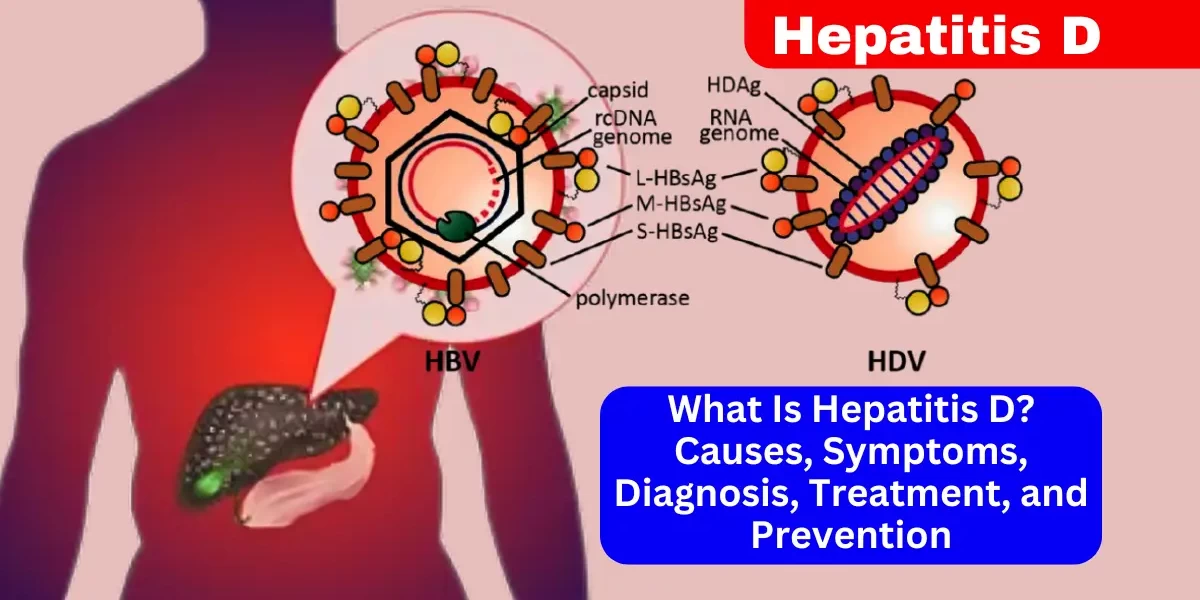
Hepatitis D, referred to as delta hepatitis, is a liver condition triggered by the hepatitis D virus (HDV). Unlike other forms of hepatitis, HDV is unique because it can only infect individuals who are already infected with the hepatitis B virus (HBV). This makes hepatitis D a "satellite" virus, relying on HBV to replicate and cause liver damage. Understanding hepatitis D is crucial because it is considered the most severe form of viral hepatitis, often leading to rapid progression of liver disease, including cirrhosis, liver failure, and even liver cancer.
What Is Hepatitis D?
Hepatitis D is a viral infection that targets the liver, but it’s not your typical virus. It’s defective, meaning it can’t replicate on its own. Instead, it hijacks the hepatitis B virus to complete its life cycle. This dependency makes hepatitis D a co-infection or superinfection in people with HBV.
Superinfections are often more severe, as they can accelerate liver damage and lead to chronic hepatitis D. According to the World Health Organization (WHO), approximately 5% of people with chronic HBV are also infected with HDV, translating to around 15-20 million people worldwide.
The Unique Nature of Hepatitis D
Hepatitis D is caused by the hepatitis D virus (HDV), which is a small, enveloped RNA virus. Unlike other hepatitis viruses, HDV is incomplete and requires the presence of HBV to replicate. This is because HDV lacks certain enzymes and proteins necessary for replication, which it borrows from HBV. This unique relationship makes HDV a satellite virus, dependent on HBV for its survival and propagation.
Transmission of Hepatitis D
HDV spreads via exposure to contaminated blood or various infectious bodily secretions. The most common routes of transmission include:
-
Blood Transfusions and Organ Transplants: Before the widespread screening of blood products, HDV was commonly transmitted through blood transfusions and organ transplants. Today, this route is rare due to rigorous screening processes.
-
Injecting Drug Use: Sharing needles and other drug paraphernalia is a significant risk factor for HDV transmission.
-
Unprotected Sex: HDV can be transmitted through unprotected sexual contact, particularly in individuals with multiple sexual partners or those engaging in high-risk sexual behaviors.
-
Mother-to-Child Transmission: Although less common, HDV can be transmitted from an infected mother to her baby during childbirth.
Global Prevalence of Hepatitis D
The prevalence of HDV varies significantly across different regions of the world. It is most common in areas with high rates of HBV infection, such as parts of Africa, Asia, and South America. In some regions, up to 20% of individuals with chronic HBV are co-infected with HDV. In contrast, the prevalence is much lower in developed countries, where HBV vaccination programs have significantly reduced the incidence of both HBV and HDV.
Hepatitis D Stages
Hepatitis D progresses in stages, much like other forms of hepatitis. Understanding these stages helps in managing the disease effectively:
-
Acute Hepatitis D: This is the initial stage following infection. Symptoms may be mild or severe, depending on whether it’s a co-infection or superinfection. Some people clear the virus naturally during this stage.
-
Chronic Hepatitis D: If the virus persists for more than six months, it becomes chronic. This stage is more common in superinfections and can lead to serious liver complications.
-
Cirrhosis: Chronic hepatitis D often progresses to cirrhosis, where healthy liver tissue is replaced by scar tissue, impairing liver function.
-
Liver Failure or Cancer: In advanced cases, hepatitis D can lead to liver failure or hepatocellular carcinoma (liver cancer).
Acute Hepatitis D
Acute hepatitis D occurs when a person is first infected with HDV. This can happen in two ways:
In co-infections, the immune system often clears both viruses, leading to recovery. However, in superinfections, the presence of chronic HBV provides a fertile ground for HDV to thrive, often leading to chronic hepatitis D.
Chronic Hepatitis D
Chronic hepatitis D develops when the virus persists in the body for more than six months. This stage is more common in superinfections and is associated with a higher risk of severe liver damage. Chronic hepatitis D can lead to progressive liver fibrosis, cirrhosis, and an increased risk of liver cancer.
Cirrhosis
Cirrhosis represents an advanced phase of liver disorder marked by the substitution of normal liver tissue with fibrous scar tissue. This impairs the liver's ability to function properly and can lead to a range of complications, including portal hypertension, ascites (fluid accumulation in the abdomen), and hepatic encephalopathy (brain dysfunction due to liver failure).
Liver Failure or Cancer
In advanced cases, chronic hepatitis D can lead to liver failure, where the liver is no longer able to perform its vital functions. This is a life-threatening condition that requires immediate medical attention. Additionally, chronic hepatitis D significantly increases the risk of hepatocellular carcinoma (HCC), a type of liver cancer.
Hepatitis D Symptoms and Signs
The symptoms of hepatitis D can vary depending on the stage of the infection and whether it’s a co-infection or superinfection. Common hepatitis D symptoms and signs include:
In acute cases, symptoms may appear suddenly and be severe. In chronic cases, symptoms may develop gradually and worsen over time. Some people, however, may remain asymptomatic for years, only to discover the infection during routine blood tests or when liver damage has already occurred.
Acute Hepatitis D Symptoms
In acute hepatitis D, symptoms typically appear within 2-8 weeks after exposure to the virus. These symptoms can range from mild to severe and may include:
-
Fatigue: A common symptom of many liver diseases, fatigue in hepatitis D can be debilitating.
-
Jaundice: Yellowing of the skin and eyes due to the buildup of bilirubin, a byproduct of red blood cell breakdown.
-
Dark Urine: Caused by the excretion of bilirubin in the urine.
-
Abdominal Pain: Often felt in the upper right quadrant of the abdomen, where the liver is located.
-
Nausea and Vomiting: Common symptoms of liver inflammation.
-
Loss of Appetite: A frequent symptom of acute hepatitis, leading to weight loss.
-
Joint Pain: Some individuals may experience joint pain, similar to symptoms seen in other viral infections.
Chronic Hepatitis D Symptoms
In chronic hepatitis D, symptoms may be less pronounced but can persist for years. These symptoms often indicate ongoing liver damage and may include:
-
Persistent Fatigue: Ongoing tiredness that doesn’t improve with rest.
-
Mild Jaundice: Intermittent yellowing of the skin and eyes.
-
Abdominal Swelling: Due to fluid accumulation (ascites) caused by liver dysfunction.
-
Easy Bruising and Bleeding: Resulting from impaired liver function and reduced production of clotting factors.
-
Spider Angiomas: Small, spider-like blood vessels visible under the skin.
-
Hepatic Encephalopathy: Confusion, memory loss, and cognitive impairment due to liver failure.
Asymptomatic Cases
Some individuals with hepatitis D may remain asymptomatic for years, especially in the early stages of the disease. These individuals may only discover their infection during routine blood tests or when complications such as cirrhosis or liver cancer develop.
Hepatitis D Causes and Risk Factors
The primary cause of hepatitis D is infection with the hepatitis D virus, but this can only happen in the presence of HBV. The virus is transmitted through contact with infected blood or other bodily fluids. Key risk factors include:
-
Having chronic hepatitis B
-
Injecting drugs with shared needles
-
Receiving unscreened blood transfusions or organ transplants
-
Engaging in unprotected sex with an infected person
-
Being born to a mother with HBV/HDV (vertical transmission)
Geographically, hepatitis D is more prevalent in regions with high rates of HBV, such as parts of Africa, Asia, and South America.
Causes of Hepatitis D
Hepatitis D is caused by the hepatitis D virus (HDV), which is a defective virus that requires the presence of HBV to replicate. HDV spreads via exposure to contaminated blood or various infectious bodily secretions. The virus can enter the bloodstream through:
-
Direct Blood Contact: Such as sharing needles or receiving contaminated blood products.
-
Sexual Contact: Unprotected sex with an infected person.
-
Mother-to-Child Transmission: Although less common, HDV can be transmitted from an infected mother to her baby during childbirth.
Risk Factors for Hepatitis D
Several factors increase the risk of contracting hepatitis D:
-
Chronic Hepatitis B: Individuals with chronic HBV are at the highest risk of HDV infection.
-
Injecting Drug Use: Sharing needles and other drug paraphernalia is a significant risk factor.
-
Unprotected Sex: Engaging in unprotected sex with multiple partners or with an infected person increases the risk.
-
Healthcare Exposure: Healthcare workers and individuals who receive frequent blood transfusions or organ transplants are at higher risk.
-
Geographic Location: Living in or traveling to regions with high rates of HBV and HDV increases the risk of infection.
Hepatitis D Diagnosis
Diagnosing hepatitis D involves a combination of blood tests and liver function assessments. Key steps in the diagnosis of hepatitis D include:
-
HBV Testing: Since HDV requires HBV, testing for hepatitis B is the first step.
-
HDV Antibody Test: This detects antibodies against HDV, indicating exposure to the virus.
-
HDV RNA Test: This confirms active infection by detecting the virus’s genetic material.
-
Liver Function Tests: These assess the extent of liver damage.
-
Imaging Studies: Ultrasound or MRI may be used to evaluate liver health.
Early diagnosis is critical to prevent complications and manage the disease effectively.
HBV Testing
Since HDV cannot exist without HBV, the first step in diagnosing hepatitis D is to test for hepatitis B. This involves:
-
HBsAg Test: Detects the presence of hepatitis B surface antigen (HBsAg), indicating an active HBV infection.
-
Anti-HBc Test: Detects antibodies against the hepatitis B core antigen, indicating past or present HBV infection.
HDV Antibody Test
The HDV antibody test detects antibodies against HDV, indicating exposure to the virus. There are two types of HDV antibodies:
HDV RNA Test
The HDV RNA test detects the genetic material of the virus, confirming an active HDV infection. This test is crucial for diagnosing chronic hepatitis D and monitoring the effectiveness of treatment.
Liver Function Tests
Liver function tests (LFTs) assess the health of the liver by measuring levels of enzymes, proteins, and other substances produced by the liver. Elevated levels of liver enzymes, such as ALT and AST, indicate liver inflammation and damage.
Imaging Studies
Imaging studies, such as ultrasound, CT scans, or MRI, may be used to evaluate the liver's structure and detect signs of cirrhosis, liver cancer, or other complications.
Prognosis of Hepatitis D
The prognosis of hepatitis D varies depending on the type of infection and the patient’s overall health. Co-infections (HBV and HDV together) often resolve on their own, but superinfections (HDV in someone with chronic HBV) tend to have a poorer prognosis. Chronic hepatitis D can lead to cirrhosis in 70-80% of cases, with a high risk of liver failure or cancer.
Co-infection Prognosis
In co-infections, the immune system often clears both HBV and HDV, leading to recovery. However, some individuals may develop severe acute hepatitis, which can be life-threatening. The overall prognosis for co-infections is generally better than for superinfections.
Superinfection Prognosis
Superinfections, where HDV infects someone with chronic HBV, have a poorer prognosis. The presence of chronic HBV provides a fertile ground for HDV to thrive, often leading to chronic hepatitis D. This can result in rapid progression to cirrhosis, liver failure, and liver cancer.
Factors Affecting Prognosis
Several factors can influence the prognosis of hepatitis D, including:
-
Age: Older individuals tend to have a poorer prognosis.
-
Overall Health: Individuals with other health conditions, such as HIV or hepatitis C, may have a worse prognosis.
-
Liver Function: The extent of liver damage at the time of diagnosis significantly affects the prognosis.
-
Treatment: Early and effective treatment can improve the prognosis.
Duration of Hepatitis D
The duration of hepatitis D depends on whether the infection is acute or chronic. Acute hepatitis D may last a few weeks to several months, while chronic hepatitis D can persist for years, often leading to long-term liver damage.
Acute Hepatitis D Duration: Acute hepatitis D typically lasts for a few weeks to several months. In co-infections, the immune system often clears both HBV and HDV, leading to recovery. However, in some cases, acute hepatitis D can progress to chronic hepatitis D.
Chronic Hepatitis D Duration: Chronic hepatitis D can persist for years, often leading to progressive liver damage. Without effective treatment, chronic hepatitis D can result in cirrhosis, liver failure, and liver cancer.
Hepatitis D Treatment and Medication
Currently, there is no cure for hepatitis D, but treatment focuses on managing symptoms, slowing disease progression, and preventing complications. Key treatment options include:
-
Pegylated Interferon Alpha: This is the most commonly used medication for hepatitis D. It helps reduce viral activity and liver inflammation.
-
Antiviral Therapy for HBV: Since HDV relies on HBV, controlling HBV can indirectly help manage HDV.
-
Liver Transplant: In cases of severe liver damage, a transplant may be the only option.
Research is ongoing to develop more effective treatments, including direct-acting antivirals specifically targeting HDV.
Pegylated Interferon Alpha
Pegylated interferon alpha is the primary treatment for hepatitis D. It works by boosting the immune system's ability to fight the virus and reducing liver inflammation. Treatment typically lasts for 48 weeks, but the response rate varies. Some individuals may achieve a sustained virological response (SVR), where the virus is undetectable in the blood after treatment.
Antiviral Therapy for HBV
Since HDV relies on HBV for replication, controlling HBV can indirectly help manage HDV. Antiviral medications, such as tenofovir or entecavir, are used to suppress HBV replication. However, these medications do not directly target HDV.
Liver Transplant
In cases of severe liver damage, a liver transplant may be the only option. This procedure entails transplanting a healthy liver from a donor to replace the impaired one. Liver transplantation can be life-saving, but it is a complex procedure with significant risks and challenges.
Emerging Treatments
Research is ongoing to develop more effective treatments for hepatitis D. Some promising approaches include:
-
Direct-Acting Antivirals: These medications specifically target HDV and are currently in clinical trials.
-
Gene Therapy: Experimental approaches aim to disrupt the replication of HDV using gene-editing technologies.
Complementary and Integrative Approaches
While medical treatment is essential, some patients explore complementary and integrative approaches to support liver health. These may include:
-
Dietary Changes: A balanced diet rich in fruits, vegetables, and whole grains can support liver function.
-
Herbal Supplements: Milk thistle and turmeric are popular for their potential liver-protective properties, though their efficacy is not scientifically proven.
-
Lifestyle Modifications: Avoiding alcohol, maintaining a healthy weight, and exercising regularly can help reduce liver stress.
Always consult a healthcare provider before trying any complementary therapies, as some may interact with medications.
Dietary Changes
A healthy diet can support liver function and overall health. Key dietary recommendations for individuals with hepatitis D include:
-
Fruits and Vegetables: Rich in antioxidants, which help protect liver cells from damage.
-
Whole Grains: Provide essential nutrients and fiber, supporting overall health.
-
Lean Proteins: Such as fish, poultry, and plant-based proteins, which are easier on the liver.
-
Healthy Fats: Such as those found in nuts, seeds, and olive oil, which support liver health.
Herbal Supplements
Some individuals with hepatitis D explore herbal supplements to support liver health. Popular options include:
-
Milk Thistle: Contains silymarin, which is believed to have liver-protective properties.
-
Turmeric: Contains curcumin, which has anti-inflammatory and antioxidant effects.
However, the efficacy of these supplements is not well-established, and they should be used with caution, especially in individuals with liver disease.
Lifestyle Modifications
Lifestyle changes can play a significant role in managing hepatitis D and supporting liver health. Key recommendations include:
-
Avoiding Alcohol: Consuming alcohol can worsen liver impairment and is best abstained from.
-
Maintaining a Healthy Weight: Obesity can contribute to liver damage, so maintaining a healthy weight is important.
-
Regular Exercise: Physical activity supports overall health and can help reduce liver stress.
Prevention of Hepatitis D
The best way to prevent hepatitis D is to prevent hepatitis B, since HDV cannot exist without HBV. Key prevention strategies include:
-
Vaccination: The hepatitis B vaccine is highly effective and provides indirect protection against HDV.
-
Safe Practices: Avoid sharing needles, practice safe sex, and ensure blood products are screened for HBV and HDV.
-
Education: Raising awareness about transmission risks is crucial, especially in high-risk populations.
Interestingly, efforts to prevent hepatitis C (another serious liver infection) also overlap with hepatitis D prevention, as both viruses share similar transmission routes.
Vaccination
The hepatitis B vaccine is the most effective way to prevent hepatitis D. The vaccine is typically given in a series of three doses and provides long-lasting protection against HBV. By preventing HBV, the vaccine indirectly protects against HDV.
Safe Practices
Implementing precautionary measures can greatly minimize the likelihood of HDV infection. Key recommendations include:
-
Avoiding Sharing Needles: Individuals who inject drugs should use sterile needles and avoid sharing equipment.
-
Practicing Safe Sex: Using condoms and limiting the number of sexual partners can reduce the risk of transmission.
-
Screening Blood Products: Ensuring that blood and organ donations are screened for HBV and HDV can prevent transmission.
Education and Awareness
Raising awareness about the risks of HDV and the importance of prevention is crucial, especially in high-risk populations. Education campaigns can help reduce stigma, promote vaccination, and encourage safe practices.
Complications of Hepatitis D
If left untreated, hepatitis D can lead to severe complications, including:
-
Cirrhosis: Scarring of the liver that impairs its function.
-
Liver Failure: Should the liver cease to perform its indispensable functions.
-
Hepatocellular Carcinoma: A type of liver cancer.
-
Fulminant Hepatitis: A rare but life-threatening condition characterized by sudden liver failure.
These complications highlight the importance of early diagnosis and treatment.
Cirrhosis
Cirrhosis represents an advanced phase of liver disorder marked by the substitution of normal liver tissue with fibrous scarring. This impairs the liver's ability to function properly and can lead to a range of complications, including:
-
Portal Hypertension: Increased blood pressure in the portal vein, which can cause varices (enlarged veins) and bleeding.
-
Ascites: Fluid accumulation in the abdomen, leading to swelling and discomfort.
-
Hepatic Encephalopathy: Brain dysfunction due to liver failure, resulting in confusion, memory loss, and cognitive impairment.
Liver Failure
Liver failure occurs when the liver is no longer able to perform its vital functions. This is a critical, potentially fatal situation that demands urgent medical intervention. Symptoms of liver failure include:
-
Jaundice: Yellowing of the skin and eyes.
-
Confusion and Coma: Due to hepatic encephalopathy.
-
Bleeding: Resulting from impaired production of clotting factors.
-
Multi-Organ Failure: As the liver fails, other organs may also be affected.
Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is a type of liver cancer that is more common in individuals with chronic hepatitis D. The risk of HCC is significantly higher in individuals with cirrhosis. Early detection and treatment are crucial for improving outcomes.
Fulminant Hepatitis
Fulminant hepatitis is a rare but life-threatening condition characterized by sudden liver failure. It can occur in acute hepatitis D and requires immediate medical intervention. Symptoms include:
-
Severe Jaundice: Rapid onset of yellowing of the skin and eyes.
-
Coagulopathy: Impaired blood clotting, leading to bleeding.
-
Encephalopathy: Rapid progression to confusion, coma, and death if untreated.
Conclusion
Hepatitis D is a complex and serious liver infection that thrives in the presence of hepatitis B. Understanding what hepatitis D is, its stages, symptoms, causes, and treatment options is crucial for managing the disease and improving outcomes. While there is no cure yet, advances in medical research offer hope for more effective treatments in the future.
Prevention remains the best strategy, particularly through hepatitis B vaccination and adopting safe practices to reduce transmission risks. If you or someone you know is at risk, seek medical advice promptly. Early intervention can make all the difference in preventing the severe complications associated with hepatitis D.
By staying informed and proactive, we can combat this silent but deadly virus and protect liver health for generations to come.
FAQ's
1. Is hepatitis D lifelong?
Yes, hepatitis D (HDV) can become a chronic, lifelong infection if it persists for more than 6 months. It only occurs in individuals who are already infected with hepatitis B (HBV), as HDV requires HBV to replicate.
2. Which hepatitis is not curable?
Chronic hepatitis B and hepatitis C are often not curable, but they can be managed with antiviral treatments. Hepatitis D, which depends on hepatitis B, is also not curable, though treatments can help manage symptoms.
3. What is the difference between hepatitis D and E?
-
Hepatitis D (HDV): A defective virus that requires hepatitis B virus (HBV) to replicate. It is transmitted through blood and bodily fluids and can cause severe liver damage.
-
Hepatitis E (HEV): A self-limiting virus transmitted primarily through contaminated water or food. It does not require another virus to replicate and usually resolves on its own.
4. What is hepatitis type D?
Hepatitis D (HDV) is a viral infection that affects the liver and only occurs in individuals who are already infected with hepatitis B (HBV). It can cause severe liver damage and is transmitted through blood or bodily fluids.
5. Is hepatitis E permanent?
No, hepatitis E (HEV) is usually an acute, self-limiting infection that resolves on its own within a few weeks. However, in rare cases, such as in pregnant women or individuals with weakened immune systems, it can become chronic or severe.
6. Is there a vaccine for hepatitis D?
No, there is no specific vaccine for hepatitis D. However, since HDV requires HBV to replicate, the hepatitis B vaccine can prevent HDV infection by preventing HBV.
7. What are the 7 types of hepatitis?
The 7 types of hepatitis are:
-
Hepatitis A (HAV)
-
Hepatitis B (HBV)
-
Hepatitis C (HCV)
-
Hepatitis D (HDV)
-
Hepatitis E (HEV)
-
Hepatitis F (HFV) – A hypothetical virus, not widely accepted.
-
Hepatitis G (HGV) – A virus with unclear clinical significance.
8. What if hepatitis E is positive?
A positive hepatitis E test indicates an active or past HEV infection. Most people recover without treatment, but if symptoms are severe or persistent, medical attention may be required, especially for pregnant women or immunocompromised individuals.
9. What is the best treatment for hepatitis E?
There is no specific antiviral treatment for hepatitis E. Management focuses on supportive care, such as rest, hydration, and proper nutrition. In severe cases, hospitalization may be required.
10. Is hepatitis E killed by cooking?
Yes, hepatitis E virus (HEV) can be killed by thorough cooking. Properly heating food to high temperatures and ensuring safe water practices can prevent HEV transmission.
11. Is hepatitis E life threatening?
In most cases, hepatitis E is not life-threatening and resolves on its own. However, it can be severe or fatal in certain populations, such as pregnant women (especially in the third trimester), individuals with pre-existing liver disease, or those with weakened immune systems.