Introduction
- Acetylcholine (ACh) is a chemical messenger that carries signals from nerve cells to muscle cells. It is one of the most common and important neurotransmitters in the body, and it is involved in many functions, such as learning, memory, attention, sleep, and movement.
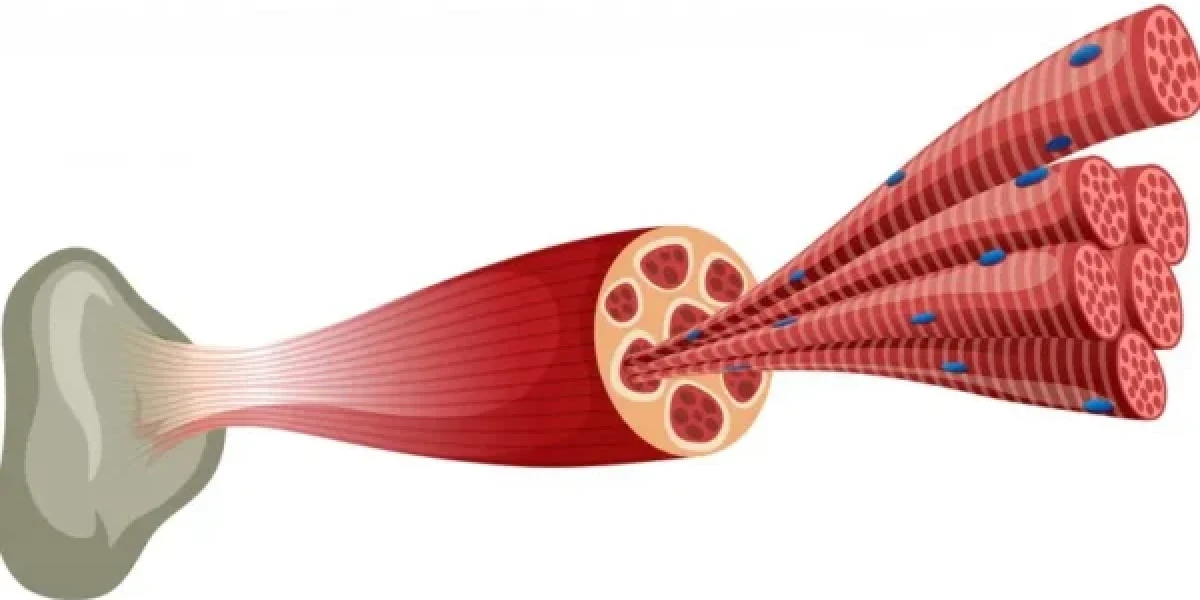
- Muscle contraction is the process by which muscle fibers shorten and generate force. It is essential for various activities, such as breathing, walking, lifting, and maintaining posture. Muscle contraction is controlled by the nervous system, which sends electrical impulses to the muscles via motor neurons.
- Neurotransmitters are substances that transmit signals across the synapses, which are the gaps between nerve cells and their targets. Neurotransmitters are released by the presynaptic cell (the sender) and bind to receptors on the postsynaptic cell (the receiver), causing a change in its electrical or chemical state. Neurotransmitters are crucial for muscle function, as they enable the communication between nerve cells and muscle cells.
Acetylcholine Synthesis and Release
- Synthesis of ACh in nerve terminals: ACh is synthesized in the cytoplasm of the nerve terminals, which are the endings of the motor neurons. The enzyme choline acetyltransferase (ChAT) catalyzes the reaction between choline and acetyl-CoA, producing ACh and CoA. Choline is obtained from the diet or recycled from the breakdown of ACh, while acetyl-CoA is derived from glucose metabolism. Acetylcholine in Muscle
- Storage of ACh in synaptic vesicles: ACh is then transported into the synaptic vesicles, which are small membrane-bound sacs that store neurotransmitters. The transport is mediated by a protein called vesicular acetylcholine transporter (VAChT), which uses the energy of a proton gradient to pump ACh into the vesicles.
- Release of ACh into the synaptic cleft: When an action potential (a brief electrical signal) reaches the nerve terminal, it triggers the opening of voltage-gated calcium channels (VGCCs), which allow calcium ions to enter the cell. The influx of calcium ions causes the synaptic vesicles to fuse with the presynaptic membrane and release ACh into the synaptic cleft, which is the space between the nerve terminal and the muscle cell membrane. Acetylcholine in Muscle
Neuromuscular Junction
- Structure of the neuromuscular junction: The neuromuscular junction (NMJ) is the specialized synapse between a motor neuron and a skeletal muscle fiber. It consists of three main components: the nerve terminal, which contains the synaptic vesicles and the VGCCs; the synaptic cleft, which contains the enzyme acetylcholinesterase (AChE), which breaks down ACh; and the motor end plate, which is the region of the muscle cell membrane that contains the acetylcholine receptors (AChR). Acetylcholine in Muscle
- Nerve impulse transmission at the neuromuscular junction: The nerve impulse transmission at the NMJ is a one-way process, meaning that the signal can only travel from the nerve cell to the muscle cell, and not the other way around. This is because the nerve terminal only releases ACh, while the muscle cell only expresses AChR. The transmission is also very fast and reliable, as each action potential in the nerve cell causes a large amount of ACh release, and each ACh molecule binds to multiple AChR, ensuring a strong and consistent response in the muscle cell.
- Binding of ACh to receptors on the muscle cell membrane: ACh diffuses across the synaptic cleft and binds to AChR on the motor end plate. AChR are ligand-gated ion channels, which means that they open or close in response to the binding of a specific molecule (in this case, ACh). AChR are composed of five subunits, arranged in a ring-like structure, forming a pore in the center. When two ACh molecules bind to two adjacent subunits, the pore opens and allows sodium ions to flow into the muscle cell and potassium ions to flow out of the muscle cell. Acetylcholine in Muscle
Acetylcholine Receptor Activation
- Structure of acetylcholine receptors (AChR): There are two main types of AChR: nicotinic and muscarinic. Nicotinic AChR are found at the NMJ and in some parts of the brain, while muscarinic AChR are found in the heart, smooth muscles, glands, and other parts of the brain. Nicotinic AChR are named after their ability to be activated by nicotine, a plant alkaloid that mimics the action of ACh. Muscarinic AChR are named after their ability to be activated by muscarine, a mushroom toxin that also mimics the action of ACh. Acetylcholine in Muscle
- Activation of AChR by ACh binding: As mentioned above, the binding of ACh to nicotinic AChR at the NMJ causes the opening of the ion channel and the influx of sodium ions and the efflux of potassium ions. This creates a net positive charge inside the muscle cell, which depolarizes the membrane potential (the difference in electrical charge across the membrane). This depolarization is called the end-plate potential (EPP), and it is the first step in the generation of an action potential in the muscle cell. Acetylcholine in Muscle
- Generation of action potential in the muscle cell: The EPP is a local and graded potential, meaning that it varies in size depending on the amount of ACh released and bound, and that it decays over distance. Therefore, the EPP alone is not enough to trigger an action potential, which is a uniform and all-or-none potential, meaning that it has a fixed size and shape, and that it propagates without decay along the membrane. To initiate an action potential, the EPP must reach a certain threshold level, which is determined by the voltage-gated sodium channels (VGSCs), which are distributed along the muscle cell membrane. When the EPP reaches the threshold, the VGSCs open and allow a large influx of sodium ions, which further depolarizes the membrane and initiates the action potential. The action potential then travels along the muscle cell membrane, activating more VGSCs and maintaining its amplitude.
Role of Acetylcholine in Muscle Fiber Excitation
- Propagation of action potential along the sarcolemma: The sarcolemma is the term used to describe the muscle cell membrane and the transverse tubules (T-tubules), which are invaginations of the membrane that penetrate deep into the muscle cell. The T-tubules allow the action potential to reach the interior of the muscle cell, where it can activate the sarcoplasmic reticulum (SR), which is a specialized organelle that stores calcium ions. Acetylcholine in Muscle
- Release of calcium ions from the sarcoplasmic reticulum: The SR is composed of two regions: the terminal cisternae, which are enlarged sacs that contain high concentrations of calcium ions, and the longitudinal tubules, which are narrow tubes that connect the terminal cisternae and run parallel to the T-tubules. The SR is also equipped with two types of calcium channels: the ryanodine receptors (RyR), which are located on the terminal cisternae and release calcium ions into the cytoplasm, and the Sarco/endoplasmic reticulum calcium ATPase (SERCA), which are located on the longitudinal tubules and pump calcium ions back into the SR. The release of calcium ions from the SR is triggered by the action potential that travels along the T-tubules. The T-tubules and the terminal cisternae are closely apposed, forming a structure called the triad. The T-tubules contain a protein called dihydropyridine receptor (DHPR), which is a voltage sensor that detects the change in membrane potential. The DHPR is physically and functionally coupled to the RyR, such that when the DHPR senses the depolarization, it induces a conformational change in the RyR, which opens the calcium channel and allows calcium ions to flow out of the SR. Acetylcholine in Muscle
- Troponin-tropomyosin complex regulation (continued): When calcium ions bind to troponin, they cause a conformational change in the protein, which moves the tropomyosin away from the myosin-binding sites, exposing them for the myosin heads to attach. This is the start of the cross-bridge cycle, which is the repeated process of myosin heads binding, pulling, and detaching from the actin filaments, resulting in muscle contraction. Acetylcholine in Muscle
Contraction Mechanism
- Binding of calcium ions to troponin: As explained in the previous section, the release of calcium ions from the sarcoplasmic reticulum is triggered by the action potential that travels along the T-tubules. The calcium ions then bind to troponin, which is a protein that regulates the interaction between the actin and myosin filaments. Troponin has three subunits: troponin C (TnC), which binds to calcium ions; troponin I (TnI), which inhibits the binding of myosin to actin; and troponin T (TnT), which binds to tropomyosin, which is another protein that covers the myosin-binding sites on actin. When calcium ions bind to TnC, they cause a conformational change in the troponin complex, which moves TnI away from the actin filament and TnT away from the tropomyosin, exposing the myosin-binding sites on actin.
- Exposure of myosin-binding sites on actin: The exposure of the myosin-binding sites on actin allows the myosin heads to attach and form cross-bridges with the actin filaments. Myosin is a protein that consists of two heavy chains and four light chains, forming a rod-like tail and two globular heads. The myosin heads have two binding sites: one for actin and one for ATP (adenosine triphosphate), which is the energy source for muscle contraction. The myosin heads also have an enzyme called myosin ATPase, which hydrolyzes ATP into ADP (adenosine diphosphate) and Pi (inorganic phosphate), releasing energy and changing the shape of the myosin head. Acetylcholine in Muscle
- Cross-bridge formation and sliding filament theory: The cross-bridge formation and sliding filament theory describe the mechanism by which the actin and myosin filaments slide past each other and shorten the muscle fiber, generating force and movement. The cross-bridge cycle consists of four steps: attachment, power stroke, detachment, and recovery stroke. In the attachment step, the myosin head binds to the actin filament, forming a cross-bridge. In the power stroke step, the myosin head pivots and pulls the actin filament towards the center of the sarcomere (the functional unit of muscle contraction), releasing ADP and Pi. In the detachment step, a new ATP molecule binds to the myosin head, causing it to detach from the actin filament. In the recovery stroke step, the myosin head hydrolyzes the ATP molecule, returning to its original position and ready to bind to another actin site. The cross-bridge cycle repeats as long as there is sufficient calcium and ATP available, resulting in the sliding of the actin and myosin filaments and the contraction of the muscle fiber. Acetylcholine in Muscle
Termination of Acetylcholine Action
- Acetylcholinesterase (AChE) role in synaptic cleft: The action of acetylcholine at the neuromuscular junction is terminated by the enzyme acetylcholinesterase (AChE), which is located on the postsynaptic membrane and in the synaptic cleft. AChE hydrolyzes ACh into acetate and choline, which are then released into the synaptic cleft. The breakdown of ACh prevents the continuous stimulation of the acetylcholine receptors and the depolarization of the muscle cell membrane, allowing the muscle cell to relax and return to its resting state.
- Breakdown of ACh into acetate and choline: The breakdown of ACh into acetate and choline is a fast and efficient process, as AChE has a high affinity and specificity for ACh, and can hydrolyze thousands of ACh molecules per second. The acetate and choline molecules are then removed from the synaptic cleft by diffusion and active transport, respectively. The acetate molecule is either metabolized by the muscle cell or transported into the blood, while the choline molecule is taken up by the presynaptic nerve terminal, where it can be reused for the synthesis of new ACh molecules. Acetylcholine in Muscle
- Recycling of choline for ACh synthesis: The recycling of choline for ACh synthesis is an important mechanism that ensures the availability of ACh for nerve-muscle communication. The choline molecule is transported into the nerve terminal by a protein called high-affinity choline transporter (HACT), which uses the energy of a sodium gradient to pump choline into the cell. The choline molecule then combines with acetyl-CoA, which is derived from glucose metabolism, to form ACh, catalyzed by the enzyme choline acetyltransferase (ChAT). The newly synthesized ACh molecule is then transported into the synaptic vesicle by the vesicular acetylcholine transporter (VAChT), where it is stored until the next nerve impulse arrives. Acetylcholine in Muscle
Disorders Related to Acetylcholine and Muscle Contraction
- Myasthenia gravis and AChR dysfunction: Myasthenia gravis is an autoimmune disease that causes muscle weakness and fatigue, due to the production of antibodies that block or destroy the acetylcholine receptors at the neuromuscular junction. The antibodies prevent the binding of ACh to the receptors, reducing the end-plate potential and the generation of action potential in the muscle cell. The muscle cell becomes less responsive to nerve stimulation, resulting in impaired muscle contraction and function. The side effects of myasthenia gravis incorporate hanging eyelids, twofold vision, trouble gulping, talking, and breathing, and shortcoming in the appendages. The disease can be treated with drugs that inhibit acetylcholinesterase, such as pyridostigmine, which increase the amount of ACh in the synaptic cleft and enhance the stimulation of the remaining receptors. Other treatments include immunosuppressive drugs, such as prednisone, which reduce the production of antibodies, and thymectomy, which is the surgical removal of the thymus gland, which is involved in the immune system. Acetylcholine in Muscle
- Botulinum toxin and inhibition of ACh release: Botulinum toxin is a neurotoxin that is produced by the bacterium Clostridium botulinum, which can cause a serious and potentially fatal condition called botulism, which is characterized by muscle paralysis and respiratory failure. The toxin works by blocking the release of ACh from the nerve terminal, preventing the transmission of nerve impulses to the muscle cell. The toxin binds to the presynaptic membrane and cleaves the proteins that are involved in the fusion of the synaptic vesicles with the membrane, such as SNAP-25, syntaxin, and synaptobrevin. The toxin prevents the exocytosis of ACh into the synaptic cleft, resulting in the loss of muscle contraction and function. The symptoms of botulism include blurred vision, drooping eyelids, slurred speech, difficulty swallowing, and muscle weakness. The disease can be treated with antitoxin, which neutralizes the toxin, and supportive care, such as mechanical ventilation, to assist breathing. Acetylcholine in Muscle
- Therapeutic interventions for acetylcholine-related disorders: Acetylcholine-related disorders can be treated with various therapeutic interventions that target different aspects of the acetylcholine pathway, such as synthesis, release, receptor activation, breakdown, and recycling. Some examples of these interventions are:
- Cholinergic agonists, such as nicotine and muscarine, which mimic the action of ACh and activate the acetylcholine receptors, enhancing the nerve-muscle communication. These drugs can be used to treat conditions such as Alzheimer’s disease, which is associated with a loss of cholinergic neurons in the brain, and nicotine addiction, which is caused by the stimulation of nicotinic receptors in the reward system.
- Cholinergic antagonists, such as atropine and curare, which block the action of ACh and inhibit the acetylcholine receptors, reducing the nerve-muscle communication. These drugs can be used to treat conditions such as bradycardia, which is a slow heart rate, and muscle spasms, which are involuntary contractions of the muscles.
- Cholinesterase inhibitors, such as physostigmine and neostigmine, which inhibit the action of acetylcholinesterase and increase the amount of ACh in the synaptic cleft, enhancing the stimulation of the acetylcholine receptors. These drugs can be used to treat conditions such as myasthenia gravis, as mentioned above, and glaucoma, which is an increased pressure in the eye, and nerve agent poisoning, which is caused by the exposure to chemicals that inhibit acetylcholinesterase and cause excessive muscle contraction and paralysis.
- Choline precursors, such as lecithin and choline chloride, which provide the raw material for the synthesis of ACh in the nerve terminal, increasing the availability of ACh for nerve-muscle communication. These drugs can be used to treat conditions such as age-related cognitive decline, which is associated with a reduced production of ACh in the brain, and liver disease, which is associated with a reduced metabolism of choline.
Conclusion
- In conclusion, acetylcholine is a neurotransmitter that mediates the communication between nerve cells and muscle cells, and enables muscle contraction. It is synthesized and released by nerve cells, and it binds to receptors on muscle cells, causing a depolarization of the membrane and an action potential. The action potential travels along the muscle cell membrane and activates the sarcoplasmic reticulum, which releases calcium ions into the cytoplasm. The calcium ions bind to troponin, which regulates the interaction between the actin and myosin filaments, which generate force and movement. The action of acetylcholine is terminated by the enzyme acetylcholinesterase, which breaks down acetylcholine into acetate and choline, which are then removed from the synaptic cleft. Acetylcholine-related disorders can be treated with various therapeutic interventions that target different aspects of the acetylcholine pathway, such as synthesis, release, receptor activation, breakdown, and recycling. Acetylcholine in Muscle
- Significance of understanding acetylcholine in muscle physiology: Understanding the role of acetylcholine in muscle physiology is important for both basic and clinical research, as it provides insights into the mechanisms and regulation of muscle function, and the causes and treatments of muscle disorders. Acetylcholine is a key molecule for muscle function, and its dysregulation can lead to various disorders, such as myasthenia gravis, botulism, and nerve agent poisoning, which affect the quality of life and survival of millions of people worldwide. Therefore, studying the acetylcholine pathway and its interactions with other molecules and systems can help to improve the diagnosis, prevention, and management of these disorders, and to discover new therapeutic targets and strategies for muscle health and disease. Acetylcholine in Muscle
- Potential avenues for future research: Future research on acetylcholine and muscle contraction can explore various topics and questions, such as:
- How does acetylcholine interact with other neurotransmitters and neuromodulators, such as dopamine, serotonin, and endorphins, and how does this affect muscle function and behavior?
- How does acetylcholine influence the development, maintenance, and regeneration of muscle cells and tissues, and how does this relate to aging, injury, and disease?
- How does acetylcholine affect the plasticity and adaptation of muscle cells and tissues, and how does this relate to exercise, training, and performance?
- How does acetylcholine affect the communication and coordination of muscle cells and tissues, and how does this relate to posture, balance, and movement?
- How does acetylcholine affect the perception and modulation of pain, fatigue, and stress, and how does this relate to muscle function and well-being?
FAQ
- What is acetylcholine?
- Acetylcholine is a neurotransmitter that carries signals from nerve cells to muscle cells, and enables muscle contraction. Acetylcholine in Muscle
- How is acetylcholine synthesized and released?
- Acetylcholine is synthesized in the cytoplasm of the nerve terminals, by the enzyme choline acetyltransferase, which combines choline and acetyl-CoA. Acetylcholine is then transported into the synaptic vesicles, by the protein vesicular acetylcholine transporter, where it is stored until the next nerve impulse arrives. At the point when an activity potential arrives at the nerve terminal, it sets off the kickoff of voltage-gated calcium channels, which permit calcium particles to enter the cell. The influx of calcium ions causes the synaptic vesicles to fuse with the presynaptic membrane and release acetylcholine into the synaptic cleft.
- How does acetylcholine activate the muscle cell?
- Acetylcholine diffuses across the synaptic cleft and binds to acetylcholine receptors on the motor end plate, which are ligand-gated ion channels. The binding of acetylcholine causes the opening of the ion channel and the influx of sodium ions and the efflux of potassium ions, creating a net positive charge inside the muscle cell, which depolarizes the membrane potential. This depolarization is called the end-plate potential, and it is the first step in the generation of an action potential in the muscle cell. The action potential then travels along the muscle cell membrane, activating more voltage-gated sodium channels and maintaining its amplitude.
- How does acetylcholine cause muscle contraction?
- The action potential that travels along the muscle cell membrane activates the sarcoplasmic reticulum, which is a specialized organelle that stores calcium ions. The sarcoplasmic reticulum releases calcium ions into the cytoplasm, which bind to troponin, which is a protein that regulates the interaction between the actin and myosin filaments, which are the contractile proteins that generate force and movement. The binding of calcium ions to troponin causes a conformational change in the troponin-tropomyosin complex, which moves the tropomyosin away from the myosin-binding sites on actin, exposing them for the myosin heads to attach. The myosin heads then bind to the actin filaments, forming cross-bridges, and pull the actin filaments towards the center of the sarcomere, shortening the muscle fiber and generating force and movement. Acetylcholine in Muscle
- How is acetylcholine action terminated?
- The action of acetylcholine at the neuromuscular junction is terminated by the enzyme acetylcholinesterase, which is located on the postsynaptic membrane and in the synaptic cleft. Acetylcholinesterase hydrolyzes acetylcholine into acetate and choline, which are then released into the synaptic cleft. The breakdown of acetylcholine prevents the continuous stimulation of the acetylcholine receptors and the depolarization of the muscle cell membrane, allowing the muscle cell to relax and return to its resting state. The acetate and choline molecules are then removed from the synaptic cleft by diffusion and active transport, respectively. The acetate molecule is either metabolized by the muscle cell or transported into the blood, while the choline molecule is taken up by the presynaptic nerve terminal, where it can be reused for the synthesis of new acetylcholine molecules. Acetylcholine in Muscle
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.