasn’t yet reached the muscle layer.
Stage II
Stage II bladder cancer involves cancer cells that have spread into the bladder muscle but haven’t moved beyond the bladder.
Stage III
At stage III, the cancer has spread through the bladder muscle to surrounding tissues, such as the prostate in men or the uterus in women.
Stage IV
This is the most advanced stage of bladder cancer, where cancer has spread to nearby organs or distant parts of the body, such as the lungs or bones.
Bladder Cancer Treatment
Bladder cancer can be a daunting diagnosis, but understanding your treatment options can make a big difference in your journey. Treatments for bladder cancer range from surgery to cutting-edge therapies like immunotherapy and targeted treatments. In this article, we'll break down the various methods to treat bladder cancer, explain potential complications, and give you the knowledge to have informed discussions with your healthcare provider.
Surgical Treatments for Bladder Cancer
Transurethral Resection of Bladder Tumor (TURBT)
TURBT is often the first step in diagnosing and treating bladder cancer. This operation entails excising the tumor from the bladder via the urethra. No external incisions are made, which makes recovery easier. TURBT is mainly used for non-muscle invasive bladder cancer, which means the cancer is limited to the inner lining of the bladder.
When is TURBT appropriate? TURBT is generally performed when bladder cancer is detected early. It’s less invasive, and for some patients, it can be enough to remove the cancerous tissue completely.
Cystectomy
A cystectomy is the surgical removal of part or all of the bladder. There are two types: partial cystectomy, where only part of the bladder is removed, and radical cystectomy, which involves removing the entire bladder along with nearby lymph nodes and sometimes other organs.
When is cystectomy required? A cystectomy is usually needed when bladder cancer has spread deeper into the muscle layer of the bladder or when non-invasive treatments haven’t been successful. It is a more invasive surgery but necessary for aggressive forms of cancer.
Chemotherapy for Bladder Cancer
Chemotherapy plays a crucial role in treating bladder cancer both before surgery (neoadjuvant chemotherapy) and after surgery (adjuvant chemotherapy). Chemotherapy uses powerful drugs to destroy cancer cells and prevent them from growing.
- Before surgery, chemotherapy can shrink tumors, making surgery more effective.
- After surgery, it helps eliminate any remaining cancer cells to reduce the risk of recurrence.
Radiation Therapy for Bladder Cancer
Radiation treatment employs high-energy beams to target and destroy cancerous cells. It can be used in combination with other treatments like chemotherapy or as a standalone option for patients who cannot undergo surgery.
Benefits and limitations: Radiation therapy can be effective in shrinking tumors, but it’s not always enough on its own, especially for more advanced bladder cancer.
When is radiation therapy recommended? This is often considered for patients with muscle-invasive bladder cancer or for those who are not fit for surgery due to other health issues.
Immunotherapy for Bladder Cancer
One of the most exciting advancements in cancer treatment is immunotherapy, which harnesses the body’s immune system to attack cancer cells. Bladder cancer patients have seen promising results with certain immunotherapy drugs like checkpoint inhibitors.
Who benefits the most from immunotherapy? Immunotherapy is particularly effective in patients with advanced or recurrent bladder cancer, especially when other treatments have failed. It helps the body recognize and fight cancer more effectively.
Targeted Therapy for Bladder Cancer
Targeted therapies are designed to attack specific molecules within cancer cells that help them grow. These treatments are emerging as game-changers in cancer therapy because they are more precise and often cause fewer side effects than traditional chemotherapy.
What are the potential benefits? Patients with advanced bladder cancer or those whose cancer has specific genetic markers may benefit the most from targeted therapies.
Potential Complications of Bladder Cancer
Bladder cancer treatment can come with its own set of complications, and it’s important to be prepared.
Urinary Incontinence
Urinary incontinence can occur after bladder surgery or as a result of radiation therapy. While it can be distressing, there are management strategies such as pelvic floor exercises, medications, and sometimes additional surgery to improve control.
Sexual Dysfunction
Surgical treatments, especially radical cystectomy, can impact sexual health. Men may experience erectile dysfunction, while women might experience changes in sexual sensation. Open discussions with healthcare providers about preserving sexual function are essential.
Psychological Impact
A cancer diagnosis can adversely affect mental well-being. Fear, anxiety, and depression are common among bladder cancer patients. Seeking psychological support through therapy, support groups, or counseling can help manage the emotional side of cancer.
Managing Side Effects of Treatment
Bladder cancer treatments come with a range of side effects, from physical symptoms like fatigue and nausea to emotional challenges. Coping strategies, such as mindfulness, staying physically active, and leaning on a support network, can help mitigate these effects.
Consulting with Healthcare Providers
Every bladder cancer case is unique, and discussing all available treatment options with your healthcare team is critical. Personalized treatment plans based on your cancer stage, health condition, and personal preferences will ensure the best possible outcome.
Living with Bladder Cancer: Adjusting to Life After a Diagnosis
A diagnosis of bladder cancer can significantly impact a patient’s life, bringing about emotional, physical, and psychological changes. For many, this news introduces a journey that requires lifestyle adjustments, building strong support networks, and developing effective coping strategies. While the road may seem daunting, adopting a proactive approach to self-care and maintaining open lines of communication with healthcare providers can make a big difference in the overall quality of life for bladder cancer patients.
Lifestyle Adjustments After a Bladder Cancer Diagnosis
Bladder cancer often requires significant lifestyle adjustments, particularly if treatments like surgery, chemotherapy, or radiation therapy have been part of the patient’s journey. These changes may affect day-to-day activities, personal relationships, and even work life. For example, those who undergo a cystectomy (partial or radical removal of the bladder) may need to adjust to life with a urinary diversion, such as a urostomy. While this can be a considerable change, medical professionals and specialized nurses can provide support to help patients manage these transitions smoothly.
Fatigue is another common side effect, and many patients find that their energy levels drop during or after treatment. It’s crucial to listen to the body and balance rest with light physical activity. Incorporating gentle exercises like walking or yoga can help regain strength and stamina over time. Dietary adjustments may also be necessary, especially if treatments have affected the digestive system or bladder function. Eating a balanced diet rich in nutrients can aid recovery and boost energy levels, enhancing both physical and emotional well-being.
Building a Support Network: Why It Matters
Living with bladder cancer can feel isolating, but building a robust support network can help ease the emotional burden. Family and friends often provide the first line of support, offering comfort and assistance with daily tasks or simply being there to listen. However, connecting with others who understand the experience of living with cancer can be incredibly beneficial. Support groups, whether in person or online, allow patients to share their experiences, ask questions, and receive emotional reinforcement from others who are going through similar challenges.
Healthcare providers also play an integral role in the support system. Regular check-ins with doctors, nurses, and counselors can help patients stay on track with their treatment plan and manage any side effects. Many hospitals and clinics also offer access to oncology social workers or patient navigators, who can assist with managing the logistical and emotional aspects of a cancer diagnosis.
Coping Strategies: Taking a Proactive Approach to Self-Care
Coping with the emotional and psychological effects of bladder cancer is just as important as managing the physical side. A proactive approach to mental health can help patients navigate the feelings of fear, anxiety, or depression that often accompany a cancer diagnosis. Practices like mindfulness meditation, deep breathing exercises, and cognitive behavioral therapy (CBT) have been shown to reduce stress and improve emotional resilience. Staying mentally engaged through hobbies, reading, or even volunteering can provide a positive distraction and sense of purpose.
Staying in close contact with healthcare providers ensures that patients can address any concerns or symptoms as they arise. It’s essential to maintain an open dialogue with doctors about how treatments are affecting daily life, both physically and emotionally. This proactive approach can prevent complications and help in adjusting treatments as needed to suit the patient’s evolving needs.
Frequently Asked Questions(FAQ's)
-
What are 4 types of bladder cancer?
-
Urothelial (transitional cell) carcinoma
-
Squamous cell carcinoma
-
Adenocarcinoma
-
Small cell carcinoma
-
What is the main cause of bladder cancer?
-
The main cause of bladder cancer is not fully understood, but risk factors include smoking, exposure to certain chemicals, chronic bladder inflammation, and a family history of bladder cancer.
-
What is the biggest symptom of bladder cancer?
-
The biggest symptom of bladder cancer is blood in the urine (hematuria), which can be visible or microscopic.
-
What is the best treatment for bladder cancer?
-
The best treatment for bladder cancer depends on the stage and type of cancer, but common treatments include surgery, chemotherapy, radiation therapy, and immunotherapy.
-
Can bladder cancer be fully cured?
-
Yes, bladder cancer can be fully cured, especially if detected and treated early. However, the likelihood of a cure depends on the stage and type of cancer.
-
What is the first treatment for bladder cancer?
-
The first treatment for bladder cancer often involves surgery to remove the tumor, followed by additional treatments like chemotherapy or immunotherapy depending on the stage and type of cancer.
-
What is the new treatment for bladder cancer in 2024?
-
A new treatment for bladder cancer in 2024 is the combination of enfortumab vedotin and pembrolizumab, which has shown promising results in clinical trials.
-
Can you live a normal life after bladder cancer?
-
Yes, many people can live a normal life after bladder cancer, especially if it is detected and treated early. Regular follow-ups and monitoring are important to ensure the cancer does not return.
-
What is the best test to detect bladder cancer?
-
The best test to detect bladder cancer is a cystoscopy, which allows doctors to examine the inside of the bladder using a scope. Other tests may include urine tests, imaging tests, and biopsy.