Introduction
A biopsy is a medical procedure in which a small sample of tissue is removed from the body for closer examination under a microscope. This procedure is essential in identifying a wide range of conditions, particularly cancer. By analyzing tissue at the cellular level, doctors can detect abnormalities that may not be visible through imaging or other diagnostic tests. The significance of biopsies in medical diagnostics cannot be overstated—they are the gold standard for confirming or ruling out diseases, determining the aggressiveness of a condition, and guiding treatment decisions. Biopsies provide the detailed information needed to craft personalized treatment plans, making them invaluable in modern medicine.
Why Are Biopsies Conducted?
Biopsies are conducted for several critical reasons, with the primary goal being to confirm a diagnosis. When imaging tests like X-rays, MRIs, or CT scans reveal an abnormal growth or suspicious area, a biopsy is typically the next step. For example, if a lump is found in the breast or an unusual lesion appears on the skin, a biopsy is essential to determine whether the growth is benign (non-cancerous) or malignant (cancerous). This confirmation is vital because it allows doctors to accurately diagnose the condition and recommend the most appropriate treatment.
Another reason biopsies are conducted is to assess the severity or stage of a condition. In the case of cancer, for instance, a biopsy helps determine how advanced the disease is. This includes identifying the type of cancer cells present and how quickly they are likely to grow and spread. Staging a disease is crucial for doctors to develop a treatment plan that is tailored to the patient's specific needs. Whether surgery, chemotherapy, or radiation is required depends heavily on the biopsy results, which provide a clear picture of the disease's progression.
Biopsies are also used to monitor the effectiveness of ongoing treatments. For patients undergoing treatment for conditions like cancer or chronic inflammatory diseases, follow-up biopsies can be conducted to see how well the treatment is working. If the tissue shows improvement, the current treatment plan may continue; if not, doctors may adjust the treatment approach. This ongoing monitoring through biopsies ensures that patients receive the most effective care for their condition.
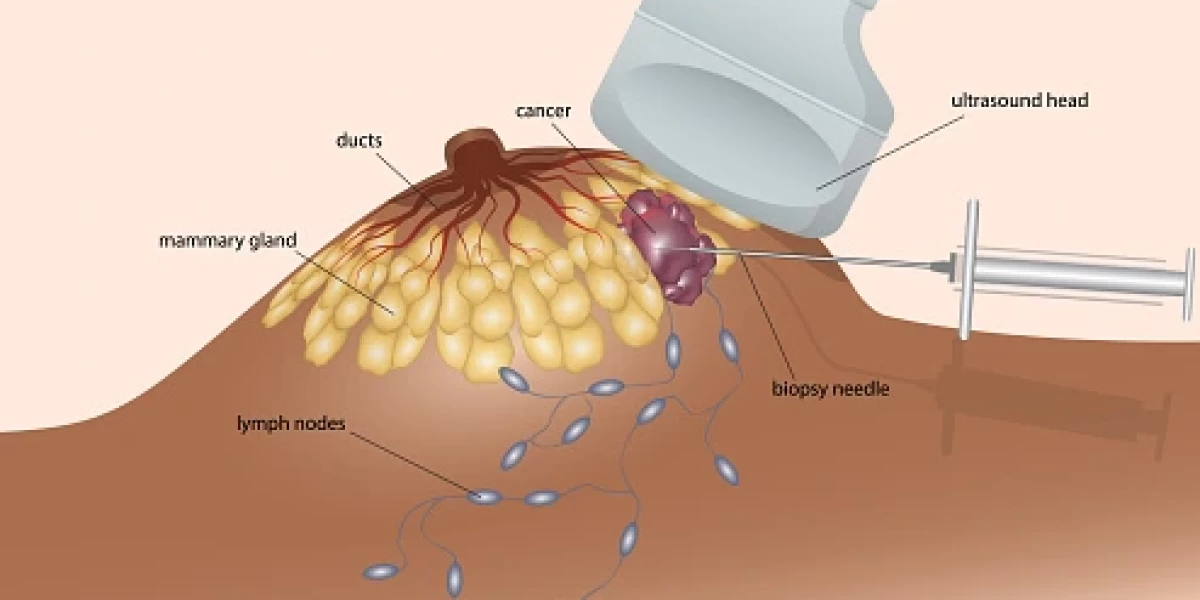
Common conditions that may require a biopsy include breast cancer, liver disease, kidney disease, and skin conditions like melanoma. In breast cancer, a needle biopsy is often performed to sample cells from a suspicious lump, while in liver disease, a liver biopsy may help assess damage or inflammation. In kidney disease, a biopsy can reveal how much damage has occurred and guide treatment to prevent further deterioration. Similarly, a skin biopsy can detect skin cancer or other skin-related conditions, ensuring timely and appropriate intervention.

Types of Biopsy Procedures
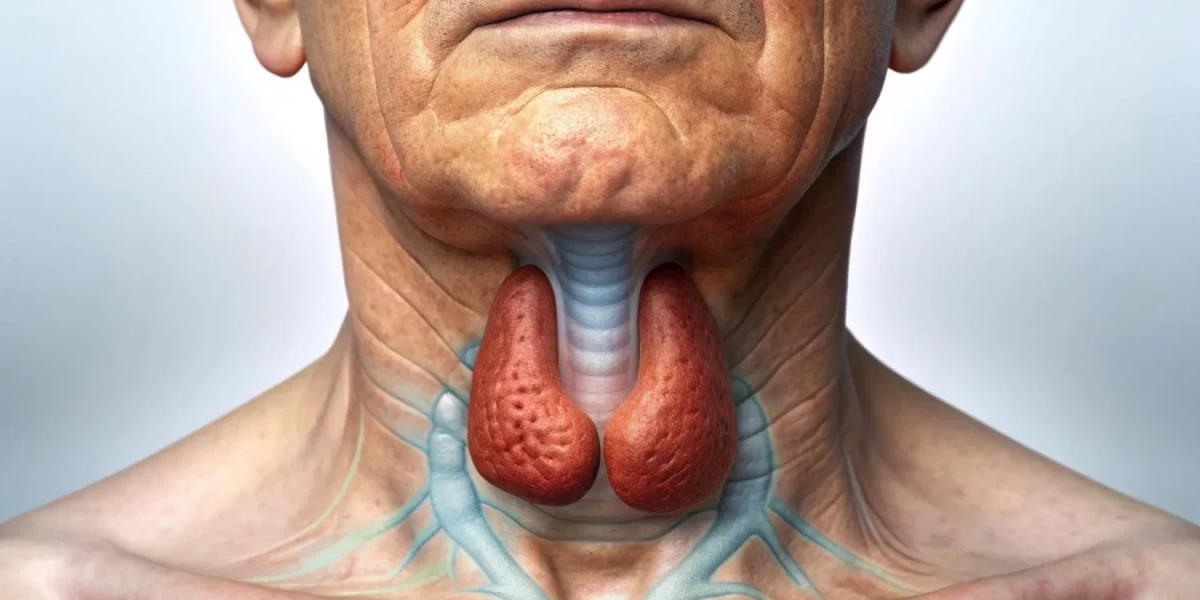
There are several types of biopsy procedures used to diagnose various medical conditions by removing tissue samples for examination. The method chosen depends on the location of the tissue, the condition being investigated, and the patient’s overall health. One of the most common types is the needle biopsy, which uses a thin needle to collect tissue from areas such as the breast, liver, or thyroid. Needle biopsies are less invasive and have a shorter recovery time compared to surgical methods.
Excisional and incisional biopsies are more invasive procedures that involve removing larger tissue samples through surgery. In an excisional biopsy, an entire lump or suspicious area is removed, while in an incisional biopsy, only a portion of the tissue is taken. These procedures are often used when a larger tissue sample is needed for a more accurate diagnosis.
Endoscopic biopsies are performed using a flexible tube with a camera (endoscope) to access internal organs like the stomach, lungs, or colon. This type of biopsy allows for both the visualization of the area and the precise removal of small tissue samples. Each of these biopsy techniques serves a specific purpose and has unique advantages depending on the medical situation.
Needle Biopsy
Needle biopsies, including fine-needle aspiration (FNA) and core needle biopsies, are minimally invasive procedures that offer accurate diagnostic results with minimal discomfort. Fine-needle aspiration uses a very thin needle to extract small amounts of tissue or fluid from suspicious areas, such as cysts or lymph nodes. It is often used for initial screening of lumps in the neck, breast, or thyroid, providing rapid results with minimal tissue disruption. FNA is typically performed in an outpatient setting, and the recovery time is brief.
Core needle biopsies, on the other hand, use a larger needle to remove a cylindrical core of tissue for analysis. This method is preferred when a larger sample is needed to provide a more comprehensive diagnosis. Core needle biopsies are commonly used for breast, liver, and prostate biopsies. They offer a balance between being minimally invasive and providing a substantial tissue sample for pathology, making them highly effective for diagnosing cancer and other conditions.
Both FNA and core needle biopsies are valuable tools for diagnosing diseases with minimal risk and discomfort, allowing patients to avoid more invasive surgical procedures.
Excisional and Incisional Biopsies
Excisional and incisional biopsies are surgical procedures that are used when larger or more complex tissue samples are required for diagnosis. An excisional biopsy involves the complete removal of a suspicious mass or area of tissue. This procedure is typically used when a doctor wants to remove a potentially cancerous tumor in its entirety for further examination. Excisional biopsies are often performed in cases of melanoma, breast lumps, or other localized growths. The advantage of this approach is that it not only provides a diagnosis but can also be a form of treatment if the entire tumor is removed.
In contrast, an incisional biopsy only removes a portion of the tissue or lesion for analysis. This method is used when the affected area is too large to remove completely, or when surgery would be too risky. Incisional biopsies are common in diagnosing conditions like soft tissue sarcomas or large skin lesions. Both procedures require local or general anesthesia and may involve a recovery period depending on the size and location of the biopsy site.
While excisional biopsies are ideal for removing entire lesions, incisional biopsies are better suited for obtaining diagnostic information when complete removal is impractical or unnecessary.
Endoscopic Biopsy
An endoscopic biopsy is a procedure that allows doctors to visualize and sample tissues from inside the body using an endoscope—a flexible tube with a light and camera attached. This technique is particularly useful for diagnosing conditions affecting the gastrointestinal and respiratory systems, such as ulcers, tumors, or infections in the stomach, esophagus, colon, or lungs. The endoscope is inserted through a natural opening, such as the mouth or rectum, allowing the doctor to view the internal organs and guide the collection of tissue samples precisely.
Endoscopic biopsies are less invasive than traditional surgery, reducing the risks of complications and shortening recovery time. The real-time visualization provided by the endoscope helps doctors target abnormal tissues more accurately, ensuring that the biopsy is taken from the most relevant area. This method is also advantageous because it allows the physician to evaluate both the tissue sample and the overall condition of the internal organs during the procedure.
Biopsy Side Effects
Biopsies are essential diagnostic tools, but they come with potential side effects and risks that patients should be aware of. One of the most common side effects is pain, which can vary depending on the biopsy type and location. While most patients experience only mild discomfort, localized pain at the biopsy site may persist for a few days. Over-the-counter pain medications are typically recommended, though stronger prescriptions may be needed in certain cases. Discussing pain management options with your healthcare provider can help alleviate concerns and ensure you're prepared.
Bleeding is another possible side effect, particularly in more invasive biopsies. For example, needle biopsies often result in minor bleeding, while surgical biopsies may require stitches and can lead to more significant blood loss. Although bleeding is usually controlled during the procedure, patients should be cautious afterward. Applying pressure to the biopsy site and following post-procedure care instructions can help prevent complications. In rare cases, patients may experience excessive bleeding or hematoma formation, which should be reported to a doctor immediately.
Infection is a less common but serious risk associated with biopsies. Any time the skin is pierced, there is a possibility of introducing bacteria into the body. Symptoms of infection, such as redness, swelling, warmth, and discharge at the biopsy site, should be monitored closely. Your healthcare provider will typically prescribe antibiotics if they suspect an infection. It’s crucial to keep the area clean and dry after the procedure to reduce this risk. While these side effects may seem alarming, understanding them helps patients make informed decisions and communicate openly with their doctors.
Preparing for a Biopsy
Proper preparation for a biopsy can ease anxiety and ensure the process goes smoothly. Before the procedure, your healthcare provider will give you detailed instructions, which may vary depending on the type of biopsy. For example, patients undergoing a needle biopsy may have minimal preparation, while those scheduled for a surgical biopsy might need to fast for several hours or avoid certain medications. It's important to follow all pre-procedure instructions carefully, as this can affect the accuracy of the biopsy and reduce the risk of complications.
Understanding what to expect during the biopsy is also essential. Most biopsies are outpatient procedures, meaning you’ll go home the same day. Depending on the type of biopsy, you may receive local anesthesia to numb the area, or in some cases, sedation or general anesthesia. Your doctor will explain the process in detail, from how long the biopsy will take to the sensations you may feel during the procedure. Having this information beforehand can help alleviate fear and uncertainty.
After the biopsy, follow-up care is crucial. You may experience mild soreness or swelling at the biopsy site, which is normal. Be sure to follow all post-procedure care guidelines, such as keeping the area clean and dry, avoiding strenuous activity, and monitoring for signs of infection or excessive bleeding. Additionally, some patients may require a follow-up appointment to remove stitches or assess healing. Preparing both physically and mentally for a biopsy can make the experience more manageable and improve recovery outcomes.
Interpreting Biopsy Results
After a biopsy, the tissue sample is sent to a laboratory for analysis, where a pathologist examines it under a microscope. This process involves identifying abnormalities in the cells, such as cancer, infection, or inflammation. The results are typically classified as either benign (non-cancerous) or malignant (cancerous), and your doctor will explain the findings in detail. It’s important to understand that a benign result doesn’t necessarily mean no follow-up is needed, as additional monitoring may be required based on your overall health.
The time frame for receiving biopsy results can vary. In some cases, results are available within a few days, while more complex analyses may take a week or longer. During this waiting period, patients often feel anxious, but staying in communication with your healthcare provider can help manage stress. Once the results are in, your doctor will discuss the next steps. If the biopsy reveals a benign condition, you may not need further treatment. However, if the results indicate cancer or another serious issue, your doctor will outline a treatment plan, which may involve surgery, medication, or additional tests.
The significance of biopsy results varies from case to case. For instance, a biopsy may confirm a diagnosis or provide more information about the severity of a condition. In other instances, a biopsy may indicate the need for further testing. It’s essential to ask questions and understand the implications of the findings so you can make informed decisions about your health moving forward.
Conclusion
In conclusion, biopsies are vital tools in modern medicine, helping doctors diagnose and manage a wide range of conditions. While there are potential side effects, such as pain, bleeding, and infection, these risks are typically minor and manageable with proper care. Preparing for a biopsy by following pre-procedure instructions and understanding what to expect can make the process smoother and reduce anxiety. Interpreting biopsy results is a crucial step in determining the appropriate next steps for treatment or further investigation. If you have concerns about your health that may require a biopsy, don’t hesitate to consult with your healthcare provider. By keeping yourself informed and proactive, you can make the most informed choices for your health.
Frequently Asked Questions(FAQ's)
-
What is the risk of biopsy?
-
Biopsies are generally safe, but they carry some risks such as bleeding, infection, and pain at the biopsy site. The risk varies depending on the type of biopsy and the area being biopsied.
-
Which biopsy is safe?
-
Needle biopsies, such as fineneedle aspiration and core needle biopsy, are considered safer because they are less invasive and have a lower risk of complications.
-
What is a high-risk biopsy?
-
High-risk biopsies are those that have a higher chance of complications or spreading cancer cells. Examples include biopsies of large tumors or those in sensitive areas like the brain or spinal cord.
-
Does biopsy confirm cancer?
-
Yes, a biopsy is the definitive way to confirm the presence of cancer by examining tissue or cells under a microscope.
-
What happens if a biopsy is positive?
-
If a biopsy is positive, it means cancer cells were found. The next steps typically involve further testing to determine the cancer's type, stage, and appropriate treatment options.
-
Can a biopsy tell where cancer started
-
A biopsy can help determine the type of cancer cells present, but it may not always pinpoint the exact origin of the cancer. Additional tests and examinations are often needed to identify the primary site.
-
Can cancer spread due to biopsy
-
While rare, there is a small risk that a biopsy can cause cancer cells to spread to other parts of the body. This risk is minimized by using minimally invasive biopsy techniques.
-
Which test shows cancer?
-
Besides biopsy, other tests that can show cancer include imaging tests (like MRI, CT scans, and PET scans), blood tests, and endoscopy.
-
What happens if a biopsy is negative
-
If a biopsy is negative, it means no cancer cells were found in the sample. However, further tests may still be needed if there are other signs or symptoms of cancer.
*Image credits- freepik*
Important Notice:
The information provided on “health life ai” is intended for informational purposes only. While we have made efforts to ensure the accuracy and authenticity of the information presented, we cannot guarantee its absolute correctness or completeness. Before applying any of the strategies or tips, please consult a professional medical adviser.